
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2013;87(8):568-573
Author disclosure: No relevant financial affiliations.
Patients with wrist pain commonly present with an acute injury or spontaneous onset of pain without a definite traumatic event. A fall onto an outstretched hand can lead to a scaphoid fracture, which is the most commonly fractured carpal bone. Conventional radiography alone can miss up to 30 percent of scaphoid fractures. Specialized views (e.g., posteroanterior in ulnar deviation, pronated oblique) and repeat radiography in 10 to 14 days can improve sensitivity for scaphoid fractures. If a suspected scaphoid fracture cannot be confirmed with plain radiography, a bone scan or magnetic resonance imaging can be used. Subacute or chronic wrist pain usually develops gradually with or without a prior traumatic event. In these cases, the differential diagnosis is wide and includes tendinopathy and nerve entrapment. Overuse of the muscles of the forearm and wrist may lead to tendinopathy. Radial pain involving mostly the first extensor compartment is commonly de Quervain tenosynovitis. The diagnosis is based on history and examination findings of a positive Finkelstein test and a negative grind test. Nerve entrapment at the wrist presents with pain and also with sensory and sometimes motor symptoms. In ulnar neuropathies of the wrist, the typical presentation is wrist discomfort with sensory changes in the fourth and fifth digits. Activities that involve repetitive or prolonged wrist extension, such as cycling, karate, and baseball (specifically catchers), may increase the risk of ulnar neuropathy. Electrodiagnostic tests identify the area of nerve entrapment and the extent of the pathology.
Musculoskeletal problems are responsible for up to 20 percent of all visits to primary care offices in the United States.1 Family physicians are often the first to evaluate and treat wrist pain. Wrist pain is traditionally classified as acute pain caused by a specific injury or as subacute/chronic pain not caused by a traumatic event (Tables 1 and 2). Injuries that cause acute pain may result in contusions, fractures, ligament sprains or tears, and instability. Subacute or chronic pain may result from overuse, have neurologic or systemic causes, or be a sequela from an old injury. Patients with these injuries may have a history of repetitive wrist movement, either occupationally or recreationally. The addition of sensory disturbances, such as numbness or tingling, points to nerve involvement.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Anatomic snuffbox swelling, scaphoid tubercle tenderness, and pain with axial pressure on the first metacarpal bone are sensitive but not specific tests for diagnosing scaphoid fractures. | C | 6, 7 |
| If plain radiography results are negative in a suspected scaphoid fracture, then the wrist should be protected in a thumb spica cast with repeat plain radiography in 10 to 14 days or a bone scan one to two days after injury. | C | 4, 5 |
| The Finkelstein test has good sensitivity and specificity for diagnosing de Quervain tenosynovitis. | C | 18, 20 |
| Cause | Clinical presentation | Recommended imaging |
|---|---|---|
| Carpal instability | Trauma, carpal tenderness, audible clunk with radial or ulnar deviation | Radiography with views in radial/ulnar deviation or advanced imaging (CT, MRI, bone scan) |
| Fracture | Trauma, bony tenderness | Radiography or advanced imaging (CT, MRI, bone scan) |
| Joint subluxation | Trauma, instability with movement | Radiography or MRI |
| Ligament tears | Trauma, painful motion | MRI |
| Cause | Clinical presentation | Recommended tests |
|---|---|---|
| Neurologic (ulnar, median, and radial nerve entrapment) | Pain with sensory and possibly motor difficulties | Radiography, electrodiagnostic tests |
| Old trauma (nonunion, avascular necrosis) | Remote history of injury with noimprovement | Plain radiography, magnetic resonance imaging |
| Systemic (rheumatoid arthritis, amyloidosis, gout) | Constitutional symptoms, swelling, constant pain | Complete blood count, erythrocyte sedimentation rate, C-reactive protein level |
| Tendinopathy | Painful movement | Tests usually not needed |
History and physical examination lead to the correct diagnosis in most cases. The location, nature, timing, and quality of the pain are important clues for narrowing the differential diagnosis. In acute wrist injuries, plain radiography should be obtained with anteroposterior, lateral, and oblique views. When the diagnosis remains unclear, further imaging, such as bone scan, ultrasonography, computed tomography, or magnetic resonance imaging (MRI), may help identify the cause. Because nontraumatic wrist pain has a wide differential diagnosis, the patient history should include a review of systems with neurologic or constitutional symptoms, as well as a social history of vocational and recreational activities. The following case studies discuss the background and presentation of three causes of wrist pain, as well as diagnostic tests and strategies.
Case 1. Scaphoid Fracture
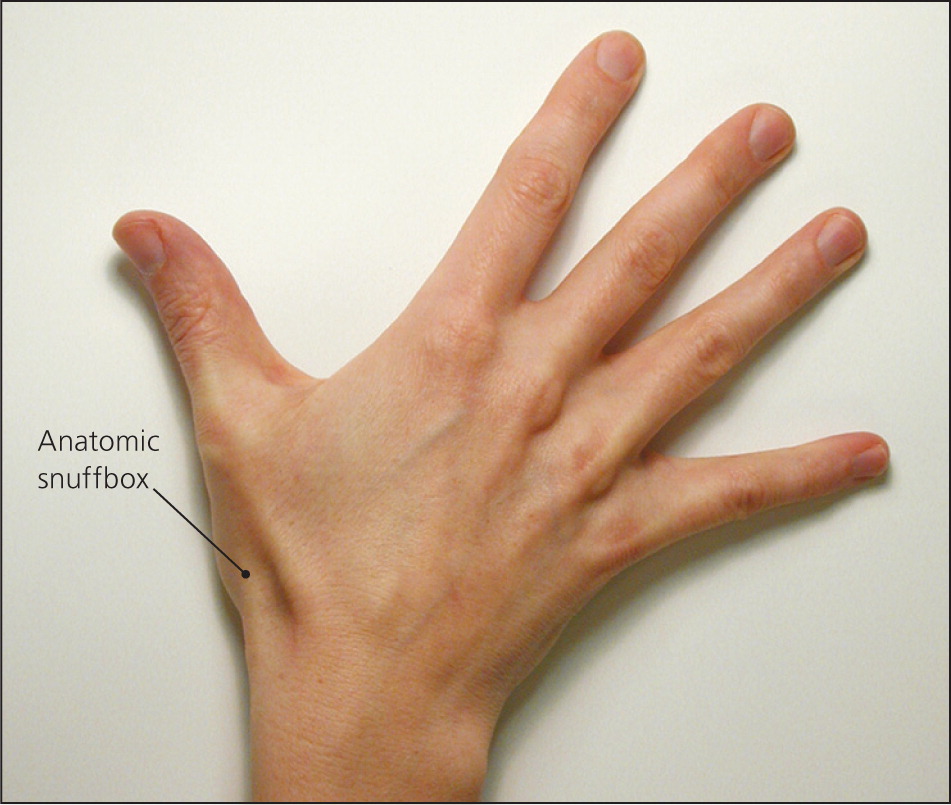
A 21-year-old man presents with dorsal left wrist pain after falling onto his outstretched hand while inline skating. He noted immediate swelling and painful wrist extension. Physical examination reveals soft tissue swelling with limited motion, mostly in extension, secondary to pain. There is bony tenderness along the distal radius as well as the anatomic snuff box. His sensory and vascular examination results are unremarkable.
BACKGROUND
The wrist comprises eight carpal bones (Figure 12 ), but only the lunate and scaphoid articulate with the radius and absorb significant impact during a fall onto an outstretched hand. The scaphoid is the most commonly fractured carpal bone. The primary vascular supply to the scaphoid originates distally from retrograde branches of the distal radial artery, making the proximal pole of the scaphoid relatively avascular and at higher risk of nonunion and avascular necrosis. Fractures of the proximal and distal portions of the scaphoid each account for 20 percent of scaphoid fractures, and the middle portion accounts for the remaining 60 percent.3
The peak incidence of scaphoid fractures occurs at about 15 years of age.4 Because of the weakness of the distal radius compared with the scaphoid, scaphoid fractures are not common in older persons. In young children, the supportive cartilage surrounding the ossific nucleus of the immature scaphoid creates protection, making physeal injuries of the radius more common.
PRESENTATION
The typical history of a patient with a scaphoid fracture is a fall onto an outstretched hand with the wrist dorsiflexed and radially deviated. Most patients with scaphoid fractures present shortly after a fall, but in some cases, the initial pain improves, causing a delayed presentation.
Physical examination may reveal a swollen wrist. Tenderness is usually located dorsally around the distal radius. Patients may have painful wrist extension and loss of grip strength if they present a few days after the injury.
There are no reliable clinical tests to rule out a scaphoid fracture. Swelling of the anatomic snuff box (Figure 25 ) increases the likelihood of a scaphoid facture. The combination of snuff box swelling, scaphoid tubercle tenderness, and pain with axial pressure on the first metacarpal bone has a sensitivity of approximately 100 percent.6 However, the specificity of each test is 9, 30, and 48 percent, respectively.6 Diminished grip strength compared with the contralateral side increases the positive predictive value for a scaphoid fracture.7 The differential diagnosis of a suspected scaphoid fracture is listed in Table 3.
| Diagnosis | Distinguishing features |
|---|---|
| Carpometacarpal dislocation | Radiographic finding of joint space loss(1 to 2 mm) in carpometacarpal joints |
| Distal radial fracture | Radiographic findings of fracture, tenderness to distal radius |
| Lunate fracture | Radiographic findings of fracture, tenderness to lunate |
| Scapholunate tear | Radiographic finding of scapholunate widening (greater than 3 mm) |
DIAGNOSTIC TESTS
Conventional radiography (anteroposterior, lateral, and oblique views) alone can miss up to 30 percent of scaphoid fractures.8 Based on retrospective studies, sensitivity improves if additional views are added (i.e., posteroanterior in ulnar deviation, pronated oblique, and supinated oblique).8 In many cases, repeat radiography is needed in 10 to 14 days to observe sclerosis, which indicates a healing fracture.
If the diagnosis cannot be confirmed with plain radiography, a bone scan or MRI can be performed. Bone scan has a sensitivity near 100 percent but produces false-positive results up to 25 percent of the time.9 MRI within one day after trauma has a sensitivity of 80 percent,10 but late examination (more than 10 days after injury) has a sensitivity and specificity comparable to bone scan.11
DIAGNOSTIC STRATEGY
If a scaphoid fracture is suspected based on history and physical examination, plain radiography should be performed, including specialized views such as a posteroanterior in ulnar deviation and a pronated oblique. If radiography is negative for fracture but clinical suspicion is high, the wrist should be protected in a thumb spica cast with the option of repeat plain radiography in 10 to 14 days or a bone scan one to two days after injury.4,5 If repeat plain radiography is negative but wrist pain persists, MRI should be performed to clarify the diagnosis.
Case 2. Ulnar Neuropathy
A 39-year-old right-handed woman presents with a four-week history of wrist pain and numbness and tingling in her right hand. There is no history of trauma or injury to the neck, elbow, or wrist. She works mostly at a desk job but has not had any changes in her work schedule. Physical examination of the wrist reveals no soft tissue swelling, muscle atrophy, or skin changes. She has painful wrist extension, as well as reproduction of the tingling in her fifth finger with tapping over the pisiform. Grip strength is normal and no other bony tenderness is appreciated.
BACKGROUND
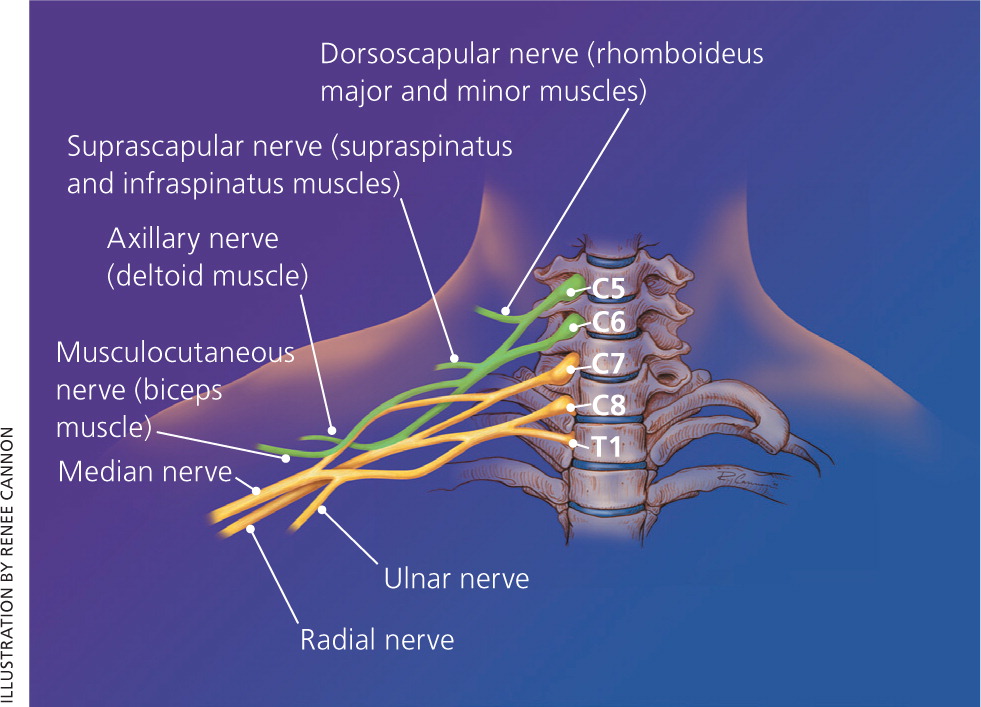
The ulnar nerve originates from the C8 and T1 nerve roots (Figure 312 ), and extends from the medial cord of the brachial plexus through the axilla, innervating the muscles of the forearm and the hand. Proximal to the wrist, dorsal and palmar cutaneous branches split off, whereas the rest of the nerve courses through the Guyon canal (Figure 4) to the palmar surface of the hand. This triangular canal is bordered medially by the pisiform, laterally by the hamate, anteriorly by the tendon of the flexor carpi ulnaris, and posteriorly by the transverse carpal ligament. In the canal, the ulnar nerve splits to a superficial sensory branch, which supplies sensation to the hypothenar eminence, and to a deep motor branch that innervates the hypothenar muscles, adductor pollicis, and flexor pollicis brevis. The ulnar nerve may be compressed anywhere in the Guyon canal, causing motor, sensory, or mixed deficits. Compression is usually caused by ganglion cysts or repetitive trauma.
Ulnar nerve entrapment is the second most common neuropathy of the upper extremity, surpassed only by median nerve entrapment (i.e., carpal tunnel syndrome).13 Although the true incidence of ulnar neuropathy at the wrist is not well documented, it is accepted to be the second most common site after compression at the elbow. Ulnar neuropathies are slightly more common in men than in women. Peak incidence is in men older than 35 years.14
PRESENTATION
The typical presentation in ulnar neuropathy is wrist discomfort with sensory changes in the fourth and fifth digits. Grip weakness may be present in chronic cases. History usually reveals no specific injury. Activities that involve repetitive or prolonged wrist extension, such as cycling, karate, and baseball (specifically catchers) may increase the risk of ulnar neuropathy.15
Physical examination of a patient presenting with these neurologic symptoms should include cervical spine, shoulder, and elbow examinations to rule out a proximal lesion. Reproduction of pain on neck movement could indicate cervical disk disease; pain with shoulder motion could indicate a brachial plexus problem; and reproduction of symptoms with compression of the nerve at the ulnar groove could indicate compression at the elbow. Compression of the ulnar nerve at the Guyon canal should cause weakness of the hypothenar muscles innervated by the deep motor branch and sensory disturbances of the fifth digit innervated by the superficial sensory branch.
Clinical tests include a positive Tinel sign on percussion of the ulnar nerve over the Guyon canal, as well as a positive Phalen sign (maximum passive flexion of the wrist for more than one minute) with paresthesias in the fourth and fifth fingers. Unlike in carpal tunnel syndrome, sensitivity and specificity of these tests for ulnar neuropathy at the wrist are not known. The differential diagnosis of suspected ulnar neuropathy at the wrist is listed in Table 4.
| Diagnosis | Distinguishing features |
|---|---|
| Brachial plexopathy | History of shoulder/arm pain, motor weakness of upper extremity |
| Cervical radiculopathy | History of neck pain, forearm symptoms (e.g., pain, numbness, tingling) |
| Ulnar neuropathy at the elbow | Elbow pain |
| Wrist fracture | Traumatic injury, positive radiographic findings |
DIAGNOSTIC TESTS
Plain radiography evaluates wrist anatomy well, and can identify fractures, dislocations, or soft tissue masses that may have led to nerve compression.
Ultrasonography of peripheral nerves is helpful in identifying compressive etiologies of nerve injury and in visualizing structural nerve changes. It is noninvasive, relatively inexpensive, and well tolerated by patients.
Electromyography and nerve conduction studies can be helpful in identifying the area of entrapment and documenting the extent of the pathology. Motor and sensory conduction velocities are more useful in acute entrapments, whereas electromyography is a better choice for chronic neuropathies because it shows axonal degeneration more clearly. The sensitivity and specificity of these electrodiagnostic tests in the primary care setting are unknown because existing studies are limited to a small number of patients with known neuropathy.
MRI can detect abnormalities of the ulnar nerve, flexor tendons, vascular structures, and the transverse carpal ligament around the Guyon canal. Neurogenic edema can be seen as early as 24 to 48 hours after denervation compared with electromyography, in which changes after denervation are not seen for one to three weeks.16 Imaging criteria for neuropathy on MRI are not well defined, and several studies have found MRI abnormalities in healthy, asymptomatic patients.17
DIAGNOSTIC STRATEGY
If ulnar neuropathy is suspected, plain radiography should be ordered first. If no obvious mass or lesion is found, electrodiagnostic tests should be ordered to localize the lesion, measure its severity, and aid in the prognosis. In the setting of inconclusive or nonlocalizing electrodiagnostic test results, ultrasonography or MRI may be useful.
Case 3. De Quervain Tenosynovitis
A 31-year-old woman presents with several months of worsening radial left wrist pain that started insidiously. She denies any specific trauma. She has no numbness or tingling in the wrist, hand, or fingers. Her pain worsens with gripping and grasping, and with picking up her nine-month-old daughter. Physical examination reveals no discoloration and minimal soft tissue swelling along the radial styloid and anatomic snuff box. There is soft tissue tenderness about the anatomic snuff box and radial styloid. She has limited motion of the thumb, with pain mostly in extension and abduction. Her sensory and vascular examinations are unremarkable.
BACKGROUND
Two major dorsal tendons of the thumb are involved: the extensor pollicis brevis and the abductor pollicis longus (Figure 5). [ corrected] These tendons comprise the lateral border of the anatomic snuffbox, with the extensor pollicis longus medially and the scaphoid bone at the bottom. The two tendons have similar function in bringing the thumb into radial abduction. These tendons run in a synovial sheath in the first extensor compartment of the hand. Inflammatory changes in the sheath and tendons result in a tenosynovitis. Recurrent or persistent inflammation may result in stenosing tenosynovitis.
PRESENTATION
The typical presentation includes subacute radial wrist pain at the thumb base and into the distal radius. In retrospect, patients may identify a new or repetitive hand-based activity as the cause, but the etiology often is idiopathic. De Quervain tenosynovitis is more common in women, particularly those 30 to 50 years of age.18 New mothers are especially noted to have this problem from picking up a child.19
Physical examination may reveal a minimally swollen wrist. Tenderness is usually located over the radial tubercle and sometimes around the soft tissues of the anatomic snuff box. Thumb motion is invariably painful. Neurovascular examination should be unremarkable. The Finkelstein test is confirmatory because it has good sensitivity and specificity.18,20 It is performed by making a fist over the thumb and then moving the hand into ulnar deviation, which passively stretches the thumb tendons over the radial styloid.20,21 A grind test of the thumb, which is performed by axial compression and slight rotation of the metacarpophalangeal joint, should be negative in those with de Quervain tenosynovitis but positive in those with first carpometacarpal osteoarthritis. The differential diagnosis of suspected de Quervain tenosynovitis is listed in Table 5.
| Diagnosis | Distinguishing features |
|---|---|
| Ganglion cyst | Visual appearance of cyst-like structure |
| Osteoarthritis of the first extensor compartment | Radiographic findings of osteoarthritis |
| Radial nerve entrapment of the forearm | Electromyographic findings |
| Wrist extensor tendinopathy | Clinical examination findings |
DIAGNOSTIC TESTS
The diagnosis is clinical based on history and examination. In cases where osteoarthritis of the carpometacarpal joint is considered, pain relief with diagnostic lidocaine (Xylocaine) injection of the first extensor compartment excludes arthritic cause. Radiography, electromyography/nerve conduction studies, blood tests, and MRI or ultrasonography may be used to evaluate for alternative diagnoses.
DIAGNOSTIC STRATEGY
If the history and examination are consistent, no further diagnostic testing is needed. For suspicion of fracture or arthritis, radiography is an appropriate first step. If suspected, radial nerve abnormalities may be ruled out with electromyography or nerve conduction studies. If there is concern for infectious tenosynovitis, a complete blood count and measurement of inflammatory markers, such as erythrocyte sedimentation rate and C-reactive protein levels, are appropriate. If the patient does not respond to treatment or if the diagnosis is in question, an MRI or musculoskeletal ultrasonography may be ordered to further evaluate the first extensor compartment.19,22
Data Sources: A PubMed search was completed in Clinical Queries using the key terms scaphoid fracture, ulnar neuropathy, and de Quervain's. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were Essential Evidence Plus, the Cochrane database, the National Guideline Clearinghouse, and UpToDate. Search date: August 2011.
