
Am Fam Physician. 2004;69(7):1707-1714
Shoulder dystocia can be one of the most frightening emergencies in the delivery room. Although many factors have been associated with shoulder dystocia, most cases occur with no warning. Calm and effective management of this emergency is possible with recognition of the impaction and institution of specified maneuvers, such as the McRoberts maneuver, suprapubic pressure, internal rotation, or removal of the posterior arm, to relieve the impacted shoulder and allow for spontaneous delivery of the infant. The “HELPERR” mnemonic from the Advanced Life Support in Obstetrics course can be a useful tool for addressing this emergency. Although no ideal manipulation or treatment exists, all maneuvers in the HELPERR mnemonic aid physicians in completing one of three actions: enlarging the maternal pelvis through cephalad rotation of the symphysis and flattening of the sacrum; collapsing the fetal shoulder width; or altering the orientation of the longitudinal axis of the fetus to the plane of the obstruction. In rare cases in which these interventions are unsuccessful, additional management options, such as intentional clavicle fracture, symphysiotomy, and the Zavanelli maneuver, are described.
Shoulder dystocia is one of the most anxiety-provoking emergencies encountered by physicians practicing maternity care. Typically defined as a delivery in which additional maneuvers are required to deliver the fetus after normal gentle downward traction has failed, shoulder dystocia occurs when the fetal anterior shoulder impacts against the maternal symphysis following delivery of the vertex. Less commonly, shoulder dystocia results from impaction of the posterior shoulder on the sacral promontory.1
The overall incidence of shoulder dystocia varies based on fetal weight, occurring in 0.6 to 1.4 percent of all infants with a birth weight of 2,500 g (5 lb, 8 oz) to 4,000 g (8 lb, 13 oz), increasing to a rate of 5 to 9 percent among fetuses weighing 4,000 to 4,500 g (9 lb, 14 oz) born to mothers without diabetes.2–4 Shoulder dystocia occurs with equal frequency in primigravid and multigravid women, although it is more common in infants born to women with diabetes.2,5 Several additional prenatal and intrapartum factors have been associated with an increased incidence of shoulder dystocia (Table 1). The single most common risk factor for shoulder dystocia is the use of a vacuum extractor or forceps during delivery.2 However, most cases occur in fetuses of normal birth weight and are unanticipated, limiting the clinical usefulness of risk-factor identification.6
Complications resulting from shoulder dystocia during delivery can affect the mother and infant (Table 2). Postpartum hemorrhage (11 percent) and fourth-degree lacerations (3.8 percent) are the most common maternal complications, and their incidence remains unchanged by rotation maneuvers or other manipulation.7 Among the most common fetal complications are brachial plexus palsies, occurring in 4 to 15 percent of infants.4,7,8 These rates remain constant, independent of operator experience.4,5 Nearly all palsies resolve within six to 12 months, with fewer than 10 percent resulting in permanent injury.7,9,10
| Maternal |
| Abnormal pelvic anatomy |
| Gestational diabetes |
| Post-dates pregnancy |
| Previous shoulder dystocia |
| Short stature |
| Fetal |
| Suspected macrosomia |
| Labor related |
| Assisted vaginal delivery (forceps or vacuum) |
| Protracted active phase of first-stage labor |
| Protracted second-stage labor |
Although shoulder dystocia and disimpaction maneuvers historically have been blamed for the etiology of these palsies, in utero positioning of the fetus, a precipitous second stage of labor, and maternal forces may contribute to their etiology.4,6,10 Additional research demonstrates that a significant percentage of palsy-type injuries occur without association to shoulder dystocia and sometimes during cesarean delivery.11,12 The rate of persistence is significantly higher at one year in cases of Erb's palsy without identified shoulder dystocia. Other common morbidities from shoulder dystocia include fractures of the clavicle and humerus, which typically heal without deformity. In severe cases, hypoxic injury or death may occur.2,13
Prevention
Evidence is lacking to support labor induction or elective cesarean delivery in women without diabetes who are at term when a fetus is suspected of having macrosomia.14 In two studies of 313 women without diabetes, induction for suspected fetal macrosomia did not lower the rates of shoulder dystocia or cesarean delivery, nor did it improve the rates of maternal or neonatal morbidity.15 [strength of recommendation (SOR) evidence level A, meta-analysis] While labor induction in women with gestational diabetes who require insulin may reduce the risk of macrosomia and shoulder dystocia, the risk of maternal or neonatal injury is not modified. Not enough evidence is available to routinely support elective delivery in this population.16,17 [SOR evidence level B, systematic review including a single randomized trial]
Similarly, prophylactic cesarean delivery is not recommended as a means of preventing morbidity in pregnancies in which fetal macrosomia is suspected.9 [SOR evidence level C, expert opinion based on cost-effectiveness analysis] Analytic decision models have estimated that 2,345 cesarean deliveries, at a cost of nearly $5 million annually, would be needed to prevent one permanent brachial plexus injury in a patient without diabetes who had a fetus suspected of weighing more than 4,000 g. In the subgroup of women with diabetes, the frequency of shoulder dystocia, brachial plexus palsy, and cesarean delivery was higher, leading the authors to conclude that a policy of elective cesarean delivery in this group potentially may have greater merit.9 [SOR evidence level C, expert opinion based on cost-effectiveness analysis]
| Maternal |
| Postpartum hemorrhage |
| Rectovaginal fistula |
| Symphyseal separation or diathesis, with or without transient femoral neuropathy |
| Third- or fourth-degree episiotomy or tear |
| Uterine rupture |
| Fetal |
| Brachial plexus palsy |
| Clavicle fracture |
| Fetal death |
| Fetal hypoxia, with or without permanent neurologic damage |
| Fracture of the humerus |
Preliminary Management and Concerns
When a shoulder dystocia occurs, umbilical cord compression between the fetal body and the maternal pelvis is a potential danger. While the safe amount of time in which significant fetal acidosis related to shoulder dystocia can be avoided is unknown, the fetal pH will drop by an estimated 0.14 per minute during delivery of the fetal trunk.18–20 No significant linear relationship has been identified between the head-to-body delivery interval and fetal acid-base balance.21
If shoulder dystocia is anticipated on the basis of risk factors, preparatory tasks can be accomplished before delivery. Key personnel can be alerted, and the patient and her family can be educated about the steps that will be taken in the event of a difficult delivery. The patient's bladder should be emptied, and the delivery room cleared of unnecessary clutter to make room for additional personnel and equipment.
One method of preliminary intervention for shoulder dystocia in a patient with risk factors involves implementing the “head and shoulder maneuver” to “deliver through” until the anterior shoulder is visible.22 [SOR evidence level C, expert opinion] This step is accomplished by continuing the momentum of the fetal head delivery until the shoulder is visible. After controlled delivery of the head, the physician proceeds with immediate delivery of the anterior shoulder without stopping to suction the oropharynx.
Reduction Maneuvers and the HELPERR Mnemonic
Shoulder dystocia becomes obvious when the fetal head emerges and then retracts against the perineum, commonly referred to as the “turtle sign.” Excessive force must not be applied to the fetal head or neck, and fundal pressure must be avoided, because these activities are unlikely to free the impaction and may cause injury to the infant and mother.23,24 [SOR evidence level B, consistent observational studies]
| H | Call for help. |
| This refers to activating the pre-arranged protocol or requesting the appropriate personnel to respond with necessary equipment to the labor and delivery unit. | |
| E | Evaluate for episiotomy. |
| Episiotomy should be considered throughout the management of shoulder dystocia but is necessary only to make more room if rotation maneuvers are required. Shoulder dystocia is a bony impaction, so episiotomy alone will not release the shoulder. Because most cases of shoulder dystocia can be relieved with the McRoberts maneuver and suprapubic pressure, many women can be spared a surgical incision. | |
| L | Legs (the McRoberts maneuver) |
| This procedure involves flexing and abducting the maternal hips, positioning the maternal thighs up onto the maternal abdomen. This position flattens the sacral promontory and results in cephalad rotation of the pubic symphysis. Nurses and family members present at the delivery can provide assistance for this maneuver. | |
| P | Suprapubic pressure |
| The hand of an assistant should be placed suprapubically over the fetal anterior shoulder, applying pressure in a cardiopulmonary resuscitation style with a downward and lateral motion on the posterior aspect of the fetal shoulder. This maneuver should be attempted while continuing downward traction. | |
| E | Enter maneuvers (internal rotation) |
| These maneuvers attempt to manipulate the fetus to rotate the anterior shoulder into an oblique plane and under the maternal symphysis (seeFigure 2). These maneuvers can be difficult to perform when the anterior shoulder is wedged beneath the symphysis. At times, it is necessary to push the fetus up into the pelvis slightly to accomplish the maneuvers. | |
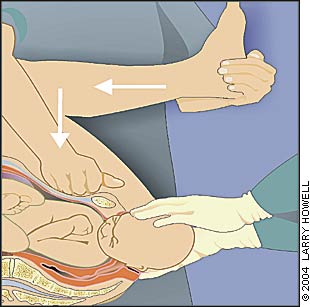
| R | Remove the posterior arm. |
| Removing the posterior arm from the birth canal also shortens the bisacromial diameter, allowing the fetus to drop into the sacral hollow, freeing the impaction. The elbow then should be flexed and the forearm delivered in a sweeping motion over the fetal anterior chest wall. Grasping and pulling directly on the fetal arm may fracture the humerus. | |
| R | Roll the patient. |
| The patient rolls from her existing position to the all-fours position. Often, the shoulder will dislodge during the act of turning, so that this movement alone may be sufficient to dislodge the impaction. In addition, once the position change is completed, gravitational forces may aid in the disimpaction of the fetal shoulders. |
The HELPERR mnemonic is a clinical tool that offers a structured framework for coping with shoulder dystocia (Table 3).25 These maneuvers are designed to do one of three things: increase the functional size of the bony pelvis through flattening of the lumbar lordosis and cephalad rotation of the symphysis (i.e., the McRoberts maneuver)25; decrease the bisacromial diameter (i.e., the breadth of the shoulders) of the fetus through application of suprapubic pressure (i.e., internal pressure on the posterior aspect of the impacted shoulder); or change the relationship of the bisacromial diameter within the bony pelvis through internal rotation maneuvers.
Although there is no indication that any one of these techniques is superior to another, together they effectively relieve the impacted shoulder. The order of the steps is not as important as the fact that they each be employed efficiently and appropriately. Persistence in any one ineffective maneuver should be avoided. Clinical judgment always should guide the progression of procedures used.
CALL FOR HELP
If standard levels of traction do not relieve the shoulder dystocia, the physician must move quickly to other maneuvers while asking for help and notifying the family. A critical step in addressing the emergency management of shoulder dystocia is ensuring that all involved hospital personnel are familiar with their roles and responsibilities. This delivery team may include a family physician or obstetrician, a pediatrician or neonatologist, one or two labor nurses to assist with maneuvers, a neonatal or nursery nurse, and a clinician capable of providing anesthesia.
The primary physician should direct the team's activities, and one person should record the timing and events, so that if one maneuver is not successful after a reasonable amount of time, another maneuver may be attempted. An institutional protocol should be designed to delineate individual roles, and hospital drills may be helpful to rehearse this protocol.
EPISIOTOMY
Episiotomy should be considered when a shoulder dystocia is encountered, although because the primary problem is a bony impaction, episiotomy by itself will not release the impaction. Episiotomy does provide additional room for the physician's hand when internal rotation maneuvers are required. Given the success of the McRoberts maneuver and suprapubic pressure in relieving a large percentage of cases of shoulder dystocia, performing an episiotomy can wait until later in the sequence.
LEGS (MC ROBERTS MANEUVER)
The simplicity of the McRoberts maneuver (Figure 125 ) and its proven effectiveness make it an ideal first step in the management of shoulder dystocia. This procedure results in a cephalad rotation of the symphysis pubis and a flattening of the sacral promontory.26 These motions push the posterior shoulder over the sacral promontory, allowing it to fall into the hollow of the sacrum, and rotate the symphysis over the impacted shoulder. When this maneuver is successful, the fetus should be delivered with normal traction. The McRoberts maneuver alone is believed to relieve more than 40 percent of all shoulder dystocias and, when combined with suprapubic pressure, resolves more than 50 percent of shoulder dystocias.6 [SOR evidence level B, retrospective cohort study]
PRESSURE (SUPRAPUBIC)
When applying suprapubic pressure, an assistant's hand should be placed on top of the mother's abdomen over the fetal anterior shoulder, applying pressure in a compression/relaxation cycle analogous to cardiopulmonary resuscitation, so that the shoulder will adduct and pass under the symphysis. Pressure should be applied from the side of the mother, with the heel of the assistant's hand moving in a downward and lateral motion on the posterior aspect of the fetal impacted shoulder. Initially, the pressure can be continuous, but if delivery is not accomplished, a rocking motion is recommended to dislodge the shoulder from behind the pubic symphysis. Fundal pressure is never appropriate and only serves to worsen the impaction, potentially injuring the fetus or mother.24 [SOR evidence level B, retrospective cohort study]
ENTER (INTERNAL ROTATION MANEUVERS)
Rotation maneuvers (Figure 227) may require episiotomy to gain posterior vaginal space for the physician's hand. The Rubin II maneuver consists of inserting the fingers of one hand vaginally behind the posterior aspect of the anterior shoulder of the fetus and rotating the shoulder toward the fetal chest. This motion will adduct the fetal shoulder girdle, reducing its diameter. The McRoberts maneuver also can be applied during this maneuver and may facilitate its success.
If the Rubin II maneuver is unsuccessful, the Woods corkscrew maneuver may be attempted. The physician places at least two fingers on the anterior aspect of the fetal posterior shoulder, applying gentle upward pressure around the circumference of the arc in the same direction as with the Rubin II maneuver. This motion creates a more effective rotation. The Rubin II and Woods corkscrew maneuvers may be combined to increase torque forces by using two fingers behind the fetal anterior shoulder and two fingers in front of the fetal posterior shoulder. Procedurally, this step often is difficult because of limited space for the physician's hand. Downward traction should be continued during these rotational maneuvers, simulating the rotation of a screw being removed.
If the Rubin II or Woods corkscrew maneuvers fail, the reverse Woods corkscrew maneuver may be tried. In this maneuver, the physician's fingers are placed on the back of the posterior shoulder of the fetus, and the fetus is rotated in the opposite direction as in the Woods corkscrew or Rubin II maneuvers. This maneuver adducts the fetal posterior shoulder in an attempt to rotate the shoulders out of the impacted position and into an oblique plane for delivery.
REMOVAL OF THE POSTERIOR ARM
Removal of the posterior arm involves placing the physician's hand in the vagina and locating the fetal arm, which sometimes is displaced behind the fetus and must be nudged anteriorly. The physician's hand, wrist, and forearm may need to enter the vagina, necessitating an episiotomy or extension. The fetal elbow is then flexed, and the forearm is delivered in a sweeping motion over the anterior chest wall of the fetus. The upper arm should never be grasped and pulled directly, because this step may result in a fracture of the humerus. The posterior hand, followed by the arm and shoulder, will be reduced, facilitating delivery of the infant. Often, the fetus spontaneously rotates in a corkscrew manner as the arm is removed. The anterior shoulder will then fall under the symphysis and deliver.
| Deliberate clavicle fracture |
| Direct upward pressure on the mid-portion of the fetal clavicle; reduces the shoulder-to-shoulder distance. |
| Zavanelli maneuver |
| Cephalic replacement followed by cesarean delivery; involves rotating the fetal head into a direct occiput anterior position, then flexing and pushing the vertex back into the birth canal, while holding continuous upward pressure until cesarean delivery is accomplished. Tocolysis may be a helpful adjunct to this procedure, although it has not been proved to enhance success over cases in which it was not used.28 An operating team, anesthesiologist, and physicians capable of performing a cesarean delivery must be present, and this maneuver should never be attempted if a nuchal cord previously has been clamped and cut. |
| General anesthesia |
| Musculoskeletal or uterine relaxation with halothane (Fluothane) or another general anesthetic may bring about enough uterine relaxation to affect delivery. Oral or intravenous nitroglycerin may be used as an alternative to general anesthesia. |
| Abdominal surgery with hysterotomy |
| General anesthesia is induced and cesarean incision performed, after which the surgeon rotates the infant transabdominally through the hysterotomy incision, allowing the shoulders to rotate, much like a Woods corkscrew maneuver. Vaginal extraction is then accomplished by another physician.29 |
| Symphysiotomy |
| Intentional division of the fibrous cartilage of the symphysis pubis under local anesthesia has been used more widely in developing countries than in North America. It should be used only when all other maneuvers have failed and capability of cesarean delivery is unavailable.30,31 |
ROLL THE PATIENT
Rolling the patient onto her hands and knees, known as the all-fours or Gaskin maneuver, is a safe, rapid, and effective technique for the reduction of shoulder dystocia.32 [SOR evidence level B, cohort study] Radiographic studies indicate that pelvic diameters increase when laboring women change from the dorsal recumbent position.33 The true obstetric conjugate increases by as much as 10 mm, and the sagittal measurement of the pelvic outlet increases by up to 20 mm. Once the patient is repositioned, the physician provides gentle downward traction to deliver the posterior shoulder with the aid of gravity. The all-fours position is compatible with all intravaginal manipulations for shoulder dystocia, which can then be reattempted in this new position. All-fours positioning may be disorienting to physicians who are unfamiliar with attending a delivery in this position. Performing a few “normal” deliveries in this position before encountering a case of shoulder dystocia may prepare physicians for more emergent situations.
MANEUVERS OF LAST RESORT
DOCUMENTATION
Documentation of the management of shoulder dystocia should concentrate on the maneuvers performed and the duration of the event. Terms such as mild, moderate, or severe shoulder dystocia offer little information about the situation or care encountered. Other team members assisting the delivery should be listed, as well as cord pH, if obtained. Specific notation regarding which arm was impacted against the pubis should be made in the event that subsequent nerve palsy develops. The delivery should be reviewed with the parents, and the management and prognosis for any infant palsy should be explained.