Am Fam Physician. 1998;57(6):1314-1322
This is Part II of a two-part article on pitfalls in the radiologic evaluation of extremity trauma. Part I, “The Upper Extremity,” appeared in the March 1 issue (Am Fam Physician 1998;57:995–1002).
Fractures of the lower extremity are common reasons for visits to family physicians. Some lower extremity fractures are especially likely to be missed. Examples of lesions that commonly go unrecognized include sacral insufficiency or fatigue fracture, fracture of the femoral neck (especially if the fracture is nondisplaced and/or impacted), tibial plateau fracture, Segond fracture (vertical fracture of the lateral tibia), patellar fracture, calcaneal fracture of the foot, Lisfranc fracture/dislocation of the tarsometatarsal apparatus, and Jones fracture of the fifth metatarsal. Lower extremity fracture in children may suggest the possibility of child abuse, especially in the case of multiple or bilateral fractures.
Just as in cases of fracture of the upper limb, plain radiographs remain important diagnostic tools in the initial assessment of patients with suspected fracture or dislocation of the lower limb. This article reviews key diagnostic features and mechanisms of injury, plain-film signs and advanced imaging techniques that may be used for further evaluation.
Pelvic Girdle
The normal sacrum seldom sustains an isolated fracture. Rather, sacral fractures usually occur in combination with other fractures of the pelvic girdle following a major force. Injury to the pelvic organs is often associated with sacral fractures. Plain film assessment of the sacrum and coccyx is often difficult because of the curved configuration and overlying bowel, which obscures bony detail. Routine anteroposterior and lateral views may be supplemented by images obtained with 15 degrees of cephalad angulation.
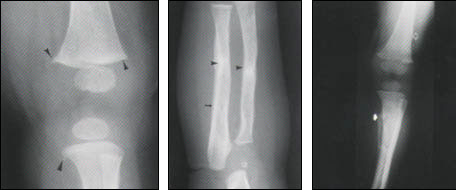
Sacral pathology may occur in the form of an insufficiency stress fracture. Insufficiency fractures of the sacrum typically occur in post-menopausal, osteoporotic women or in patients taking long-term corticosteroid treatments, those with rheumatoid arthritis or those who have undergone radiation therapy. Insufficiency fractures occur when abnormal bone (bone with decreased elastic resistance) is subject to normal stress. This is in contrast to the fatigue fracture, in which a fracture occurs in normal bone (bone with normal elastic resistance) that has been subject to abnormal stresses. Plain radiographs often appear normal in these cases. Irregularity of the contour or an actual break in the sacral arcuate lines and/or patchy sclerosis in an H-shaped configuration may be seen. This type of fracture is better demonstrated by bone scintigraphy, which reveals the characteristic “H” or “Honda” sign that appears as a result of intense radiopharmaceutical uptake, or by computed tomographic (CT) scanning (Figure 1).
Sacral insufficiency fractures also may occur in conjunction with insufficiency fractures at other sites. Fractures that involve the pubic rami may have a particularly aggressive appearance that is due to patchy areas of sclerosis, lysis and fragmentation, simulating a bone tumor. Stress fractures in patients with osteoporosis may also involve the symphysis pubis, supra-acetabular region, femoral neck, tibial plateau, proximal and distal tibia, sternum and ribs1 (Figure 2).
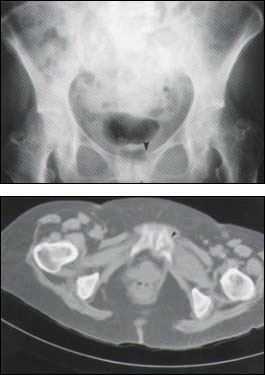
The anterior arch of the pelvis is significantly weaker than the posterior arch, so fractures of the pubic rami and symphysis are not uncommon and may be extremely difficult to identify on anteroposterior pelvic radiographs. These fractures tend not to be widely displaced. They may be impacted and, thus, seen only as a subtle, minor irregularity of the cortical margin or a region of sclerosis. If widely displaced, a thorough search for a second fracture is mandatory and must include evaluation of the sacroiliac joints and symphysis pubis. Fractures of the base of the pubis may also involve the acetabulum.
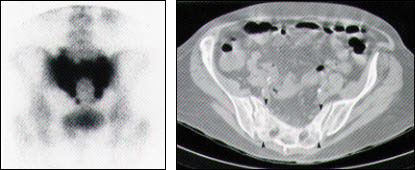
Fatigue fractures have been described in military personnel and athletes at all fitness levels. Usually, patients present with pain and localized tenderness, with a history of either an increase in activity or an alteration in the pattern of exercise. However, these fractures also occur in association with an alteration in gait or an imbalance in muscular force associated with either an ipsilateral or a contralateral injury, casting or surgery. Symptoms are typically relieved by rest. Fatigue fractures most commonly involve the bones of the lower limb. These fractures usually involve the tibial diaphysis in runners; the metatarsals in soldiers, ballet dancers and patients who have undergone bunionectomy; the tarsal navicular in soldiers and runners; the calcaneus in jumpers, parachuters and patients who have undergone immobilization; the patella in hurdlers; and the obturator ring in bowlers and gymnasts2 (Figure 3).
Multiple stress fractures are less frequent.3 Although a horizontal orientation is typically demonstrated, longitudinally oriented stress fractures are becoming more common.4 These longitudinal stress fractures usually occur in slightly older patients and almost exclusively involve the tibial shaft (Figure 4). Most cases of the classic, horizontally oriented stress fracture and the longitudinal stress fracture cannot be seen on plain radiographic films until weeks after the onset of symptoms. This often results in a delay in diagnosis and, consequently, a delay in the institution of appropriate treatment. Over time, radiographs may demonstrate a subtle increase in bone reaction along the outer cortex of the involved bone, with the subsequent development of linear sclerosis and new bone formation. The investigation of choice is scintigraphy, which shows a linear area of increased radionuclide uptake at the fracture site. However, with their higher spatial resolution, CT scan and magnetic resonance imaging (MRI) increasingly are being chosen to investigate stress fractures.

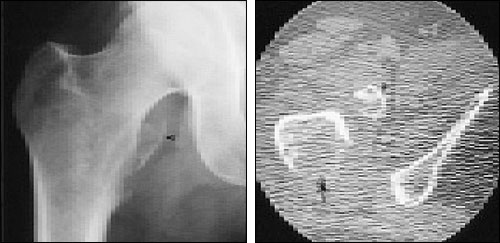
Femoral Neck
The femoral neck is best assessed on the anteroposterior view, with the leg in internal rotation. The hip joint is rarely widened by a hemarthrosis, but when widening is seen following trauma, it suggests the presence of an entrapped osteochondral fragment.
Proximal femoral fractures may be either intracapsular or extracapsular.5 Intracapsular fractures include the subcapital and transcervical types. These types occur twice as often as extracapsular fractures. The Garden system of classification of intracapsular fractures is based on the degree of displacement on prereduction radiographs.
Impacted, undisplaced or incomplete femoral neck fractures may be virtually impossible to detect radiographically. The history of trauma may be minimal. Diagnosis of this injury is further complicated because the impacted femoral neck fracture does not produce a limb deformity, the patient is able to raise and rotate the straight leg actively, and passive hip motion is painless. Accurate diagnosis is important, since the prognosis of this fracture is influenced by the degree of displacement. MRI is strongly advocated by many as the diagnostic procedure of choice because its multiplanar capabilities and high spatial resolution enable immediate detection of the fracture line. In addition, MRI is specific and can suggest alternate diagnoses.
Fractures of the femoral neck may interfere with the blood supply to the femoral head and neck by kinking or disrupting the epiphyseal arteries as they course along the superolateral aspect of the femoral neck. Thus, delayed union or nonunion occurs in 5 to 25 percent of intracapsular femoral fractures. The likelihood of union is also influenced by the degree of obliquity of the fracture line. The incidence of nonunion increases with increasing degrees of obliquity, as the shear force across the fracture is higher. As a consequence, reduction becomes increasingly difficult to maintain.
The extracapsular fractures include the basicervical and trochanteric types. Trochanteric fractures can be further subclassified into intertrochanteric and subtrochanteric. Correct radiographic diagnosis is important because these fracture types require entirely different treatment plans and have different prognoses. The excellent blood supply and the large surface area of cancellous bone virtually ensure healing of femoral neck fractures. The degree of comminution of the intertrochanteric fracture determines the method of reduction and fixation.
Isolated fractures of the lesser trochanter are rare in adults and usually represent the initial manifestation of skeletal metastatic disease (Figure 5).
Knee
Plain film imaging options for assessment of the knee include the anteroposterior and lateral views, the sunrise view and the notch, or tunnel, view. Assessment of the weight-bearing surfaces of the tibiofemoral joint space is obtained from the anteroposterior film. The notch view demonstrates the posterior aspect of the femoral condyles and enables evaluation of the tibial spines and the intercondylar notch. The lateral view is used to evaluate the soft tissues, particularly the extensor mechanism, and to define the presence of joint effusion. Joint effusion is manifested as loss of the clear plane of demarcation between the quadriceps tendon and the suprapatellar fat pad, with an ovoid density filling in the normal space. A lipohemarthrosis is evidenced by a fat-fluid level on a cross-table lateral view with a horizontal beam. This finding indicates an intra-articular fracture in which marrow fat and blood are extruded into the joint. In children, this injury is likely to be caused by a Salter Harris III fracture of the distal femur, but in adults it is usually attributable to a fracture of the tibial plateau.
Segond fracture suggests the presence of significant, but often radiographically occult, pathology. A small, vertically oriented, avulsed bony fragment involving the lateral aspect of the proximal lateral tibia is nearly always associated with a tear of the anterior cruciate ligament in the older population. Alternatively, an avulsion of the tibial spines is seen in younger patients6 (Figures 6 and 7).
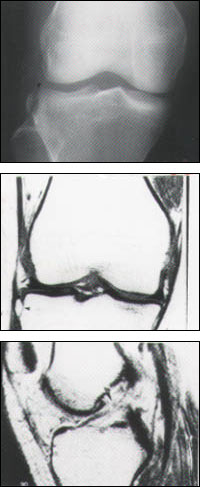
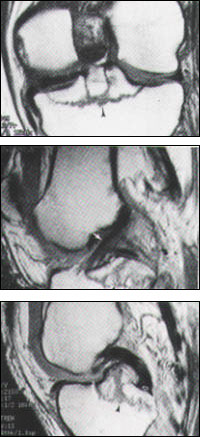
Fractures of the tibial plateau may also be radiographically subtle. Most are the result of a twisting injury from a fall, although these injuries also occur in pedestrians involved in motor vehicle accidents. More than one half occur in patients over 50 years of age, and 80 percent involve the lateral plateau as a result of a valgus stress. Oblique films are often useful in clarifying suspected plateau pathology. Radiographs typically demonstrate a vertical split extending from the joint margin, linear sclerosis below the joint line and depression of the articular surface (Figure 8). Historically, anteroposterior tomography and scintigraphy have been used to make the diagnosis, although MRI is extremely useful in the detection of occult fractures and in the demonstration of associated internal derangement. CT scanning is ideal for assessing the extent of bony involvement and evaluating the degree of depression of the articular surface, which is important in determining management options.
Patellar fractures occur with direct and indirect trauma, such as explosive quadriceps contraction. These fractures are often difficult to demonstrate and are best visualized on lateral and sunrise views. Fifty to 80 percent of patellar fractures are transverse, although they may be longitudinal when associated with a direct force. It is important to exclude a bipartite or tripartite patella as the cause of osseous fragments adjacent to the patella.7 This normal variant is typically (although not exclusively) seen as apparent patellar fragmentation with the smaller components lying over the superolateral aspect of the patella. It is bilateral in up to 75 percent of cases. The margins of the fragments are sclerotic and rounded, and do not fit together perfectly. In contrast, patellar fracture fragments have nonsclerotic, sharp margins and would fit perfectly together.
Foot
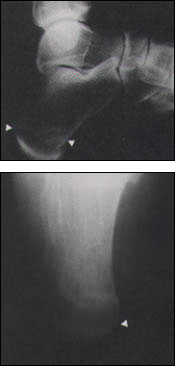
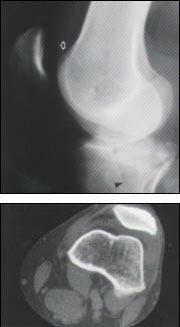
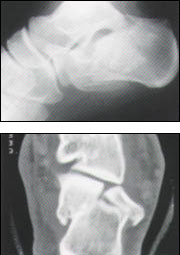
The calcaneus is the most commonly fractured tarsal bone. Typically the result of a fall from a height, calcaneal fractures are bilateral in 10 percent of cases and associated with compression fractures of the vertebral bodies in 10 percent. Plain radiographs are commonly diagnostic. CT scanning, however, is the imaging modality of choice to evaluate the extent of the injury. CT scans also provide an indication of the long-term outlook and assist in preoperative planning by defining the involvement of the articular surfaces and the degree of comminution, and allowing evaluation of the peroneal tendon for entrapment between the fibula and the calcaneus. Intra-articular fractures occur in 75 percent of cases and are associated with a poorer prognosis (Figure 9).
Intra-articular fractures that are not reduced anatomically result in incongruity of the articular surfaces and, subsequently, osteoarthritis. Lisfranc fracture–dislocations represent fracture-dislocations of the metatarsals (usually the second to fifth metatarsals) at the tarso-metatarsal joint. Although historically associated with trauma, they are also associated with a neuropathic (Charcot) foot that is related to diabetes mellitus or other neuropathy. Diagnosis of these fractures can be difficult and, thus, meticulous attention must be given to the normal anatomic relationships to avoid misdiagnosis. Normally, on anteroposterior radiographs, the lateral aspect of the base of the first metatarsal aligns with the lateral border of the medial cuneiform, and the medial border of the second metatarsal aligns with the medial border of the middle cuneiform. On oblique films, the lateral border of the third metatarsal aligns with the lateral border of the lateral cuneiform, and the medial border of the fourth metatarsal aligns with the medial border of the cuboid. The base of the fifth metatarsal articulates with the cuboid; however, it normally extends laterally to its lateral border. The second metatarsal base is recessed between the medial and lateral cuneiform, providing extra stability to the Lisfranc joint. These fracture-dislocations may be either homolateral or divergent. The homolateral fracture-dislocation, in which the first or second to fifth metatarsals all dislocate dorsally and laterally, is more common than the divergent fracture-dislocation, in which the first metatarsal subluxes medially, while the second, third, fourth and fifth metatarsals dislocate laterally (Figure 10).
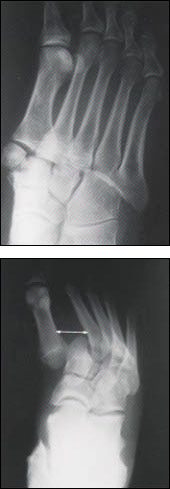
The Jones fracture is a transverse fracture of the proximal shaft of the fifth metatarsal. It has important prognostic implications and must be differentiated from an avulsion fracture of the fifth metatarsal tuberosity and the normal fifth metatarsal apophysis. The Jones fracture is relatively common. It may present as ankle pain rather than foot pain and usually results from an inversion injury. This fracture is associated with a high incidence of delayed union or nonunion and refracture. In skeletally immature patients, the apophysis is differentiated since it is longitudinally oriented, it does not enter the cuboid-metatarsal joint space, and it may be bipartite (Figure 11).

Child Abuse
Members of the medical profession are legally required to report findings that are suspicious for child abuse. Diagnosis is of paramount importance in order to protect the child and other siblings from further injury. Radiographically demonstrable skeletal abnormalities will be seen in 20 to 40 percent of abused children, although few radiographic findings are pathognomonic.
Radiologic findings inconsistent with the stated history or signs suggesting a delay in seeking medical care should alert the physician. The humerus, femur, tibia, skull and small bones of the hands and feet are the bones most commonly involved. However, fractures occurring in unusual locations, such as the posterior ribs, the vertebrae, the sternum and the long bones in infants not yet walking, should arouse suspicion. Multiple fractures, involvement of both sides of the body or fractures in various stages of healing raise the possibility of nonaccidental injury. Exuberant callus formation is also suggestive, although infantile cortical hyperostosis has similar appearances. Acute metaphyseal corner fractures are usually only seen in nonaccidental injuries, unless associated with the rare Menkes' kinky-hair syndrome, which is related to copper deficiency. Periostitis is a delayed radiographic finding of nonaccidental injury. However, periostitis may be normal during infancy. It is also seen in patients with Caffey's disease, infection and osteogenesis imperfecta (Figure 12).