
Family physicians may encounter unfamiliar employment challenges in the short-term, but long-term job prospects remain promising.
Fam Pract Manag. 2021;28(1):11-16
Author disclosures: no relevant financial affiliations disclosed.
The coronavirus pandemic has had a profound effect on many aspects of health care, including the employment market for physicians. This article will explore how employment conditions for family physicians have changed as a result of COVID-19. It also will review current starting salaries, signing bonuses, and other features of physician employment contracts based largely on data from physician search firm Merritt Hawkins, with which we are affiliated.
HOW THE PHYSICIAN JOB MARKET HAS CHANGED
Prior to the pandemic, the employment market for family physicians and many other types of physicians had been robust. The challenge was not finding a job, but selecting the right one from among a plethora of choices. For example, in 2019, the majority (69%) of primary care residents in their last year of training received 51 or more recruiting offers, and almost half (46%) received more than 100 offers.1
Beginning in March 2020, the job market changed as the pandemic brought financial duress to physician practices, hospitals, and other entities that recruit and employ doctors.
By August 2020, 72% of physicians reported a reduction in income as a result of the pandemic.2 Of those, 55% experienced an income reduction of 26% or more.2 Additionally, 8% of physicians reported closing their practices as a result of COVID-19, a number that unfortunately is likely to grow as the pandemic continues. It is probable that many of the independent practices that cannot weather the COVID-19 storm alone will look to merge with hospitals or larger medical groups to survive. In addition, fewer physicians may be inclined to open private practices in this environment. That means a growing number of physicians will be looking to hospitals or hospital-owned medical groups for employment.
However, hospitals also have taken a financial hit. The American Hospital Association estimates that U.S. hospitals lost more than $323 billion from March through December 2020.3
As a result, the pace of physician hiring has slowed significantly. Many practices and hospitals have neither the patient volume nor the financial resources required to recruit additional physicians. Instead, some physicians have been furloughed and others laid off, something we have never observed in our 33 years of recruiting.
Today, rather than having many practice opportunities to choose from, residents and practicing physicians may have to compete to secure positions that meet their needs. In addition, when comparing opportunities, physicians may find greater differences in scope of practice, compensation, sites of care, and other factors than they would have found pre-pandemic. Physicians will need to weigh these differences against their immediate and longer-term requirements.
In a sign of the times, the number of physicians contacting Merritt Hawkins to inquire about practice opportunities or to respond to job postings has significantly increased since the pandemic began, while the number of employers initiating searches for physicians has declined. Family physicians seeking jobs are advised to be open-minded about accepting an offer early in the recruiting process if it meets most of their needs.
Most job interviews are now virtual, and physicians may have to make a decision without having visited the location and without having personally met the people they will be joining. The era of comparison shopping during the course of multiple job interviews over many months is temporarily on hold.
KEY POINTS
The COVID-19 pandemic has caused financial difficulties for physician practices, hospitals, and other organizations that recruit and employ doctors, leading to a challenging job market.
While demand for family physicians has declined compared with previous years, long-term job prospects remain favorable.
Family physicians can expect their employment contracts to include stalled starting salaries, mostly volume-based production bonuses, modest signing bonuses, and relocation and CME allowances.
TRENDS AFFECTING DEMAND FOR FAMILY PHYSICIANS
Each year, Merritt Hawkins releases its Review of Physician and Advanced Practitioner Recruiting Incentives, examining the salaries, signing bonuses, and other incentives that hospitals and medical groups offer when recruiting physicians. The 2020 review is based on data from 3,251 search engagements conducted nationwide and reflects the types of physicians that employers are seeking. For the 14th consecutive year, family medicine was the most requested search engagement.4
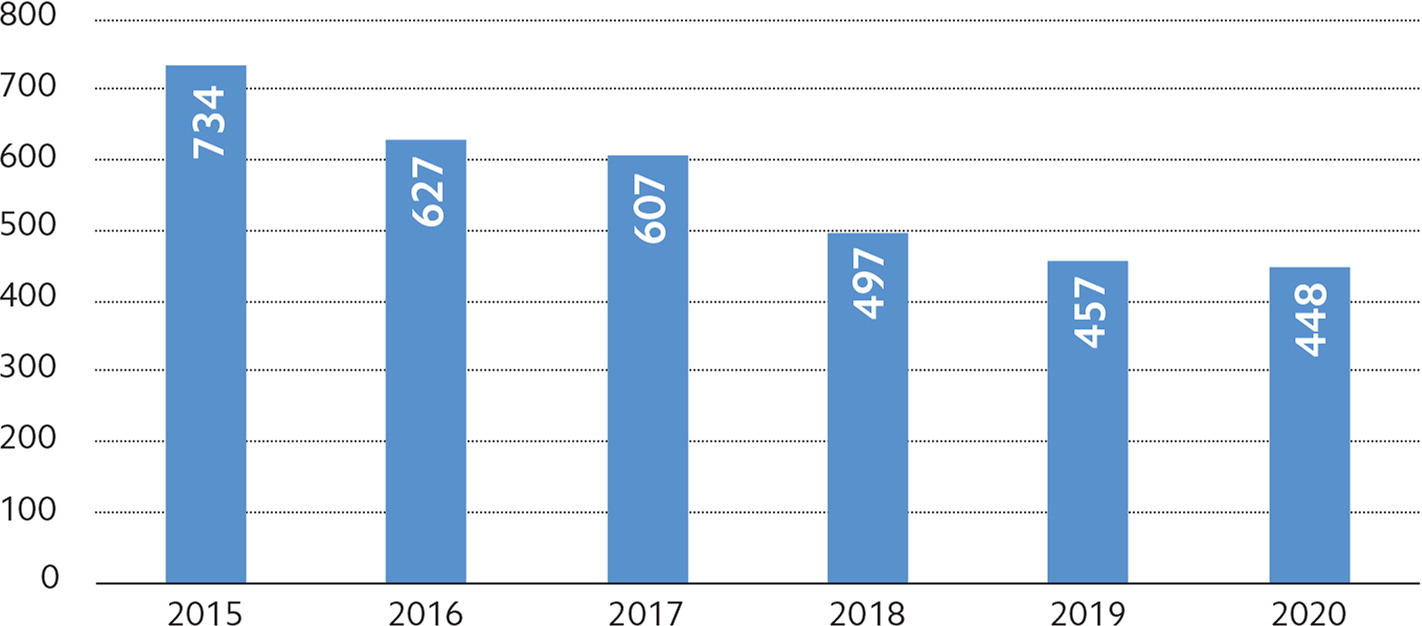
However, demand for family physicians has declined in recent years, even pre-COVID-19. In 2015, Merritt Hawkins conducted a record-high 734 family medicine searches. That number fell to 448 searches in 2020, a decrease of almost 40%.4 (See “Family medicine search assignments by year.”)
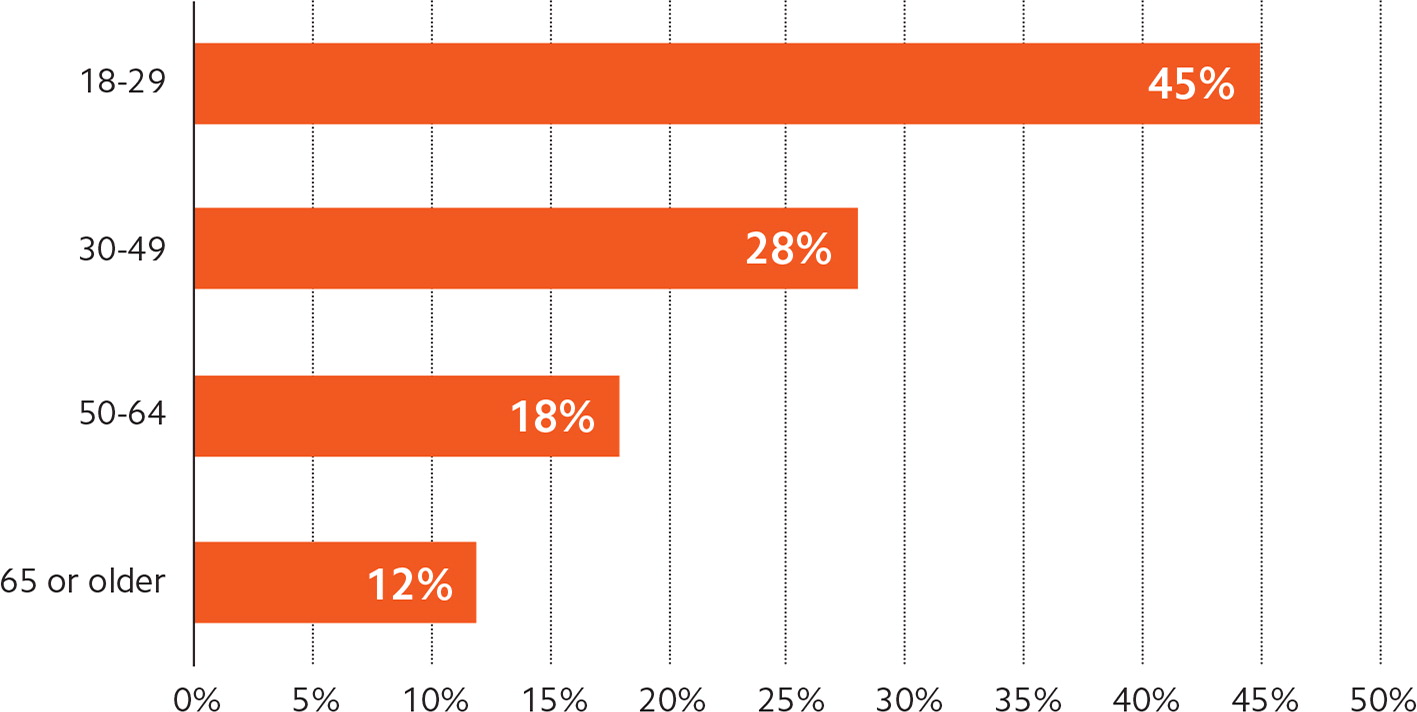
One reason for this shift is that some patients appear to be turning away from the traditional office-based primary care model. According to an October 2018 report from the Health Care Cost Institute, visits to primary care physicians dropped 18% from 2012 to 2016.5 In 2012, 51% of office visits for patients under 65 were to primary care physicians. That percentage declined to 43% in 2016, according to the report. Young people, in particular, appear less inclined to see a primary care physician than older people. (See “Adults who have no primary care physician by age range.”)
The same report found a 129% increase in office visits to nurse practitioners (NPs) and physician assistants (PAs) from 2012 to 2016. This is likely due to the rise in convenient care venues such as urgent care centers, retail clinics, and telemedicine companies. These are commonly staffed by NPs and PAs, and are becoming key entry points into the health system, particularly for young people.
Primary care physicians' widespread adoption of telemedicine during the pandemic could help reverse this trend. Assuming reimbursement and regulatory policies that allow for the expanded use of telemedicine remain in place, office-based family medicine practices that offer tele-medicine will be better able to compete with urgent care centers and other venues on convenience, thereby attracting younger patients, such as millennials, who embrace convenience. Older patients who have been exposed to telemedicine as a result of the pandemic also are showing a preference for this delivery model. This could create additional job opportunities for family physicians while providing patients with the continuity of care they gain from having a primary care physician.
As the population ages, demand for primary care physicians could also increase because of their critical role in care coordination of older patients, many of whom have multiple chronic illnesses that need to be tracked and managed. It is largely due to population aging that the Association of American Medical Colleges (AAMC) projects a shortage of up to 139,000 physicians — including up to 55,200 primary care physicians — by 2033.6
Primary care physicians also are essential to the implementation of value-based reimbursement models and to the integrated systems built on these models, such as accountable care organizations (ACOs). In these models, primary care physicians are the quarterbacks of the care delivery team, ensuring tasks are allocated appropriately and resources are managed efficiently. The principles of value-based care and population health management cannot be applied without a robust network of primary care doctors.
WHAT TO EXPECT IN AN EMPLOYMENT CONTRACT
Given the changing job market and future trends, here's what family physicians can expect to see in their employment contracts.
Starting salaries. Average starting salary offers made to family medicine physicians grew from $185,000 in 2013 to $241,000 in 2018, an increase of 30%, as tracked by previous reviews from Merritt Hawkins. However, the 2020 review indicates that starting salaries for family physicians have remained flat at around $240,000 over the last two years,4 another sign that demand for family physicians has abated somewhat. (See “Starting salaries for family physicians.”)
How the COVID-19 pandemic affects starting salaries for family physicians going forward will depend on how quickly the economy recovers and how quickly patient confidence in seeking health care is restored. This is likely to vary by region.
Salary growth also will depend on tele-medicine regulatory and reimbursement policies. If telehealth visits ultimately are reimbursed at roughly in-person rates, making them a viable alternative to in-person visits, family physicians should be able to generate the volume necessary to earn productivity bonuses and generate additional downstream revenue for their affiliated hospitals, which would eventually increase starting salary offers. In the short-term, however, starting salary offers in family medicine can be expected to stay flat or decrease slightly as utilization stays low and new delivery models like telemedicine are implemented.
| Low | Average | High | |
|---|---|---|---|
| 2020 | $140,000 | $240,000 | $325,000 |
| 2019 | $130,000 | $239,000 | $400,000 |
| 2018 | $165,000 | $241,000 | $400,000 |
Production bonuses. Typically, family physicians are offered employment contracts that feature a starting base salary that can be supplemented through a production bonus; 72% of Merritt Hawkins' search engagements featured this type of contract structure.4 An additional 25% featured a straight salary, while less than 1% featured an income guarantee.4
Salaries with production bonuses are commonly offered by hospitals and medical groups, whereas the straight salary model is more frequently used by urgent care centers, federally qualified health centers (FQHCs), and academic settings. Income guarantees, which are essentially loans physicians must repay (but that may be forgiven over time), generally are used to establish physicians in solo or small independent practices. Income guarantees were once the standard — when private practices were more prevalent than they are now — but they are rarely used today.
Production bonuses determine the maximum income physicians can potentially earn beyond their base salary. These bonuses are calculated using a variety of metrics, including the following:
Relative value units (RVUs),
Net collections,
Gross billings,
Patient encounters,
Quality.
All of these, with the exception of quality, are volume-driven metrics. Today, RVUs are the primary way employers measure physician productivity. The more RVUs family physicians generate by seeing more patients or providing more complex visits, the more net reimbursement they collect or gross billings they generate, and the higher their bonus. RVUs are featured in 73% of physician employment contracts offering a salary and production bonus. 4 The widespread use of RVUs highlights the extent to which physician compensation remains volume-based, although this is changing.
In order to evolve from the fee-for-volume model, ACOs, hospitals, medical groups, and other organizations are striving to create physician payment structures that reward doctors for providing value. Value may be measured through a number of metrics, including the following:
Quality/value-based physician compensation metrics,
Patient satisfaction scores,
Adherence to treatment/quality protocols,
Reduction of hospital readmissions/errors,
Group governance participation,
Cost reduction/containment,
Appropriate coding,
Implementation/use of EHRs.
According to our 2020 review, 64% of contracts that featured a production bonus included quality as one of the metrics, up from 56% the previous year and up from 23% in the 2015.4 This indicates that quality is becoming a more common determinant of physician production bonus amounts, but does not address the question of how much of total physician compensation is tied to quality.
The 2020 review tracks this amount directly, as did the two prior reviews. In instances where the production bonus includes quality metrics, an average of 11% of the physician's total compensation will be determined by quality. This percentage was the same in 2019 and was 8% in 2017.4 The majority of income for physicians, therefore, is still determined by their base salary plus volume-driven production bonuses.
COVID-19 and the pivot toward telehealth is likely to change how physician productivity and quality are measured. Assuming that recently expanded reimbursement for telehealth remains close to in-office rates, health care systems and other employers are likely to measure physician telehealth production through a patient encounter or RVU system, most likely the latter. They may also create production metrics around telehealth service quality, such as number of repeat telehealth patients or patient satisfaction reviews conducted through an automated system.
It will likely take delivery systems several quarters, if not several years, to develop the appropriate mix of incentives to reward desired physician behaviors in a manner that reflects strategic goals. Consequently, physicians need to be careful when entering into evergreen contracts or employment agreements with set baselines/averages that might become punitive over time. In addition, physicians should enter into agreements with some level of adaptation expected over the next few years, as market forces remain unstable.
Signing bonuses. Signing bonuses were offered in 72% of the recruiting assignments Merritt Hawkins conducted in the 2020 review period, up slightly from 71% percent the previous year.4 Signing bonuses offered to all physicians averaged $27,893, down from $32,692 the previous year.4 For family physicians, signing bonuses averaged $25,100, with a low of $2,500 and a high of $75,000.
Signing bonuses remain a standard recruiting incentive among hospitals and medical groups, but they may not be part of incentive packages offered by academic medical centers, direct pay/concierge clinics, urgent care centers, FQHCs, Indian Health Service centers, and other settings.
Relocation, CME, and other allowances. Incentives such as paid relocation, paid continuing medical education (CME), health insurance, and malpractice insurance are usually standard in physician employment contracts.
The average relocation allowance offered to physicians was $10,553.4 There typically is little difference in relocation bonus amounts based on specialty.
Medical education loan repayment. Educational loan repayment entails payment of the physician's medical school loans by the recruiting hospital or another entity in exchange for a commitment to stay in the community for a given period of time. This can be an effective incentive given that average medical school debt now exceeds $190,000.7
Only 24% of Merritt Hawkins' search engagements tracked in the 2020 review featured medical education loan repayment, compared with 31% the previous year.4 The average amount of loan forgiveness offered to physicians was $101,590, which is virtually unchanged from the previous year.4 In contracts featuring educational loan forgiveness, 9% required a one-year commitment, 24% required a two-year commitment, and 67% featured a three-year commitment.
Due to the pandemic, the use of loan forgiveness as an incentive may decline slightly in the short-term as employers are likely to have more candidates to choose from who no longer carry educational debt.
A CHALLENGING PRESENT BUT ROBUST FUTURE
The coronavirus pandemic has dramatically reduced employment opportunities for family medicine physicians and is likely to suppress starting salaries and production bonus potential in the short term. Family physicians currently seeking job opportunities should adjust their expectations and job-seeking strategies accordingly.
However, an aging patient population, the adoption of telehealth, and the key role family physicians play in value-based delivery models ensure the job market for family physicians will be robust in the long term.
