
Am Fam Physician. 2012;86(5):451-453
Author disclosure: No relevant financial affiliations to disclose.
A 47-year-old man presented with a three-week history of cramping lower abdominal pain, change in bowel habits, and hematochezia. Symptoms started with constipation and lower abdominal pain. The pain worsened over two to three days, then his bowel movements resumed with improvement in pain. However, his stools were smaller and softer, and contained bloody mucus. A cycle of constipation followed by smaller stools with hematochezia continued. He also had abdominal bloating and excessive flatus, especially in the early morning.
His physical examination, laboratory tests, and routine stool studies were normal. A colonoscopy revealed a 6-cm, firm, tubular, polypoid mass with a wide base at the splenic flexure that filled greater than 75 percent of the colonic lumen (Figure 1). Biopsies of the polyp showed reactive changes, focal fibrosis, and fibrinopurulent debris.

Question
Discussion
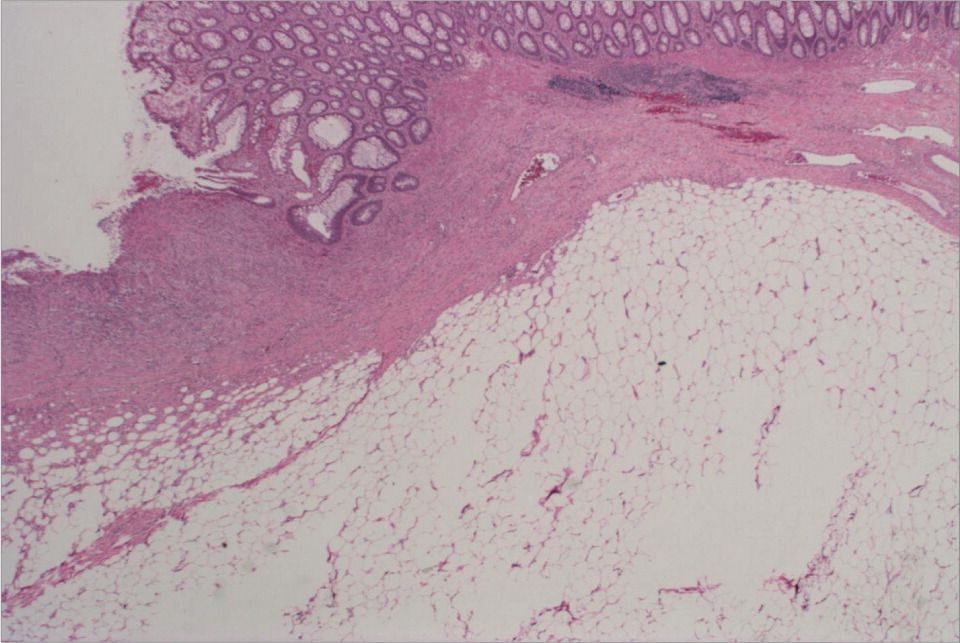
The answer is D: lipoma. An abdominal and pelvic computed tomography scan showed a large mass in the distal transverse colon, which corresponded to the colonoscopic findings and had features suggestive of a lipoma (Figure 2). The histopathologic evaluation of the resected specimen revealed submucosal fat, confirming the diagnosis (Figure 3).

Colonic lipoma is a benign, nonepithelial tumor that is usually detected incidentally. It is the most common submucosal tumor of the colon.1 The prevalence has been estimated at 0.2 to 4.4 percent.2 Symptoms may include abdominal pain, rectal bleeding, altered bowel habits, abdominal distension, anorexia, and weight loss. Although large symptomatic lesions are uncommon, symptoms usually appear when the lipoma is greater than 2 cm in size.3 Lipomas usually have a broad base and a yellowish hue from the underlying fat. Other endoscopic signs include tenting effect (i.e., a tent-like appearance from easy retraction of the overlying mucosa upon grasping with forceps), cushion sign (i.e., a sponge- or pillow-like impression upon probing with forceps), and naked fat sign (i.e., extrusion of yellowish fat after taking repeat biopsies from the same site). Computed tomography and magnetic resonance imaging findings are essentially diagnostic. Computed tomography shows a characteristic low densitometric value consistent with fat and has higher sensitivity for larger lesions than for smaller ones.4 Magnetic resonance imaging shows a signal intensity characteristic of adipose tissue in T1-weighted and fat-suppressing images.5
Adenocarcinoma can present with a change in bowel habits, abdominal pain, and weight loss. The appearance on endoscopy can vary from an indent on a polyp to a fungating mass.1 It usually appears as a hard, large mass with an irregular surface that can be deeply depressed or have superficial ulceration.6 It can also present as an annular lesion causing stenosis or obstruction of the colon.
Colonic adenoma is a premalignant lesion that can be pedunculated or sessile and vary in size. Endoscopically, adenomas are generally reddish with rich vascularization. They can also appear velvety with finger-like projections. The probability of invasive cancer with colonic adenoma is related to the size of the polyp. An adenomatous polyp of greater than 1 cm is a risk factor for cancer, and is a predictor of recurrent high-risk adenomas.7,8
Gastrointestinal stromal tumors can also present with similar symptoms of abdominal pain and rectal bleeding. They are the most common connective tissue tumors in the gastrointestinal tract, but occur more often in the stomach and the small intestine.9 Endoscopically, these tumors present as a bulge in the lumen with normal overlying mucosa or a characteristic central ulceration.
Melanoma metastasizes commonly to the gastrointestinal tract. The most common site of metastasis is the small bowel, followed by the colon and stomach. Primary colonic melanoma is extremely rare because of the absence of embryonic melanocytes in the colon. On endoscopy, colonic melanoma is often pigmented and ranges in size from a small submucosal lesion to a large fungating mass. Diagnosis requires histopathology and immunohistochemistry of the endoscopic biopsies or resected specimen. The prognosis of patients with primary colonic melanoma is better than that of patients with melanoma in other sites. The overall mortality is 47 percent, with one-year and five-year survival rates of 60 percent and 33 percent, respectively.10
| Condition | Characteristics |
|---|---|
| Adenocarcinoma | Hard, large mass with an irregular surface that may be deeply depressed or have superficial ulceration; annular lesions can cause stenosis or obstruction of the colon |
| Adenoma | Premalignant lesion that can be pedunculated or sessile; reddish and velvety with finger-like projections and rich vascularization |
| Lipoma | Broad-based mass with a yellowish hue; tenting effect, cushion sign, and naked fat sign may be present |
| Gastrointestinal stromal tumor | Usually develops in the stomach and the small intestine; normal appearance of the overlying mucosa bulging into the lumen; central ulceration may be present |
| Melanoma | Metastatic lesion that is often pigmented and ranges in size from a small submucosal lesion to a large fungating mass; primary colonic lesions are extremely rare because of the absence of embryonic melanocytes in the colon |
