
Am Fam Physician. 2004;69(3):561-569
A more recent article on obstructive sleep apnea is available.
Obstructive sleep apnea should be suspected in patients who are overweight, snore loudly, and have chronic daytime sleepiness. The diagnosis of sleep apnea may be confirmed by sleep laboratory studies. Patients' symptoms and the frequency of respiratory events on laboratory testing are important factors in determining the severity of disease. In patients with mild sleep apnea, conservative treatment measures include getting sufficient sleep, abstaining from the use of alcohol and sedatives, losing weight, and avoiding the supine position during sleep. Continuous positive airway pressure (CPAP) is the most consistently effective treatment for clinically significant obstructive sleep apnea. In general, heavier patients with thicker necks require higher pressure settings. As patients age or gain weight, additional pressure may be necessary. Bilevel pressure machines or machines that slowly ramp up the pressure may increase patient acceptance of CPAP therapy. Complications of CPAP use include nasal dryness and congestion, claustrophobia, facial skin abrasions, air leaks, and conjunctivitis. Strategies to improve patient compliance include allowing patients to try a number of masks to find the most comfortable fit, adding humidification, treating nasal disease and, most importantly, providing close follow-up and encouragement. Oral appliances are inconsistently effective in the management of obstructive sleep apnea but may be an option in patients with mild disease who cannot tolerate CPAP. Palatal surgery often decreases snoring but may not reduce the occurrence of sleep apnea. Patients with severe disease and intolerance of CPAP may be candidates for more invasive surgical procedures. Supplemental oxygen and drug therapy may have limited, adjunctive roles in the treatment of obstructive sleep apnea.
Sleep apnea is a cessation of breathing during sleep that is caused by repetitive partial or complete obstruction of the airway by pharyngeal structures. Patients with obstructive sleep apnea often are overweight, snore loudly, and complain of daytime fatigue and sleepiness. A sleep laboratory may be used to confirm the diagnosis. Family physicians should be able to diagnose and manage this relatively common disorder.
Deciding When to Treat
The initial step in the management of sleep apnea is deciding which patients need treatment. The severity of the condition is measured by the number of apneas (cessations of airflow) or hypopneas (reductions in airflow) that cause sleep arousal. The number of these events per hour is commonly called the “apnea-hypopnea index” or the “respiratory disturbance index.” An often quoted study recommended treatment if patients had 20 or more respiratory events per hour, because long-term mortality increases above that level.1 [Strength of recommendation B, cohort study] However, patients with five or fewer respiratory events per hour may merit treatment if they complain of sleepiness and fatigue, or have secondary medical complications such as heart failure.2
Sleep Hygiene
Patients who snore but have no more than mild sleep apnea on laboratory testing may be treated adequately with conservative measures involving good sleep hygiene. The physician should verify that patients are spending adequate time in bed. Sleep deprivation increases a person's propensity to snore.3–5
Treatment of disorders that reduce nasal airflow, such as chronic rhinitis, nasal polyps, or septal deviation, is important because reduced nasal airflow increases the propensity to snore. Moreover, mouth breathing during sleep, which results from nasal obstruction, causes the jaw to drop and reduces the diameter of the pharyngeal airway, increasing the likelihood of obstructive sleep apnea.
Patients with obstructive sleep apnea should avoid alcohol and other sedating agents. Because patients with sleep apnea tend to sleep poorly, they are more likely to turn to sedatives to promote sleep. However, such sleep aids may cause snoring in persons who normally do not snore, while persons who already snore may become apneic if the sleep aids relax the tongue and parapharyngeal muscles.
The majority of patients who have obstructive sleep apnea are overweight. Sometimes losing even a modest amount of weight, such as 9.1 to 13.6 kg (20 to 30 lb), improves sleep apnea significantly. Unfortunately, only a small percentage of dieters permanently lose weight.6 Recent data show that up to 6 percent of older adults gain enough weight to develop significant sleep apnea over a period as short as four years.7
Raising the head of the bed and avoiding the supine position during sleep are methods of decreasing the incidence of apnea. Elevation of the head tends to bring the tongue forward, while sleeping on the side moves the tongue laterally.
Patients with mild sleep apnea tend to respond best to conservative measures. Those with greater degrees of sleep apnea should continue to use these measures while receiving more invasive therapy.
Continuous Positive Airway Pressure
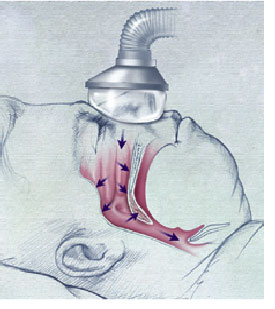
Many patients with documented sleep apnea require more than conservative therapy. Continuous positive airway pressure (CPAP) is the most consistently successful and extensively studied treatment for obstructive sleep apnea. CPAP machines contain a fan that blows air under pressure into the nostrils. The airflow acts as a pneumatic splint that keeps the pharyngeal airway open (Figure 1). CPAP is not curative, and patients must use the mask whenever they sleep. A recent systematic review concluded that CPAP therapy improves quality of sleep and reduces problems of excessive daytime sleepiness in patients with obstructive sleep apnea.8 [Strength of recommendation B, systematic review of lower quality randomized controlled trials] Other studies9,10 have shown that CPAP therapy improves mood and functional status in patients with sleep apnea, and decreases the incidence of motor vehicle crashes in these patients.
PRESSURE REQUIREMENTS
The optimal pressure to use in CPAP therapy is determined in a sleep laboratory study, during which the degree of apnea is monitored with various mask adjustments and increasing levels of air pressure. Pressures are measured in centimeters of water and can vary from 3 to 20 cm, with most patients requiring 6 to 12 cm of pressure to reduce their respiratory disturbance index to fewer than 10 events per hour.
Sleep studies last one or two nights. In a full-night study, one entire session is devoted to documenting the presence and severity of sleep apnea; the second full-night session is used to titrate CPAP treatment.
When sleep laboratory availability or expense is an issue, physicians should consider a split-night study that screens for sleep apnea during the first few hours and then adjusts CPAP treatment during the rest of the night. The therapeutic pressure that is determined in a split-night study usually is close to the pressure determined during a full, eight-hour CPAP trial.11 There may be a disadvantage to using the split-night study when pretest clinical suspicion of sleep apnea is unclear or when tolerance of the CPAP mask is difficult (i.e., there may not be enough time to make proper adjustments).
A number of studies have attempted to predict optimal CPAP pressure to control apnea. In general, heavier patients with short, thick necks and severe apnea require higher pressures.12 The most symptomatic and severely apneic patients also tolerate higher pressures better than thinner patients with mild disease.
The pressure required to control sleep apnea is not always static. One study13 showed that after four weeks of mask treatment, the median reduction in pressure requirements was 1.5 cm of water. A possible explanation may be a reduction in airway edema following cessation of snoring.
CPAP requirements also may change over longer periods. Weight loss may reduce the level of required CPAP pressure, while weight gain often necessitates the use of higher pressures. Furthermore, sleep apnea typically increases with age. Patients who have been stable for several years on a given CPAP pressure may gradually resume snoring. A return of symptoms signals the need for reassessment of the CPAP pressure.
COMPLIANCE
Despite the effectiveness of CPAP, many patients have difficulty tolerating this therapy. Patients may complain about the rush of air pressure during CPAP, especially on exhalation. Bilevel pressure ventilation uses a decreased air pressure during exhalation and may be more acceptable to some patients.14 Differences between inspiratory and expiratory pressures can vary by as much as 5 to 7.5 cm of pressure in some patients. Bilevel positive airway pressure may have a particular role in patients with chronic lung disease because it reduces the work of breathing.15
Older study results showed lower compliance rates, depending on how compliance is defined. Long-term compliance with CPAP therapy may be challenging. Up to 50 percent of patients will not wear the mask for an adequate period each night.16 Short-term nightly use of more than 90 percent can be achieved when close follow-up is provided by a nurse skilled in CPAP use.17
| Optimal mask fit | |
| Appropriate mask size and shape | |
| Nasal pillows | |
| Full-face mask | |
| Close patient follow-up and encouragement | |
| Treatment of nasal symptoms | |
| Cool or warm humidification of air | |
| Nasal steroid spray | |
| Ear, nose, and throat evaluation | |
| Surgery | |
A number of strategies may be used to improve CPAP compliance (Table 1). The technical staff in the sleep laboratory can help patients with initial acceptance of CPAP by offering masks in a variety of sizes, shapes, and materials to optimize patient comfort. Many CPAP machines have a “ramp” feature that improves patient comfort by slowly raising the pressure output during the first 30 minutes as the patient tries to initiate sleep. Some patients require a chin strap to keep the mouth closed and avoid oral air leakage during CPAP therapy.
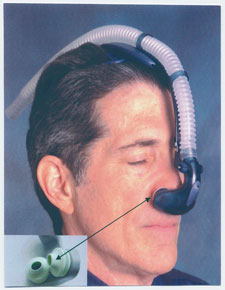
Nasal pillows are an alternative to the CPAP mask and may improve compliance. When nasal pillows are used, air is blown directly into the nostrils (Figure 2). Some patients elect to use a CPAP mask one night and nasal pillows the next night to reduce the chance of pressure irritation from either appliance.
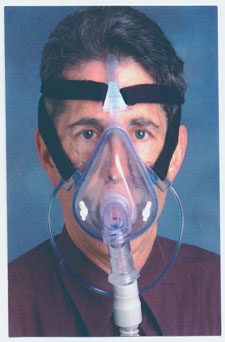
Occasionally, patients with significant nasal obstruction benefit from use of a full-face mask (Figure 3). With this device, positive airway pressure can be exerted through the nose, the mouth, or both. Patients scheduled for nasal surgery may benefit from using this type of mask, because CPAP therapy can help in the perioperative period when the nasal passages are packed. Patients can be converted to a nasal mask after the nasal disease has been corrected. Full-face masks are generally well tolerated, but the potential for aspiration exists in patients who are sedated with alcohol or medication.
Physicians should encourage patients to use the CPAP mask. When beginning CPAP treatment, some patients cannot wear the mask for more than one hour at a time. Wearing time often increases slowly over a few months. Patients who continue to complain of residual daytime sleepiness despite the use of CPAP should be questioned carefully about actual mask wearing time, because studies have shown that patients often overestimate the time they spend wearing the mask.18,19
Physicians also should review sleep hygiene. Prolonged sleeping times on weekends or days off suggest insufficient sleep time during the rest of the week. Patients who begin to feel more rested after initiating CPAP treatment may shift to a later bedtime, which can result in a recurrence of daytime fatigue.
COMPLICATIONS
Minor complications that may occur with CPAP treatment include, in order of frequency, nasal symptoms (dryness, congestion, rhinorrhea), air leakage from the mask, claustrophobia, skin abrasions, and conjunctivitis. Initial complaints about mask use include nasal mucosal drying and congestion, claustrophobia, and pressure on the face.
A room-temperature humidifier attached to the CPAP machine adds moisture and often is helpful in patients with nasal drying or congestion. Cold, dry air coming directly from the CPAP mask may increase nasal resistance via increased nasal congestion. Heated humidification is more expensive but may be attempted in particularly difficult cases.20 Nasal irritation and congestion may be treated with nasal sprays containing steroids, ipratropium, or antihistamines. Patients with persistent difficulties may benefit from referral to an ear, nose, and throat specialist.
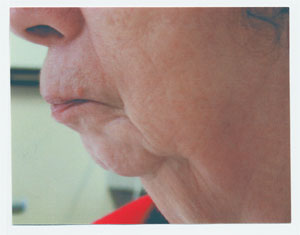
The CPAP mask should fit snugly. However, if the mask is too tightly fitted, it can cause abrasions of the nasal bridge (Figure 4).
Oral Appliances
Various oral appliances can be used to move the tongue or mandible forward. These devices are used most often in patients who snore but have only mild apnea. The efficacy of oral appliances in the treatment of obstructive sleep apnea has been inconsistent. However, one recent long-term study21 showed a partial response in up to two thirds of patients.
Current guidelines from the American Sleep Disorders Association recommend that patients being considered for oral appliances have an initial sleep study to assess the presence and severity of sleep apnea. To ensure efficacy, a follow-up study in patients with moderate to severe sleep apnea with the device in place is recommended.22

Insurance companies generally do not pay for oral appliances, which may cost $600 or more. Moreover, finding a dentist who can fit the appropriate device and follow the patient may be a challenge. More research is necessary before any universal recommendation can be made about the use of oral appliances in the treatment of obstructive sleep apnea.
Surgery
PALATAL SURGERY
Patients who cannot be treated adequately with CPAP or other conservative measures and who have clinically significant disease may want to consider more invasive treatment. Uvulopalatoplasty is a surgical or laser procedure that removes part of the uvula and soft palate in an attempt to alleviate snoring and sleep-disordered breathing. Radiofrequency methods (i.e., somnoplasty) also can reduce palatal soft tissue.23
Palatal surgical procedures tend to alleviate snoring but are not consistently effective in treating sleep apnea. Many patients with sleep apnea have airway obstruction beyond the palatal area that is not treated by soft tissue procedures.
JAW SURGERY
Patients with maxillomandibular anatomy that predisposes them to airway obstruction may be considered for jaw surgery (Figure 5). In one study,24 maxillomandibular advancement surgery effectively treated sleep apnea in as many as 95 percent of patients; however, no randomized studies are available. Radiographs of the jaw and skull (cephalometrics) are obtained before surgery to help the oral surgeon make relational measurements of the jaw, teeth, and airway.
Among the less invasive jaw procedures is genial tubercle and tongue advancement, in which the anterior tip of the mandible is moved forward along with its lingual attachments, bringing the tongue forward and increasing the diameter of the airway.25
Advancement of both the upper and lower jaws with bimaxillary and mandibular osteotomies is a more definitive but much more invasive surgery. Patients who have this type of surgery should expect a prolonged postoperative recovery time while the jaws are fixed or wired shut to allow healing. Complications include lingual or oral numbness and malpositioning of the jaw. Adolescents and young adults with more severe apnea who cannot tolerate CPAP and are willing and healthy enough to undergo extensive oral surgery may be candidates for the procedures.
OTHER SURGICAL PROCEDURES
Tracheotomy is a last-resort measure that is employed only in life-threatening situations, such as acute respiratory failure or when patients are severely apneic and noncompliant. Because of complications and disability, tracheotomy generally is not well accepted by patients as a long-term treatment.26
In patients with morbid obesity, weight loss via bariatric surgery helps to decrease the severity of obstructive sleep apnea.27 However, the potential complications and cost of this type of surgery relegate it to a secondary role in the treatment of sleep apnea.
Supplemental Oxygen and Drug Therapy
Oxygen and medications may have adjunctive roles in the treatment of obstructive sleep apnea in some patients. They rarely are used as primary treatments.
Oxygen therapy is only partially effective. Although it helps to treat the oxyhemoglobin desaturation that occurs with some respiratory events, it does not reverse obstruction. When supplemental oxygen is used, apneas occur less frequently but may last longer.28 Oxygen therapy may be useful in patients for whom no other treatments are acceptable, but carbon dioxide retention is a risk in patients with severe underlying lung disease.
Because of fatigue and sleep deprivation, depression is a common complication of obstructive sleep apnea. Protriptyline (Vivactil) is a tricyclic antidepressant that depresses rapid eye movement (REM) sleep, the period during which the most significant apneas often occur.29 However, the drug is not used often because of its anticholinergic side effects. A large number of newer antide-pressants also decrease REM sleep and, thus, have the potential to improve sleep apnea. As yet, however, no clear evidence supports their use.