
Highly trained workers can perform more visit-related tasks, boosting care quality and reducing physician burnout.
Fam Pract Manag. 2019;26(1):17-22
Author disclosure: no relevant financial affiliations disclosed.

Team-based care has become popular as the health care industry looks for new approaches to both deliver patient care and reimburse physicians.1 Many models are available, but we developed our own version of advanced team-based care built around the idea of providing physicians with substantial support, which we believe not only improves the care of our patients but also helps alleviate health care worker burnout.
Bellin Health is a community-based health care system serving northeastern Wisconsin and the upper peninsula of Michigan. We currently employ about 130 primary care physicians and advanced practice clinicians in our 30 clinics across the area. The system also includes two hospitals and a growing base of specialists.
Our model of team-based care has three main elements:
Total redesign of the office visit, including a greatly enhanced role for empowered certified medical assistants (CMAs) and licensed practical nurses (LPNs) who now close care gaps, review patient medication, and provide a key role working with the electronic health record (EHR) during visits.
A team approach to completing “in-basket” work performed between visits, including patient forms, lab results, medication refills, prior authorization requests, and other paperwork that usually falls to the physician. We do this by leveraging daily huddles and co-location — having team members work in close quarters to make communication more efficient. This element features an enhanced role for care team registered nurses (RNs), who provide both administrative services and direct patient care.
Development of an extended care team, including case managers, clinical pharmacists, diabetes educators, RN care coordinators, and others who support the care of our complex and high-risk patients.
This article will focus on the enhanced roles for the CMAs, LPNs, and RNs in our model and describe some of the ways we help these valuable team members become comfortable and efficient in their new roles.
KEY POINTS
Advanced team-based care uses well-trained certified medical assistants, licensed practical nurses, and registered nurses to take over more facets of the patient visit, freeing up time for the physician.
Care team coordinators run the daily morning huddle, do pre-visit planning, find and resolve patient care gaps, and handle electronic health record duties during the patient visit.
Registered nurses oversee blood pressure follow-ups, annual wellness visits, chronic care management services, and transitional care management services.
Even small practices can use advanced team-based care if they proceed slowly, find which parts work for them, and make sure new personnel generate sufficient revenue to make the model financially sustainable.
THE NEW OFFICE VISIT AND THE CARE TEAM COORDINATOR
Our team-based office visits feature the work of care team coordinators (CTCs). These are CMAs and LPNs who have received extensive training to take a lead role in the office visit, performing many tasks previously handled by the physician.
Our analysis determined that the optimal number of CTCs per physician or advanced practice clinician depended on the number of daily patients seen. (See “Care team coordinator staffing model.”)
| Number of daily patient visits per provider | Care team coordinator (CTC) to provider ratio |
|---|---|
| Fewer than 15 | One CTC per physician/provider |
| 15–19 | Three CTCs per two physicians/providers |
| 20 or more | Two CTCs per physician/provider |
CTC tasks. Each morning, the CTCs run brief daily huddles for their care teams — including the physician or advance practice clinician and, if available, the RN and team scheduler — to review that day's schedule and anticipate patient needs so the visits go smoothly. They also prepare for each visit by looking for gaps in that patient's care, such as missing immunizations.
Once the patient arrives, the CTC, as part of an expanded rooming process, will perform medication reconciliation, manage refills, and help the patient set the agenda for the visit. He or she may also pull up appropriate documentation templates in the EHR.
The biggest change comes during the visit itself, when the CTC stays in the room with the physician to provide documentation support and record pending orders as directed. This allows the physician to focus his or her time entirely on the patient.
After the physician's portion of the visit is complete, the CTC stays with the patient to review the changes recommended by the physician, schedule future labs or follow-up appointments, and go over the after-visit summary. Meanwhile, the physician leaves the exam room and goes to the team's co-location space to sign off on pended orders and review, edit, and approve the documentation entered by the CTC. There is evidence that the quality of notes completed by MAs is equal to or better than those written by physicians.2 (Note: Medicare has eased team documentation requirements starting in 2019, but check with your Medicare administrative contractor and other payers to ensure compliance with local policies regarding team documentation.) The patient's chart is usually closed before the physician moves on to the next patient, who is already in the next exam room with a second CTC. This eliminates the need to work on the EHR after hours or at home.
Training. CTCs require significant training to prepare for their enhanced roles. Our eight-week process uses weekly meetings of the care team (if the team is new to the process) or just the CTC (if that person is new to the role) to cover such things as change management, team culture, and the basics of population health and documentation. The CTCs also shadow existing teams to get a better understanding of their new roles. (See “Care Team Coordinator training schedule.”)
The week before the go-live date, the new CTC has three days of EHR training to learn about visit templates and the specifics of working with the EHR.
For the first two weeks after going live, the CTCs receive elbow-to-elbow support from experienced CTCs.
An implementation team of a change lead administrator, an RN, and two CTCs are responsible for much of this training. We perform sustainability audits after six months and periodically thereafter to ensure that the teams are continuing to use the new processes and workflows and do not slip back to the old ways of doing things.
We also encourage physicians to support the CTCs as they learn their new roles. With ongoing nurturing and positive feedback from the physician, most CTCs become comfortable in their new roles within the first few weeks.
CARE TEAM COORDINATOR TRAINING SCHEDULE
Weeks one through four
Standard training, including rooming procedures, clinical skills, basic life support training, job-specific skills, and electronic health record (EHR) basics.
Weeks five through eight
Team-based care training, including closing care gaps, pre-visit planning, team documentation basics, clinical documentation, team culture and change management, working with EHR templates, medication review and refills, setting the patient agenda, reviewing the after-visit summary, basic health coaching, and scheduling future appointments and labs.
Results. We introduced this model in a single location in 2014. By the end of 2018, we had spread the model to all of our primary care teams. We are now implementing this transformation with our other specialties, which face many of the same challenges as primary care.
We made the assessment early on that for this transformation to succeed, there had to be three wins — for the patient, for the care team, and for the health system.
On the patient side, there is nearly universal acceptance of the CTC. Our scripting allows the patient to opt out of having the CTC in the room, but this rarely happens. For one thing, patients have noticed that the physician can better focus on them during the visit with the CTC working on the computer in the exam room. The model also allows physicians to see more patients, which reduces wait times for appointments and further increases patient satisfaction. Almost 97 percent of patients using team-based care practices said they could get an appointment when they wanted one, compared with almost 71 percent before we implemented the new model.
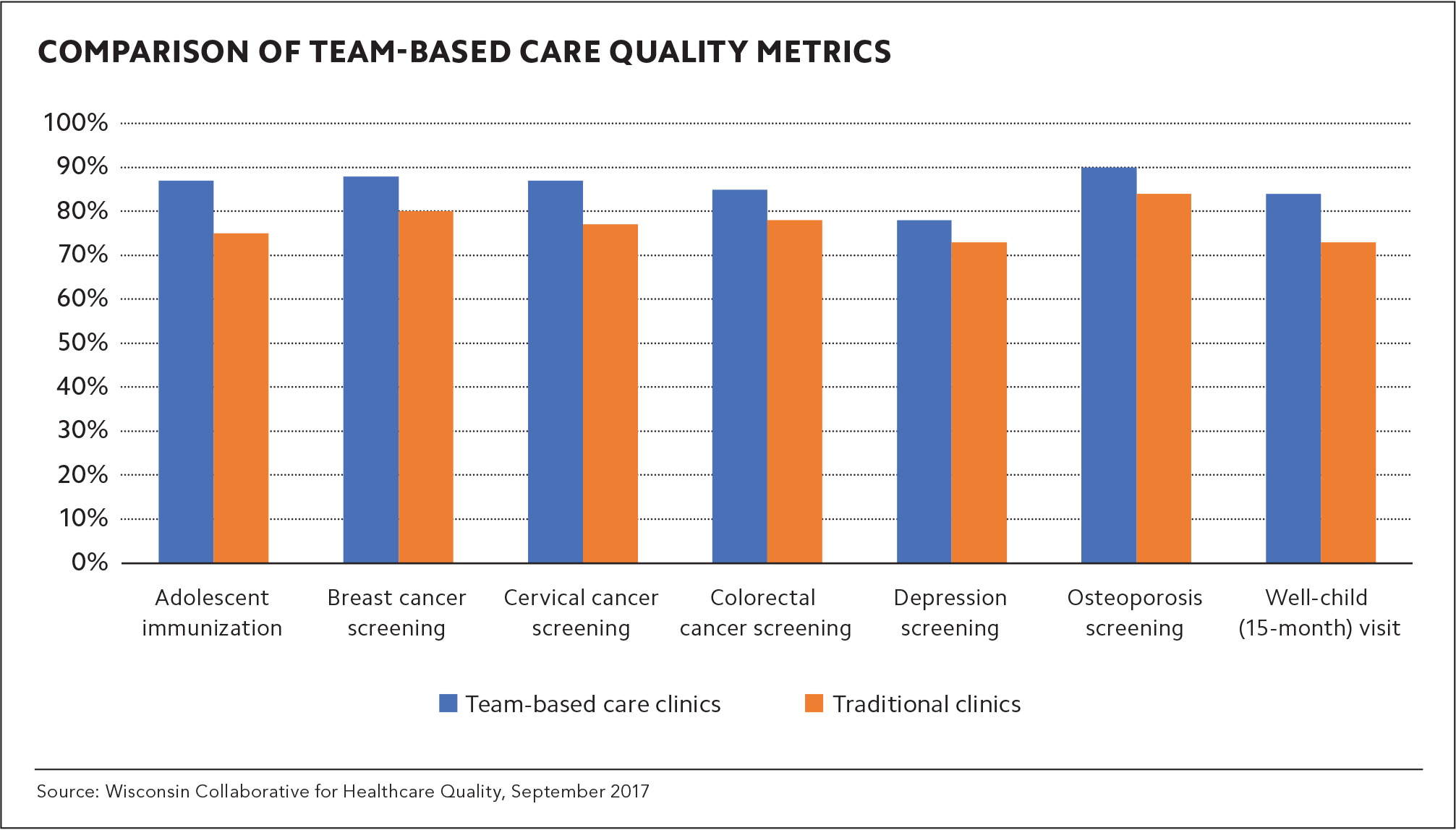
We have also seen significant improvement in care quality. Patients in practices using the new model have experienced, on average, an 8 percent gain in seven key quality metrics over one year when compared with patients whose physicians were not using the new model. (See “Comparison of team-based care quality metrics.”) We believe this improvement occurs because the entire team, not just the physician, is responsible for quality, and patients benefit from the CTCs' pre-visit planning and the use of standing orders and protocols to close care gaps. The CTCs have also developed meaningful relationships with their patients, which helps when the CTC calls them with results or to answer patient questions about their visit.
For the health system, the model allows physicians to see more patients, generate more revenue, and make the transformation financially sustainable. Also, the model produces cost savings as patients whose practices used the new model had a per member per month (PMPM) cost that was $27.12 lower than patients in more traditional practices. We believe these savings are due to our increase in preventive care, which reduces complications and hospital readmissions (down from 19.7 percent in 2016 to 6 percent in 2018 for patients with congestive heart failure).
Challenges. The chief hurdle for this transformation has been making sure the CTCs don't get overwhelmed by their new responsibilities, especially the documentation. Before training, most CTCs have little understanding of even the basic structure of a note. This is why our training begins with note fundamentals and expands from there. Still, not every CMA or LPN can make the transition. Some may not have the technical skills for the EHR work, and others are simply not a good fit for this enhanced role.
It can also be difficult to find enough CMAs to train as CTCs, which is one of the reasons we have also included LPNs. Once trained, there is the additional problem of turnover as CTCs feel more empowered in their new roles and may want additional training and advancement. At my clinic alone, we have had eight CTCs seek training as RNs. To deal with this attrition, we focus on recruiting new staff and have met with area technical colleges for assistance.
Lastly, physicians have not always been receptive to the transformation or fully engaged with team-based care, which can send mixed messages to team members. In our system, the physicians need to play a key role in nurturing and supporting CTCs. They cannot opt out of this transformation because the primary goal is to improve the health of our patient population. We have maintained some degree of flexibility to accommodate individual physicians, but that can make developing consistent processes and workflows difficult.
In the end, most physicians have embraced this model, which will likely help with recruitment as team-based care principles become more common in family medicine residency programs.3
THE ENHANCED CARE TEAM RN
The role of the RN in ambulatory settings is evolving.4 Outside of team-based care, the RN often is limited to triage and performing any tasks that lack clear workflows. Our system still involves some triage, but we have developed several other roles for our care team RNs.
They schedule and perform certain types of patient visits, such as blood pressure follow-ups and Medicare annual wellness visits (AWVs). Handling these visits frees up the physician to see more patients and improves quality by making sure these patient needs do not fall through the cracks. Our system completed AWVs for 76 percent of our eligible patients in 2018, well above a national rate of about 30 percent.5 The RNs can also use this time to provide in-depth patient education. We have found that patients with diabetes who are given a warm handoff from their physician to the RN and receive basic diabetes education are more engaged in managing their disease.
RNs also perform outreach for Medicare patients who are eligible for chronic care management (CCM) and transitional care management (TCM) services.
In addition, RNs serve as leaders on the care team, providing a valuable resource for the CTCs, facilitating the regular care team meetings, helping develop plans for improving quality measures, and discussing high-risk patients with the extended care team. They also provide oversight to our team-based approach to in-basket work, assisting when CTCs and physicians are too busy to address those items themselves.
We determined that one RN for every 3,000 patients with at least four to six billable patient visits a day was sustainable.
Training. As with the CTCs, training for the care team RNs starts several weeks before the go-live date and covers the same basic training in team-based care. Additional training includes motivational interviewing, which helps make RNs more effective in the significant face-to-face time they have with patients, as well as specific instruction on performing blood pressure visits, diabetes education and management, and CCM and TCM work-flows. RNs receive close support as they begin their new roles.
Results. The use of ambulatory RNs in team-based care models has been emerging in ways that increase financial sustainability. For example, RNs can bill 99211 for blood pressure visits with established patients. They can also perform Medicare wellness visits and CCM and TCM services under the supervision of a physician. Additionally, RNs' direct involvement in patient visits can help improve quality care measures for diabetes and blood pressure management.
Challenges. As with CTCs, RNs can become stressed by the number of new roles under this model, especially early on. Some RNs also may not be comfortable taking on an active role in patient care, especially if they have gotten used to their triage role.
Turnover among RNs in this role is a concern as well, and several RNs in our system have moved on to become nurse practitioners. We encourage this self-advancement and have adjusted our onboarding processes for new RNs accordingly.
As RNs and CTCs take on these new roles, it's important to establish standardized workflows and ongoing communication to avoid confusion about who is responsible for certain activities. For example, if a patient calls with questions about a recent visit, is it the responsibility of the CTC, the RN, or the physician to respond? Physicians may also question where to route patient emails or other in-basket items if these responsibilities are not clarified.
Physician acceptance of the new RN role is occasionally a challenge as some believe that the RNs cut into their potential relative value units (RVUs) and revenue by billing for blood pressure checks and AWVs. (We credit these RVUs internally, not to individual physicians.) However, most physicians embrace the new RN role and find no drop off in RVUs because the team's increased efficiency leads to improved patient access.
WHAT ABOUT SMALLER PRACTICES?
Bellin is an integrated health system with the resources to tackle this transformation in a comprehensive way. But even small practices can obtain some of the benefits from this model if they approach team-based care incrementally and figure out what works for them. We had no grant money for this project, so we had to be cautious with finances to ensure sustainability, just as a smaller practice would.
Adjusting your processes to allow non-physician clinical staff to address patient care gaps can help generate value-based payments based on quality measures. This is one of the reasons we used up-trained clinical staff instead of trained scribes for EHR support. Also consider involving ambulatory RNs in reimbursable visits.
To create additional capacity for physicians, work with your IT staff or vendors to streamline your in-basket work. Look for items that could be filtered, such as daily progress notes from hospitalists. Route every item to the staff members who can handle those items at the top of their skill set, and use a team approach to remove the pressure on physicians.8
In our experience, co-locating the team members in the same space is a critical part of successful team-based care. Verbal communication is always more efficient than electronic messaging. If you do not have co-location space, consider putting direct support staff in the same offices as physicians and advanced practice clinicians.
THE NEW WORLD OF ADVANCED TEAM-BASED CARE
Adopting team-based care requires time, commitment, and collaboration, but the effort enables practices to better manage their patient population's health while providing burnout relief for their health care workers. Seeing practices thriving in an advanced team-based care environment gives us confidence that this emerging model of health care delivery will enable us to fulfill the elements of the Quadruple Aim — improving the patient experience, improving the health of populations, reducing the per capita cost of health care, and improving the work-life balance for health care workers.9
