A more recent article on childhood eye examinations is available.
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2013;88(4):241-248
Author disclosure: No relevant financial affiliations.
Vision screening in children is an ongoing process, with components that should occur at each well-child visit. The purpose is to detect risk factors and visual abnormalities that necessitate treatment and to identify those patients who require referral to an ophthalmologist skilled in examining children. Screening can reveal conditions commonly treated in primary care and can aid in discussion of visual concerns with parents or caregivers. Vision screening begins with a review of family and personal vision history to identify risk factors requiring referral, including premature birth, Down syndrome, cerebral palsy, and a family history of strabismus, amblyopia, retinoblastoma, childhood glaucoma, childhood cataracts, or ocular or genetic systemic disease. Visual acuity measurement and external ocular examination are performed to recognize refractive error, childhood glaucoma, and various ocular conditions. Evaluation of fixation and alignment can identify amblyopia or strabismus. Red reflex examination is used to diagnose retinoblastoma, childhood cataracts, and other ocular abnormalities.
Vision screening in children is an ongoing process with different components occurring at each well-child visit (Table 11). It can reveal conditions commonly treated in primary care and can aid in discussion of visual concerns with parents or caregivers. The purpose is to detect treatable visual abnormalities and to identify those patients who require referral for a comprehensive evaluation by an ophthalmologist skilled in examining children.1 Referral is indicated after the first screening failure.1 The American Academy of Family Physicians and the U.S. Preventive Services Task Force recommend vision screening at least once in all children three to five years of age (B recommendation).2,3 [corrected] See the videos showing an eye examinationation in a preschool-aged child and an eye examination in an infant/toddler.
Components of the eye examination in a preschool-aged child.
Components of the eye examination in an infant/toddler.
| Clinical recommendation | Evidence rating | References | Comment |
|---|---|---|---|
| Measurement of visual acuity using an eye chart is recommended in children starting at three years of age. | C | 1, 3–5 | — |
| Ocular alignment should be assessed during vision screening in children to identify strabismus and amblyopia. | C | 3, 14, 21 | Multiple studies, but with various design flaws, giving conflicting results; expert opinions vary |
| General consensus is that corneal light reflex and fix and follow should be checked starting by three months of age, and more specific alignment testing is beneficial after about three years of age | |||
| To identify opacities, red reflex examination should be performed starting at birth. | C | 1, 4, 5, 23 | — |
| Method | Indications for referral | Recommended age | ||||
|---|---|---|---|---|---|---|
| Newborn to six months | Six months and until the child is able to cooperate for subjective visual acuity measurement | Three to four years | Four to five years | Every one to two years after five years of age | ||
| Red reflex examination | Absent, white, dull, opacified, or asymmetric | X | X | X | X | X |
| External inspection | Structural abnormality (e.g., ptosis) | X | X | X | X | X |
| Pupillary examination | Irregular shape, unequal size, poor or unequal reaction to light | X | X | X | X | X |
| Fix and follow test | Failure to fix and follow | Cooperative infant older than three months | X | |||
| Corneal light reflex text | Asymmetric or displaced | X | X | X | X | |
| Instrument-based screening* | Failure to meet screening criteria | X | X | X | ||
| Cover test | Refixation movement | X | X | X | ||
| Distance visual acuity† (monocular) | 20/50 or worse in either eye | X | X | X | ||
| 20/40 or worse in either eye | X | X | ||||
| Worse than three of five optotypes on 20/30 line, or two lines of difference between the eyes | X | |||||
History
Vision screening begins with a thorough vision history taken at the patient's first visit.4 A personal or family history of risk factors for eye and vision problems that require referral is particularly important. These risks include premature birth, Down syndrome, cerebral palsy, and a family history of strabismus, amblyopia, retinoblastoma, childhood glaucoma, childhood cataracts, or ocular or genetic systemic disease.1 At each visit the physician should ask about the child's visual interactions and any eye or vision problems.5
Visual Acuity
The eye examination begins with a measurement of visual acuity. Assessing visual acuity in infants and toddlers involves evaluation of fix and follow behavior (discussed later). The American Academy of Ophthalmology recommends the use of an eye chart by three years of age.1 Picture charts (Lea or Allen) or matching charts (HOTV) can be used in preliterate children, and letter charts (Snellen) can be used in literate children (Figure 16). Each eye should be tested independently and the opposite eye occluded to discourage peeking. The Multi-Ethnic Pediatric Eye Disease Study provided updated norms for visual acuity in children two and a half to six years of age (Table 2).7 Most children do not have 20/20 vision until after six years of age,7 but at any age, visual acuity should be approximately equal between the eyes. The American Academy of Ophthalmology recommends referral for children five years or older who have monocular vision worse than three of five optotypes (letters, numbers, symbols) on the 20/30 line, or two lines of difference between the eyes, because this may be an indicator of amblyopia (decreased vision in one eye compared with the other).1,8
| Age (months) | Norms |
|---|---|
| 30 to 35 | Approximately 20/60 (6/20) or better |
| 36 to 47 | 20/50 (6/15) or better |
| 48 to 59 | 20/40 (6/12) or better |
| 60 to 72 | Approximately 20/30 (6/10) or better |
External Ocular Examination
Vision screening continues with examination of the external portion of the eye, including the eyelids, orbits, conjunctiva, sclera, cornea, and iris. Using a light, the examiner should inspect for excessive tearing, watery or purulent discharge, photosensitivity, conjunctival injection, and gross structural abnormalities. Lacrimal duct obstruction is the most common cause of persistent eye discharge in infants. This is recognized when pressure over the lacrimal sac produces mucus in an eye that otherwise has constant clear tearing.5,9 It can be treated with lacrimal duct massage and, if there are signs of infection, with topical antibiotics.5 Close follow-up for symptom resolution is recommended because childhood glaucoma has a similar presentation (although tearing in childhood glaucoma is usually accompanied by redness and corneal edema).5,9 Childhood glaucoma can also present with corneal clouding, photosensitivity, and enlarged eyes. If there is any concern for childhood glaucoma, prompt referral is indicated to prevent blindness.
Pupillary Response
Pupillary response should be assessed using a bright light to examine each pupil for direct and consensual response. When achievable, accommodative response should be tested. The room should be darkened before declaring a response absent. Pupils are measured for size and symmetry in both light and darkness. Anisocoria (greater than 1-mm difference in pupil size) in the presence of an otherwise negative eye examination can be a normal finding in up to 20% of the population.10,11 However, it may also be a sign of amblyopia or of sympathetic (e.g., Horner syndrome) or parasympathetic (e.g., third nerve palsy) abnormalities, which warrant further investigation.12
Fixation and Alignment
Ocular fixation should be evaluated routinely. Children as young as six weeks should have some response to an examiner's face.13 By two months of age, a child should be able to fix and follow an object.13 If strong binocular fix and follow is not seen by three months of age, referral is recommended.5
Ocular alignment should be assessed to identify strabismus (abnormal eye alignment).3,14 Strabismus may be caused by abnormal innervation of the eye muscles or by other conditions such as amblyopia, cataracts, or retinoblastoma. Prior to two months of age, it is common for one or both eyes to temporarily deviate out of alignment. This deviation should resolve by four months of age and warrants referral if persistent.13,15 Simple observation for obvious deviation of one eye relative to the other will alert the physician to potential problems. Corneal light reflex testing in all children, and basic cover tests in children three years and older, can expose subtle findings.
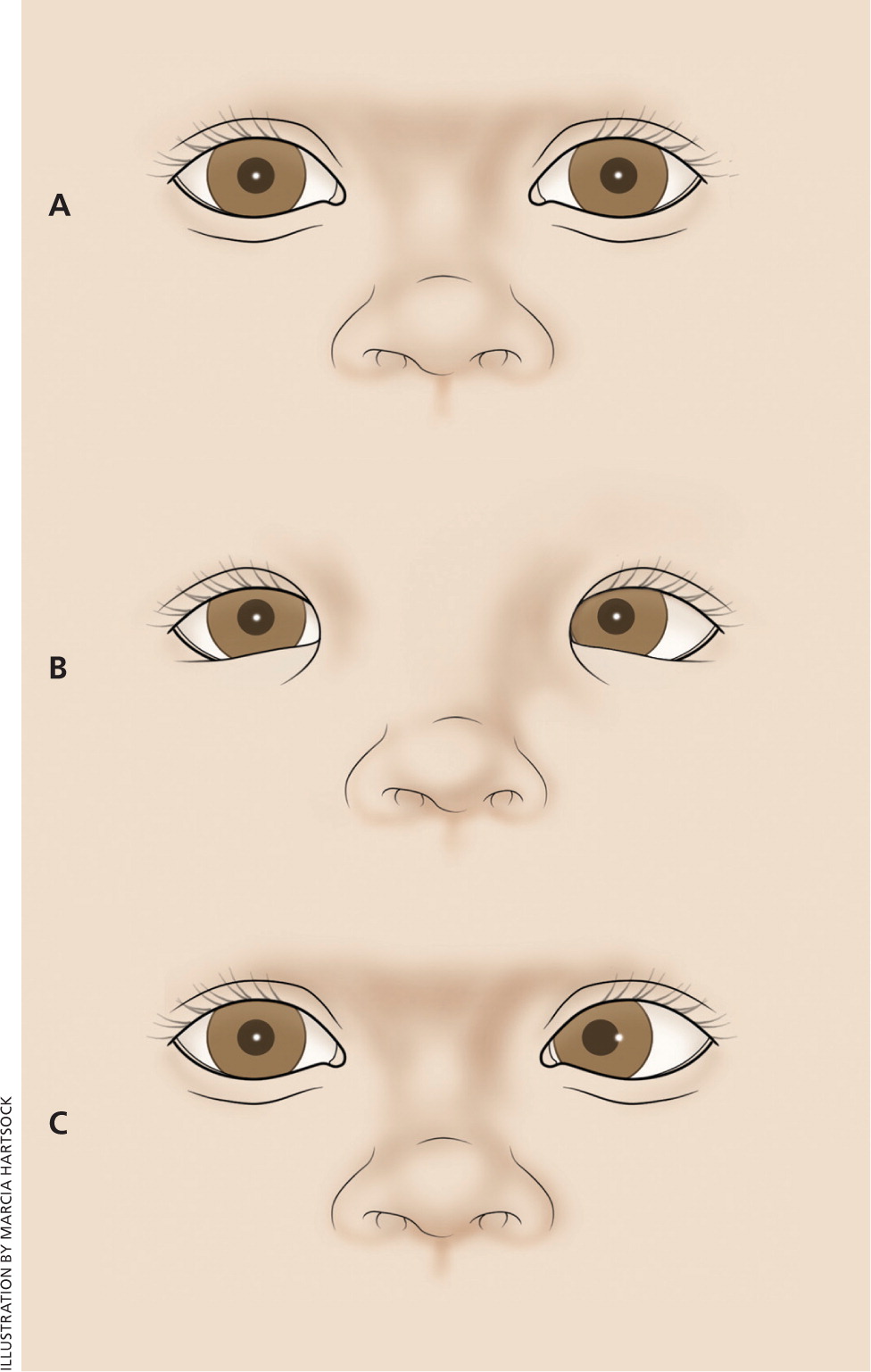
Corneal Light Reflex
In a corneal light reflex test, the child's attention is attracted to a target (a light or a brightly colored object), while a light in front of the child is directed at the child's eyes. The light's reflection will be symmetric in each pupil by four to six months of age in patients with normally aligned eyes1 (Figure 2). A wide nasal bridge or epicanthal folds may give the appearance of eye deviation; however, on closer examination, the light reflection will be found to be symmetric. This is pseudostrabismus, a normal variant (Figure 3).
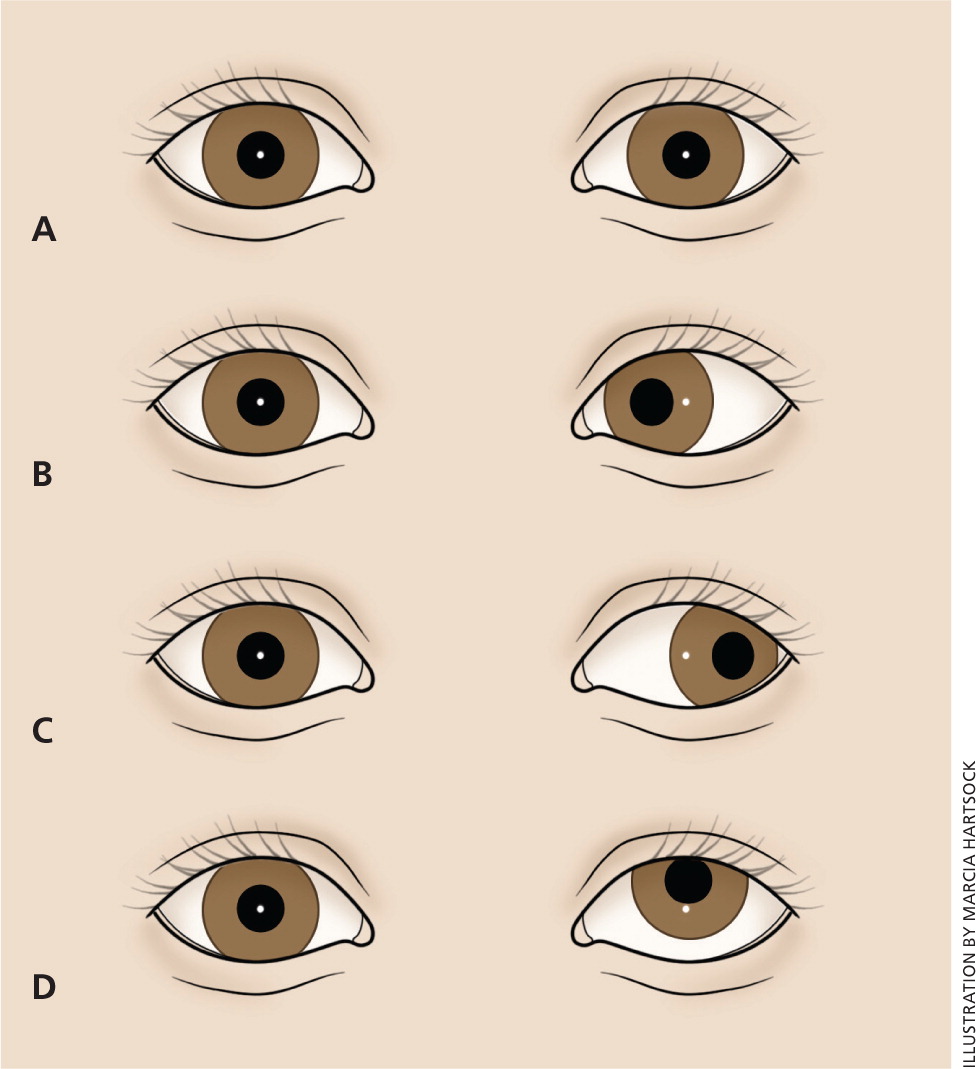
Cover, Cover-Uncover, and Alternate Cover Tests
Alignment is further screened with several tests using a cover over one eye (Figure 4). In the cover test, the child's attention is attracted to a target. The vision of one eye is then occluded. The tested (uncovered) eye is observed for movement from a deviated position to one that fixes on the target (a sign of tropia, also called manifest strabismus). The untested eye is then uncovered and the tested eye is observed again for any drift out of alignment.
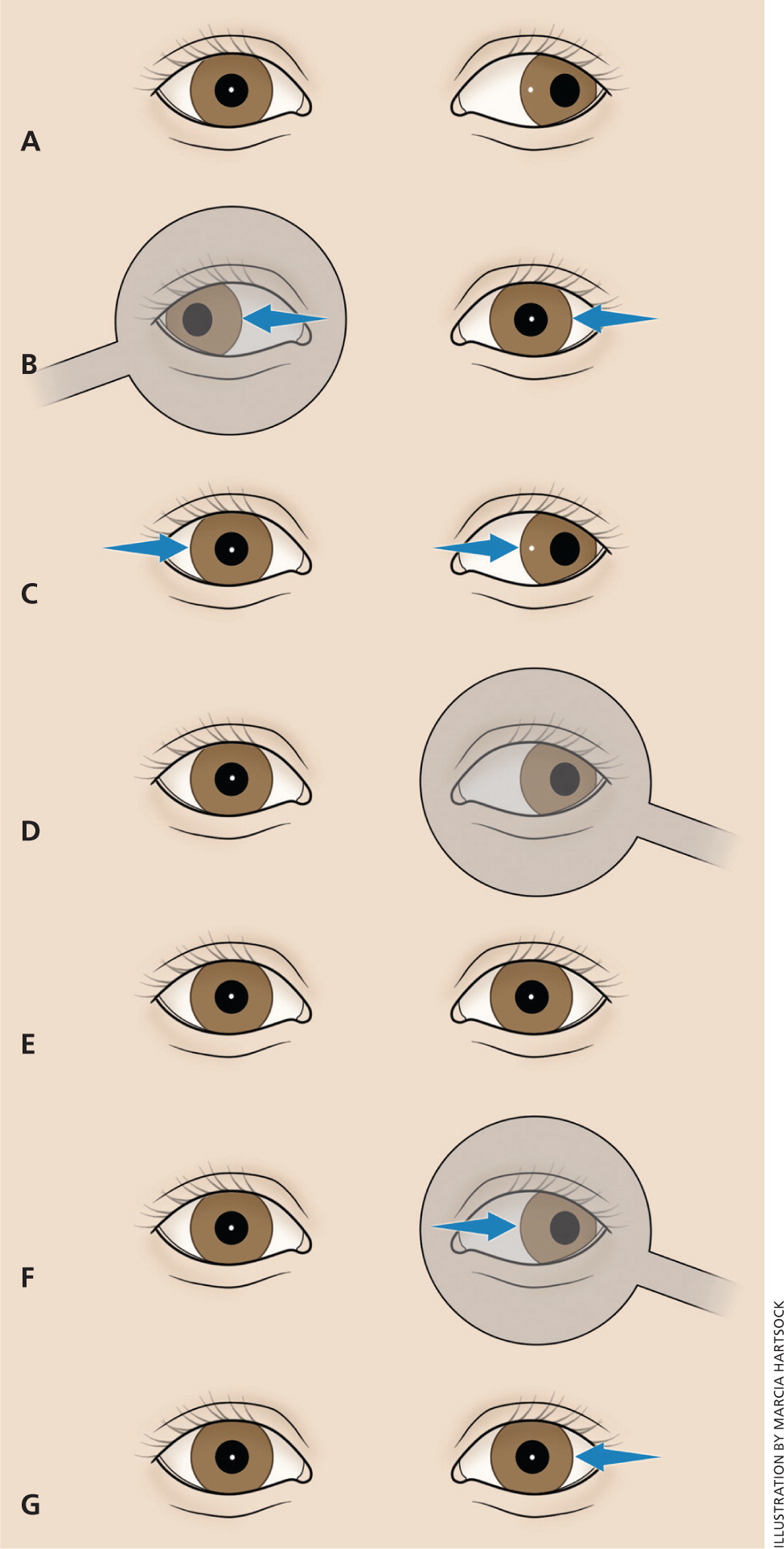
In the cover-uncover test, a cover is placed over one eye for one to two seconds while the child's attention is called to the target. The cover is then removed rapidly, and the previously covered eye is observed for any movement from a deviated position back to fixation on the target (a sign of phoria, also called latent strabismus). Minimal phoria is a normal variant.
The alternate cover test can reveal a hidden phoria. The cover is held over one eye for a few seconds, then moved rapidly over the other eye and held for a few seconds, then moved back to cover the first eye. This is repeated several times, and each time the cover is moved, the previously covered eye is observed for any “refixation” from a deviated to a normal position.
The cover, cover-uncover, and alternate cover tests should be performed on both eyes, focusing first on a near object and then on a far object. The tests should be repeated three times to check for reproducibility. If any strabismus is detected, the patient should be referred. In some children, strabismus may be present only intermittently, especially when a child is tired. If the parent or caregiver reports eye deviation, the child should be referred for further evaluation, even if the deviation is not seen in the office.16
When both visual acuity and ocular alignment are assessed, the physician should be aware of the possibility of amblyopia. Amblyopia results from any condition that decreases the vision in an eye, leading to suppression by the brain of the image from that eye. Etiologies include strabismus, infantile cataracts, neurologic disease, eye injury, retinal lesions, or a significant refractive error between the eyes (anisometropia).
Although there is no one test that will detect all cases of amblyopia, visual acuity measurement, screening for alignment, and red reflex examination all help identify amblyopia. In very young children, amblyopia should be suspected if the child seems to consistently resist the covering of one eye more than the covering of the other eye.17 A child who is reported to tilt his or her head frequently may be compensating for amblyopia or other ocular abnormalities.18,19 Rarely, the presenting symptom of amblyopia is nystagmus, which always warrants referral.13
If left untreated, amblyopia can lead to permanent vision loss.20 Amblyopia may be particularly difficult to detect in preliterate children. A study from the Netherlands showed that even in the setting of widespread, early vision screening, amblyopia was often not recognized until school age.21 Treatment of the various causes of amblyopia is most effective when started early. However, improvement can be seen even when treatment is not started until the teenage years. Referral is warranted whenever the condition is recognized.22
Red Reflex
Starting with the neonatal evaluation, ocular pathology such as ocular alignment, asymmetric refractive errors, cataracts, and retinal abnormalities can be assessed with the red reflex examination4 (Figure 5). The ophthalmoscope is used in a darkened room to view each red reflex individually 12 to 18 inches (approximately 30 to 45 cm) from the patient's eyes, and then both red reflexes simultaneously at a distance of 2 to 3 feet (approximately 0.6 to 0.9 meters). A symmetric orange-red light should reflect from each fundus; however, the tint may vary to light gray with darkly pigmented eyes. Any abnormal finding (e.g., asymmetry of color or occurrence of dark or white spots) is a reason for referral to an ophthalmologist5,23 (Figure 6). The only exception would be the presence of mucus in the tear film that is observed as a mobile opacity that resolves with blinking.1,23
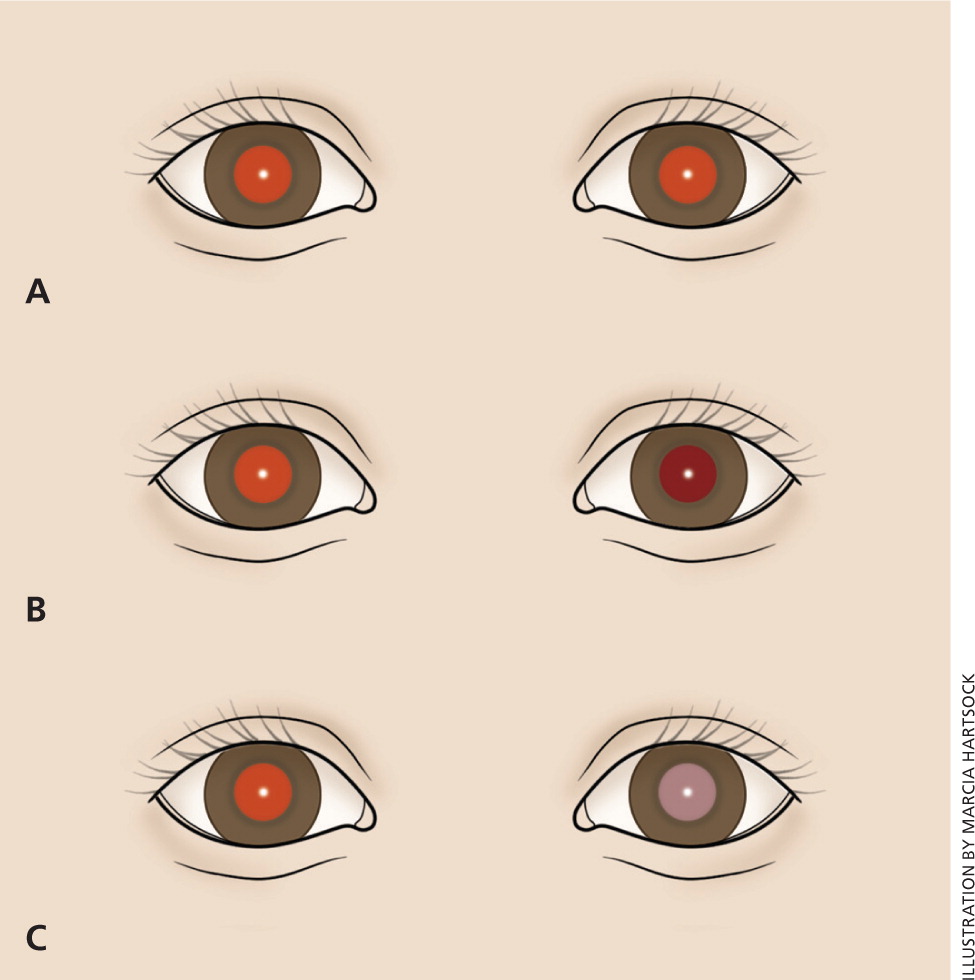

One of the concerning outcomes of an abnormal red reflex examination is the identification of a retinoblastoma. This neuroblastic tumor is the most common primary intraocular malignancy and the seventh most common malignancy of childhood, occurring in about one in 20,000 children.13,24 Leukokoria (or white pupil) is the most common finding and is often discovered by a family member who does not realize its serious etiology.13,24 There are a multitude of alternate presenting signs for retinoblastoma, including strabismus, tearing, red eye, iris discoloration, corneal clouding, hyphema, and glaucoma. Retinoblastoma is fatal without treatment, although there is potential for a more than 90% cure rate with prompt recognition and management. Because preserving the eye and functional vision is related to the magnitude of the disease, any abnormal finding should lead to a prompt referral. Although less than 25% of patients with retinoblastoma have a family history of the disease, the presence of a family history necessitates a referral regardless of the physical examination findings.13,24,25
Another potentially serious cause of an abnormal red reflex examination is a cataract. Cataracts may be unilateral or bilateral, may or may not have related signs (e.g., musculoskeletal or neurologic symptoms), may be progressive or nonprogressive, and can occur congenitally or develop during infancy. Most are idiopathic.24,26 Estimates of incidence are one to six per 10,000 live births. Up to one-third of cataracts are inherited, and they may be autosomal dominant, autosomal recessive, or X-linked.13,24,26 A family history of childhood cataracts necessitates an ophthalmologist's evaluation.23 Examination may show dull, irregular, or absent red reflex, or leukokoria. Urgent referral for treatment is recommended because prognosis is improved with earlier intervention, although treatment varies depending on the density and location of the opacity.13,25,26
A common cause of an asymmetric red reflex is a refractive error in one or both eyes. This condition could lead to a serious outcome of amblyopia if left untreated. It can be corrected with glasses provided early in life.8
Based on the potentially serious nature of abnormal red reflex findings, eye examinations should occur with each scheduled well-child visit, starting in the neonatal nursery. After three years of age, the funduscopic examination may complement the red reflex examination by providing direct information about the optic nerve and vasculature of the retina. It is possible to perform in a cooperative patient who can be preoccupied enough with a toy to fixate on it; however, not all sources agree on when to integrate the funduscopic examination into the complete childhood eye examination.5,8,23
Data Sources: We began with an evidence report from Essential Evidence Plus (search date: March 8, 2011) that used the key terms amblyopia, esotropia, and retinoblastoma, and included POEMs, Cochrane reviews, and practice guidelines. Our librarian provided searches of PubMed and http://www.guidelines.gov (search date: April 18, 2011) using the key terms nystagmus, vision screening, infant cataracts, and pediatric glaucoma. We searched PubMed multiple times during the spring of 2011 and January 2012 using various key terms from the article. We also used http://www.primeanswers.org to search PubMed (search date: April 18, 2011) for vision screening within ACP Journal Club, Clinical Evidence, Cochrane Database of Systematic Reviews, FPIN Clinical Inquiries, NEJM Clinical Practice, and U.S. Preventive Services Task Force. In addition, we searched Dynamed (search date: July 3, 2011) for vision screening and UpToDate (search dates: July 11, 2011, and January 10 through 18, 2012).