
Am Fam Physician. 1998;58(4):891-898
A more recent article on newborn circumcision techniques is available.
Circumcision performed using the Gomco clamp is usually quick and effective, and results in very little bleeding. However, every clinician performing circumcision occasionally has concerns or questions regarding the procedure. Some of the more common concerns regarding the use of the Gomco clamp are technique-related, including choosing the correct size of the Gomco bell and clamp for the procedure, choosing the right method of getting the foreskin properly through the hole of the Gomco base plate, and assessing how much foreskin to remove. Other concerns include poor cosmetic results, contraindications to routine circumcision, and circumcision in an infant whose mother has human immunodeficiency virus. This article reviews the technique of circumcision using the Gomco clamp and answers some of the more common questions.
The Gomco clamp has become one of the leading instruments used in the performance of non-ritual circumcision in the United States. This device is popular because of its safety record in preventing injury and bleeding.
Technique
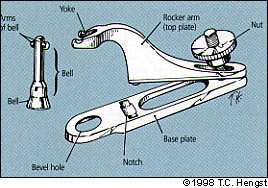
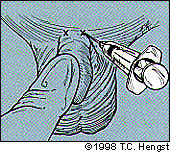
The procedure can be started after informed consent is obtained from the parents and the infant is properly identified. After the infant is restrained, the penis, scrotum and groin area are cleaned with a disinfecting solution and are inspected for anatomic abnormalities (Figure 1). The Gomco clamp is checked to make sure the bell is the right size for the clamp and that there are no defects (Figure 2). The area is prepped and a dorsal penile nerve block is administered, if desired (Figure 3a and 3b), unless a topical anesthetic cream (such as 2.5 percent prilocaine and 2.5 percent lidocaine [Emla]) has been used. A drape is used if desired.
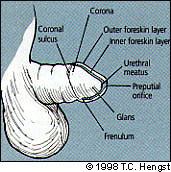
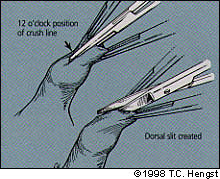
The foreskin is grasped on either side of the midline with two hemostats, taking care to avoid the urethral meatus, and a third hemostat or other instrument is carefully inserted into the preputial ring down to the level of the corona. The instrument should be used to tent the foreskin away from the glans to avoid the urethral meatus. The hemostat is swept around the glans on both the right and left sides, avoiding the ventral frenulum. This separates most of the adhesions between the inner mucosal layer and the glans. The hemostat is removed and is then used to create a crush line on the dorsal aspect not closer than 1 cm to the coronal sulcus in the foreskin. The crushed skin is cut with blunt scissors, taking care to avoid the glans (Figure 4a).
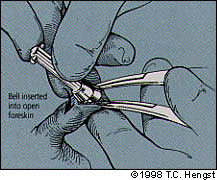
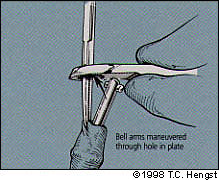
The foreskin is then retracted proximally using the hemostats, exposing the glans. Any remaining adhesions are bluntly divided using a blunt probe or gauze until the entire coronal sulcus is visible. Care should be taken to avoid the ventral frenulum to prevent bleeding. The foreskin is then drawn over the glans, and the bell of the Gomco clamp is inserted over the glans (Figure 4b). Several methods to pull the foreskin through the hole of the base plate around the bell are described later in this article. The stem of the bell is then maneuvered through the hole along with the foreskin after the amount of foreskin to be removed has been determined (Figure 4c). The amount of remaining shaft skin is evaluated and may be adjusted for length and symmetry (Figure 4d).
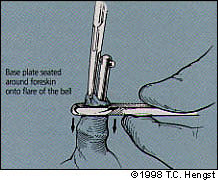
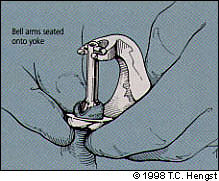
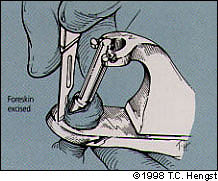
The rocker arm (top plate) of the Gomco clamp is then attached (if this has not been done previously) and brought around into the notch of the base plate. The arms of the bell are settled into the yoke, and the nut is tightened, crushing the foreskin between the bell and the base plate (Figure 4e). A scalpel is then used to excise the foreskin at the level of the base plate (Figure 4f). The nut is then loosened, and the top and base plate are removed from the bell. The shaft skin is then eased off the bell at the line of incision using a gauze with mild traction, to take its place below the corona.
The penis should be inspected following the procedure for signs of bleeding, with special attention to the ventral frenulum region. A dressing of petroleum jelly or petroleum gauze should be gently applied. The parents should be counseled about the healing process. Gentle retraction of the shaft skin may be necessary if it encroaches on the glans. Petroleum jelly may be applied liberally at diaper changes until the glans re-epithelializes.
Answers to Frequently Asked Questions
1. Is routine circumcision contraindicated in some male infants?
Several anatomic variations or abnormalities prohibit routine circumcision without proper consultation with a urologist. They include hypospadias, epispadias, megaurethra or abnormally short penile shaft (Figure 5). If, when placing the index and middle finger at the base of the penis and pushing down, there is less than 1 cm of penile shaft visible, then a Gomco circumcision should not be performed. Careful inspection of the infant's anatomy is important before beginning the procedure.
Circumcision in infants who are ill or premature should be delayed until they are well or ready for discharge from the hospital.
2. Should a dorsal penile nerve block be used?
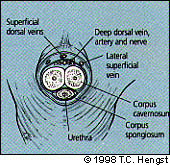
The dorsal penile nerve block was first described in 1978.1 Since then, more than 2,000 newborns undergoing circumcision and receiving dorsal penile nerve blocks have been reported without any major complications.1–7 The nerve block is a simple procedure that can be easily performed. Typically, 0.4 mL of 1 percent lidocaine is injected into the subcutaneous tissue at the base of the penis at each of the points indicated in Figure 3a for a total of 0.8 mL.
Some physicians prefer to use a single mid-line injection, but this has not been well studied or described. A small amount (0.1 to 0.2 mL) of 1 percent sodium bicarbonate pre-mixed with lidocaine can decrease the pain caused by the acidic pH of the lidocaine solution. To avoid intravascular injection, negative pressure should be applied frequently to check for the absence of blood. Some clinicians prefer to administer the block before draping the area, and then to gently massage the area while waiting approximately five minutes required for maximum effect of the anesthetic to occur.
A low rate of minor complications such as local bruising, hematoma and excessive bleeding at the injection site have been reported.1,3–5 Theoretic but unreported complications include lidocaine toxicity, lidocaine effect, delay in voiding and interference with erectile function. The most serious complication that has been reported occurred in 1990,6 and involved a two-day-old infant who received a dorsal penile nerve block with an inadvertent injection of 1:1,000 epinephrine. The infant had a brief hemodynamic response followed by a profound vasoconstriction and ischemia of the genitalia. This was resolved by inserting a caudal catheter and establishing a sympathetic block. The use of epinephrine is contraindicated in any procedure involving the penile shaft.
In 1991, concerns were raised regarding the safety of the dorsal penile nerve block because of the limited number of case reports at that time.8 Concern centered on the potential risk of lidocaine in the dorsal vein causing systemic effects in the central nervous system or heart, or systemic absorption from the tissues (which could lead to toxicity). Thus far, these complications have not been reported.
Multiple studies2,5,7,11 have documented a decrease in pain perceived by the neonate during routine circumcision when a dorsal penile nerve block is used. Because of the reported lack of major complications in over 2,000 infants receiving this analgesic block, it is reasonable to recommend that physicians performing routine newborn circumcision should become familiar and proficient with this technique.
There has been interest in a lidocaine-prilocaine cream for use in circumcision. In one small trial,12 this cream was shown to be more effective than placebo. Although the manufacturer warns against its use in infants less than one month of age because of the potential risk of methemoglobinemia, this concern may be unwarranted.
3. What size of Gomco bell should be used? Does it have to completely cover the glans?
The size of the Gomco bell used for the circumcision is dependent on the diameter of the glans rather than on the length of the penile shaft. The bell should completely cover the glans penis without overly distending the foreskin. Too small a bell will fail to protect the glans and will cause the foreskin to be redundant as it is pulled through the base plate. If a bell is selected that does not fulfill these criteria, the physician should choose a different clamp and bell to get the best fit. Care should be taken to assure that the bell is the correct size for the plate and arm being used.
4. What technique should be used for getting the foreskin properly through the hole of the Gomco base plate after the bell has been applied?
Multiple techniques have been used to secure the foreskin in order to bring it through the hole of the base plate. The most important element of this procedure is to make sure that the bell stays under the foreskin and over the glans and that equal amounts of mucosa and foreskin are brought through the base plate. In addition, the apex of the dorsal slit must be visible above the plate before putting the arms in the yoke and excising the foreskin. A small safety pin may be used to bring the edges of the dorsal slit together over the flare of the bell before bringing the draw stud through the base plate. The safety pin should be inserted through both the foreskin and the mucosa so that care is taken not to omit the mucosal layer. In addition, the clinician must take special care to make sure that the sharp end of the safety pin does not cause inadvertent injury to the clinician or the infant. Once the safety pin is satisfactorily inserted through the foreskin and underlying mucosa, the base plate can be placed over the draw stud, followed by the safety pin holding the foreskin and the mucosa. The level at which the foreskin is to be excised can then be adjusted before placing the arms of the draw stud into the yoke.
A second method for bringing the foreskin through the base plate involves placing the bell between the glans and the foreskin, and then placing a hemostat directly through the hole in the base plate. The hemostat is then used to draw the edges of the dorsal slit together over the flare of the bell. The hemostat can then be pulled back through the hole in the base plate, bringing the draw stud and foreskin with it (Figure 4c and d). Once again, care must be taken to make sure that equal amounts of foreskin and underlying mucosa are brought through and excised. This approach limits the number of operative steps involved in performing the procedure.
A third method, and one that we prefer, involves clamping the edges of the dorsal slit together with a hemostat over the flare of the bell after it has been placed over the glans penis. This assures that the bell will stay in place. The draw stud is then brought through the hole of the base plate and two separate hemostats are then used to grasp the corners of the dorsal slit at the level of the preputial opening (Figure 6). The original hemostat is then removed from the foreskin at the level of the flare of the bell, and the two hemostats above the base plate can then be used to draw the foreskin and draw stud through the base plate hole. This technique allows exact adjustment of the angle of the bell as it lies over the glans and allows adjustment of the amount of foreskin and mucosa to be removed. Once again, care is taken to make sure that the foreskin and mucosa are within the clamps and that equal amounts are removed.
5. What should be done if the physician notices that the urethral meatus is displaced, and that the infant has either an epispadias or hypospadias after the dorsal slit has been made and the foreskin has been pulled proximally, exposing the glans?
At this point, the procedure should be terminated since any repair of these congenital anomalies may involve the use of foreskin tissue. If there is bleeding from the dorsal slit, the edges should be whipstitched using a fine chromic suture, or the dorsal slit may be closed using a interrupted fine chromic suture. In one study of complications resulting from circumcision,13 22 (0.4 percent) of 5,882 newborns studied were noted to have some type of hypospadias. One third of these infants had completion of the procedure despite the presence of an anomaly.
6. What should be done if the edges of the dorsal midline incision are bleeding persistently, making the procedure difficult?
Care must be taken at the time of creating the dorsal slit to stay within the crushed area of tissue and not to extend the dorsal slit past the apex of the area of crushed tissue. This will limit the amount of bleeding from the edges of the dorsal slit. Should bleeding occur, it is best to proceed with the circumcision because once the Gomco clamp is in place, bleeding from the dorsal slit will stop. If the bleeding interferes with continuing the procedure, a hemostat can be used to create a second area of crushed tissue overlying the area of bleeding. As long as the area of crushed tissue is within the portion of the foreskin that is to be removed during the circumcision, this will not change the cosmetic outcome of the procedure. If generalized bleeding persists without an obvious source, consideration should be given to the possibility of a bleeding disorder.
7. How can the bell be kept from falling off the glans while trying to get the draw stud through the hole of the base plate?
Failure to keep the bell in place while pulling the draw stud and the foreskin through the base plate can happen for a number of reasons: the preputial opening may be dilated, the dorsal slit may be too long or the bell being used may be too small. The immediate problem can be solved by changing the size of the Gomco clamp and bell, or by using a hemostat to draw the edges of the dorsal slit together across the flare of the bell while grasping the tissue around the dorsal slit on either side widely, thus creating tension on the foreskin across the flare of the bell.
8. What if, after everything is in place but before the Gomco nut has been closed, the physician is uncertain whether there is too much or too little foreskin above the base plate?
The amount of penile shaft skin that should remain after circumcision should be assessed before the actual circumcision. One way to do this is to mark the circumference of the shaft skin with a marker, typically at the coronal ridge. In addition, when the dorsal slit is created, the clinician should have an idea about how much shaft skin should remain below the base plate. Equal amounts of skin and mucosa must be pulled through the bevel hole. Inadequate separation of the mucous membrane from the glans may result in adhesions or phimosis. If a decision is made to adjust the amount of foreskin to be removed after the Gomco clamp is in place, it is important to disassemble the draw stud arms from the yoke and to pull the bell away from the base plate. If an attempt is made to adjust the amount of foreskin while the clamp and bell are still assembled, there is a risk that vessels between the foreskin and the underlying mucosa will be sheared off and will retract. The vessels will not be sealed when foreskin excision occurs and may be at risk for bleeding, causing wound dehiscence at the line of incision.
9. What if it appears that too little foreskin has been removed after the circumcision has been completed?
Once the circumcision has been performed by the clinician, it may become apparent that too little foreskin and/or underlying mucosa was removed, requiring another procedure. If the glans is not exposed following the circumcision, then this is probably the case. Failure to remove enough of these tissues is likely to be due to the lack of enough tissue being pulled through the base plate rather than using a clamp that is too small. Any subsequent procedure should be referred to a urologist.
10. What if the nurse checks the infant's penis 30 minutes after the procedure and reports that the glans is no longer visible?
If not enough foreskin or underlying mucosa is removed during circumcision, a condition known as concealed penis can occur. In this situation, the penile shaft and glans are pushed back into the scrotal fat and the penis is buried. As long as the baby is able to urinate without obstruction, there is no need for further procedure at this time. However, a revision of the circumcision may be necessary at a later time. This procedure should be performed by a pediatric urologist.
11. What is the most common reason for a poor cosmetic result?
Failure to completely free mucosal adhesions from the glans penis so that the entire coronal sulcus is exposed is the most common reason for a poor cosmetic result. The most common place for this to occur is at the coronal sulcus just lateral to the ventral frenulum. If the adhesions are not completely separated, not enough mucosa will be removed and the glans will not be completely exposed. Phimosis may result. In one study,14 this occurred in 2 percent of patients undergoing circumcision.
12. What if the parents want to take the infant home but he hasn't urinated yet?
Most nurseries require that the infant urinate before undergoing circumcision. However, barring complications during circumcision, there is no reason that the infant needs to stay in the hospital after circumcision until micturition occurs.
13. Should the physician perform a circumcision on an infant whose mother has HIV infection?
The HIV status of the mother should not affect the physician's decision to perform newborn circumcision unless she has thrombocytopenia. In that situation, the physician would first make sure that the baby has a normal platelet count. The staff involved in performing the circumcision should use universal precautions, as they should when performing any circumcision. We are not aware of any data regarding newborn circumcision in sons of HIV-positive mothers.
14. What if the parents request a Jewish ritual circumcision (known as Berit Mila)?
Fulfillment of the covenant of Berit Mila by people of the Jewish faith is one of their oldest rituals, dating back 5,000 years to Abraham. This ceremony usually occurs on the eighth day of an infant's life and is usually performed by a ritual circumciser known as a Mohel or Mohelet. Premature infants or infants who are ill may have the ceremony deferred until they are able to safely undergo circumcision. In a community with a large Jewish population, the Mohel or Mohelet is readily available. In a small town without a significant Jewish population, a Mohel or Mohelet may be harder to find and parents may have to locate one in a larger town or travel to the larger community themselves. Checking with a local Rabbi is probably the best way to find out what services or alternatives are available to a Jewish family.