
Am Fam Physician. 2002;65(8):1581-1585
Sarcoidosis is a multisystem disease that may involve almost any organ system; therefore, it results in various clinical manifestations. Cutaneous sarcoidosis occurs in up to one third of patients with systemic sarcoidosis. Recognition of cutaneous lesions is important because they provide a visible clue to the diagnosis and are an easily accessible source of tissue for histologic examination. Because lesions can exhibit many different morphologies, cutaneous sarcoidosis is known as one of the “great imitators” in dermatology. Specific manifestations include papules, plaques, lupus pernio, scar sarcoidosis, and rare morphologies such as alopecia, ulcers, hypopigmented patches, and ichthyosis. Treatment of cutaneous lesions can be frustrating. For patients with severe lesions or widespread involvement, the most effective treatment is systemic glucocorticoids.
Sarcoidosis is a systemic disease that can involve almost any organ system. Infiltration with noncaseating granulomas is the hallmark of the disease, and it may result in various clinical manifestations. The underlying cause of sarcoidosis remains unknown.1 Although the disease can occur at any age, in persons of either gender, and in all races, older studies suggest that sarcoidosis more frequently affects persons who are of Scandinavian, Irish, or black descent.1
Diagnosis
Cutaneous involvement occurs in 20 to 35 percent of patients with systemic sarcoidosis and may occur without systemic involvement.2 Because lesions assume a vast array of morphologies, cutaneous sarcoidosis is known as one of the “great imitators” in dermatology. Involvement may be mild or severe, self-limited or chronic, and limited or wide-ranging in extent.
Correctly diagnosing sarcoidosis may be a challenge. Unfortunately, no single test can prove the diagnosis. Patients are diagnosed with sarcoidosis when a compatible clinical or radiologic picture is present, along with histologic evidence of noncaseating granulomas, and when other potential causes, such as infections, are excluded.1
Recognition of Skin Lesions
Recognition of cutaneous lesions is important because they provide a visible clue to the diagnosis and are an easily accessible source of tissue for histologic examination. Punch or incisional wedge biopsy is typically used to obtain a sample of skin that includes the dermis. If noncaseating granulomas are found (Figure 1), tissue culture may be necessary to exclude infectious causes.
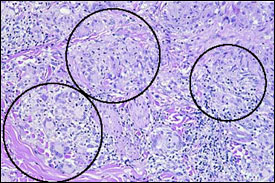
Most authors divide lesions of cutaneous sarcoidosis into nonspecific and specific types. Although nonspecific lesions occur in association with systemic sarcoidosis, no granulomas are found on biopsy. Specific lesions display noncaseating granulomas on biopsy.3 Table 1 provides an overview of the common presentations of cutaneous sarcoidosis with their corresponding differential diagnoses.
| Papules |
| Granulomatous rosacea |
| Acne |
| Benign appendageal tumors |
| Plaques |
| Psoriasis |
| Lichen planus |
| Nummular eczema |
| Discoid lupus erythematosus |
| Granuloma annulare |
| Cutaneous T-cell lymphoma |
| Kaposi's sarcoma |
| Secondary syphilis |
| Lupus pernio |
| Scar |
| Discoid lupus erythematosus |
| Erythema nodosum |
| Cellulitis |
| Furunculosis |
| Other inflammatory panniculitis |
ERYTHEMA NODOSUM
Erythema nodosum is the most common nonspecific cutaneous lesion of sarcoidosis.4 It represents a hypersensitivity reaction to a number of possible stimuli, including medications, infections, and inflammatory diseases. Erythema nodosum usually manifests as extremely tender, subcutaneous erythematous nodules, often on the anterior tibia (Figure 2). Onset of the condition may be sudden, accompanied by systemic symptoms such as fever, malaise, and polyarthralgias. Lofgren's syndrome refers to the constellation of erythema nodosum, bilateral hilar lymphadenopathy and polyarthralgias, which represents an acute presentation of systemic sarcoidosis.1 Biopsy of erythema nodosum reveals panniculitis with septal inflammation.

SPECIFIC SARCOID LESIONS
All specific cutaneous lesions exhibit noncaseating granulomas on biopsy. Despite this same histologic appearance, clinical appearance of the lesions may be markedly variable. The term “specific” is misleading because the clinical appearance of such lesions is usually not specific for sarcoidosis, and the correct diagnosis is often reached only after skin biopsy is performed.
The most common types of specific lesions are papules.3 They commonly occur on the face but may occur anywhere on the body. While only a few papules may be noted (Figure 3), multiple scattered or confluent lesions are more common. Papules of sarcoidosis may be of various colors, including red, reddish-brown, violaceous, translucent, or hyperpigmented. Most exhibit little surface change and are indurated on palpation.
Plaques are larger, flat-topped lesions that are located on the face (Figure 4), trunk, or extremities. The lesions may be single or multiple. When plaques are multiple, distribution of the lesions tends to be symmetric (Figure 5). As with papules, plaques can also be of various colors. They may be associated with large telangiectatic vessels or may exhibit thick scaling that mimics psoriasis. Plaques on the face can imitate discoid lupus, particularly when central atrophy and scaling are present.


Lupus pernio is one of the few cutaneous manifestations that are characteristic of sarcoidosis. Lesions are chronic, indurated papules or plaques that affect the mid-face, particularly the alar rim of the nose (Figure 6). Even a few small papules in this location may be associated with granulomatous infiltration of the nasal mucosa and upper respiratory tract, resulting in masses, ulcerations, or even life-threatening airway obstruction.5
Lesions of cutaneous sarcoidosis can also appear in preexisting scars. This condition is known as scar sarcoidosis. Therefore, sarcoidosis should be considered in the differential diagnosis of an enlarging, previously inactive scar. While the pathogenesis of scar sarcoidosis is unknown, lesions can develop in scars caused by mechanical trauma, such as venipuncture, and scars caused by infection, such as herpes zoster, as well as in tattoos.4 Clinically, the lesions are papular and may be mistaken for keloids.
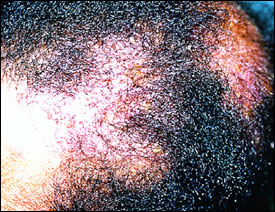
Multiple other cutaneous morphologies are possible; many are quite rare, although the incidence is difficult to determine.6 Sarcoidosis of the scalp may result in scarring (Figure 7) or nonscarring alopecia.7 Ulcerative sarcoidosis can lead to ulcerated lesions of sarcoidosis or may even develop in de novo lower leg ulcers.8 Other unusual manifestations include hypopigmented patches,6 ichthyosis of the lower legs,9 subcutaneous nodules, and erythroderma.


The relationship between cutaneous and systemic sarcoidosis is being studied. Cutaneous involvement in systemic sarcoidosis may occur at any stage of the disease. However, it is most often present at the onset and may even be the presenting complaint. Every patient with cutaneous sarcoidosis requires an initial work-up for systemic involvement, followed by periodic screening. In one study,3 approximately 30 percent of patients who initially had only cutaneous lesions developed systemic involvement months to years later.
While recommendations vary, a baseline work-up for systemic sarcoidosis should include a complete history and physical examination, baseline laboratory testing (calcium, renal function, hepatic function), chest radiography and pulmonary function testing, electrocardiography, and ophthalmologic evaluation.1 Certain types of cutaneous lesions may have a bearing on prognosis of systemic sarcoidosis. Lesions of lupus pernio, in particular, are associated with more severe systemic involvement, while erythema nodosum often indicates acute benign disease.3
Treatment
The treatment of cutaneous sarcoidosis is often frustrating, because lesions may be refractory to treatment or may recur following successful treatment. For localized involvement, topical or intralesional steroids are used. Physicians frequently attempt to use superpotent topical steroids because of their occasional effectiveness. However, these steroids often do not adequately penetrate the skin lesion. Intralesional steroids (e.g., triamcinolone acetonide [Kenalog] in a dosage of 5 mg per mL)10 are typically more effective, with injections repeated at two- to three-week intervals.
Systemic agents are reserved for widespread, progressive lesions or those that impair function. Systemic glucocorticoids are the most effective agents.2 They are commonly used at slow, tapering dosages, starting at 20 to 40 mg of oral prednisone daily for four to six weeks.4 However, there are many drawbacks to this therapy. Aside from the well-known complications of chronic steroid use, not all patients respond to systemic steroids. Those who do respond frequently experience flare-ups of disease when the treatment is completed. Many other medications may be used in refractory cases, including such agents as hydroxychloroquine (Plaquenil),11 methotrexate (Rheumatrex),12 and thalidomide (Thalomid).13 Although randomized, controlled trials are lacking, multiple anecdotal reports suggest the efficacy of these agents.