
A more recent article on arthropod bites and stings is available.
Am Fam Physician. 2013;88(12):841-847
Related letter: Identifying Erythema Migrans Rash in Patients with Lyme Disease
Author disclosure: No relevant financial affiliations.
The phylum Arthropoda includes arachnids and insects. Although their bites typically cause only local reactions, some species are venomous or transmit disease. The two medically important spiders in the United States are widow spiders (Latrodectus), the bite of which causes intense muscle spasms, and the brown recluse (Loxosceles), which may cause skin necrosis. Widow bites usually respond to narcotics, benzodiazepines, or, when necessary, antivenom. Most recluse bites resolve uneventfully without aggressive therapy and require only wound care and minor debridement. Tick bites can transmit diseases only after prolonged attachment to the host. Treatment of clothing with permethrin and proper tick removal greatly reduce the risk of infection. Ticks of medical importance in the United States include the black-legged tick, the Lone Star tick, and the American dog tick. The prophylactic use of a single dose of doxycycline for Lyme disease may be justified in high-risk areas of the country when an attached, engorged black-legged tick is removed. Bites from fleas, bedbugs, biting flies, and mosquitoes present as nonspecific pruritic pink papules, but the history and location of the bite can assist with diagnosis. Flea bites are usually on ankles, whereas mosquito bites are on exposed skin, and chigger bites tend to be along the sock and belt lines. Antihistamines are usually the only treatment required for insect bites; however, severe mosquito reactions (skeeter syndrome) may require prednisone. Applying insect repellent containing diethyltoluamide (DEET) 10% to 35% or picaridin 20% is the best method for preventing bites.
Arthropods comprise a vast invertebrate phylum that includes arachnids (those with eight legs, such as spiders, mites, and ticks) and insects (those with six legs [subphylum Hexapoda], such as mosquitoes, gnats, and flies). Most arachnid and insect bites are summertime nuisances, but several species' bites are toxic and others are vectors of disease. This article focuses on spider, mite, tick, and insect bites of medical importance.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Consider methicillin-resistant Staphylococcus aureus infection in a patient presenting with a suspected spider bite. Many purported spider bites are bacterial pyodermas or other skin conditions. | C | 2, 3 |
| Black widow spider bites should be treated with intravenous benzodiazepines for muscle spasm and narcotics for pain. | C | 4, 5 |
| Black widow antivenom should be reserved for patients with significant pain that has not responded to conventional treatment with benzodiazepines and narcotics. | C | 4, 5 |
| Wound cleansing and minor debridement are the mainstays for managing necrotic brown recluse bites. | C | 6–8 |
| Tick bites should be treated with prophylactic doxycycline (200 mg in a single dose) only when an engorged black-legged tick is acquired in a high-risk area for Lyme disease. Antibiotics are effective if given within 72 hours of tick removal. | C | 11 |
| Antihistamines are the best first-line therapy for most insect bites. | C | 21 |
Spiders
Only two spiders in the United States are considered medically important with regard to bites: the black widow (Latrodectus mactans) and the brown recluse (Loxosceles reclusa). Most spiders are harmless. Many suspected spider bites are actually caused by other conditions, such as methicillin-resistant Staphylococcus aureus infection.1 In one series of 600 suspected bites, 80% were attributable to other causes, such as pyoderma.2 Without a witnessed bite and species identification, other possibilities should be considered2,3 (Table 13 ). Most genuine bites are single lesions that require only cleansing, cold packs, and a tetanus vaccination booster.
| Other arthropod bites and stings |
| Mosquitoes, flies, ticks, mites, fleas, bees, wasps, scorpions |
| Infectious diseases |
| Chagas disease |
| Cutaneous anthrax |
| Dermatomycosis |
| Erysipelas |
| Furuncles or boils (including community-acquired methicillin-resistant Staphylococcus aureus infection) |
| Herpes simplex virus infection |
| Herpes zoster virus infection |
| Impetigo |
| Lyme disease (erythema migrans) |
| Pyoderma gangrenosum |
| Southern tick-associated rash illness |
| Sporotrichosis |
| Syphilis |
| Other conditions |
| Allergic contact dermatitis |
| Angioneurotic edema |
| Autoimmune vasculitides |
| Chemical burns |
| Chemical contact dermatitis |
| Diabetic ulcers |
| Erythema multiforme |
| Lymphomatoid papulosis |
| Poison ivy, oak, or sumac |
| Venous stasis ulcers |
WIDOW SPIDERS
Widow spiders can be found worldwide. Of the five species in the United States, the three most common are L. mactans in the East, Latrodectus hesperus in the West, and Latrodectus variolus in the North. The female L. mactans is black, usually with a classic red hourglass mark on the ventral abdomen (Figure 1). Introduced brown widow spiders (Latrodectus geometricus) are found in the South, and have an orange or yellow hourglass mark and milder venom. Widow spiders typically reside in yard debris, and their bite, which feels like a pinprick, is associated with recent outdoor activity. Widow venom contains α-latrotoxin, which provokes a massive presynaptic release of acetylcholine. After a person has been bitten, crampy muscle spasms usually occur within an hour in the chest (upper extremity bites) or the abdomen (lower extremity bites). The pain may be intense enough to mimic myocardial infarction or acute abdomen, but it is rarely life threatening and typically resolves within 48 to 72 hours.4 Nausea, weakness, local or generalized diaphoresis, and facial edema may occur. Clark's grading system is used to assess bites and determine management (Table 2).4 Grade 3 bites, especially in children or older persons, may warrant antivenom and hospital admission to reduce potential complications.

| Grade | Description |
|---|---|
| 1 | Asymptomatic; local pain at envenomation site; normal vital signs |
| 2 | Muscular pain in envenomated extremity; extension of muscular pain to abdomen (if bitten on lower extremity) or chest (if bitten on upper extremity); local diaphoresis of envenomation site or involved extremity; normal vital signs |
| 3 | Generalized muscular pain in back, abdomen, and chest; diaphoresis remote from envenomation site; abnormal vital signs, such as hypertension (systolic blood pressure > 140 mm Hg or diastolic blood pressure > 90 mm Hg) and tachycardia (pulse > 100 beats per minute); nausea and vomiting; headache |
Treatment of widow bites usually involves intravenous benzodiazepines for muscle spasms and narcotics for pain. These have largely replaced intravenous calcium gluconate 10% in clinical practice.4 An effective antivenom (L. mactans [equine]) may be considered up to 48 hours after a bite, but should be used only if severe pain persists after standard therapy. One amp of antivenom is added to 100 mL normal saline and slowly infused for 15 minutes (1 mL per minute), with the remainder given over one to two hours.5 Serum sickness may be a complication.
BROWN RECLUSE SPIDERS
Brown recluse, or “fiddleback,” spiders are found in the south-central United States (Figure 2) and South America. Brown recluse spiders typically have an inverted violin-shaped marking on their dorsal thorax (Figure 3). They are unusual in that they have three pairs of eyes instead of the traditional four pairs. In contrast to widow bites, recluse bites usually occur indoors because the spiders often hide in piles of clothing or in dark places behind furniture. Although the bite may be minimally painful, a tender erythematous halo soon develops, followed by central necrosis in about 40% of cases and scarring in 13% of cases.6 Skin grafting is rarely required.

Venom from brown recluse spiders contains sphingomyelinase D, which is thought to be responsible for neutrophil activation and skin necrosis (necrotic arachnidism). Systemic symptoms are rare in the United States, but persons may develop hemolysis, coagulopathy, and a measles-like toxic erythema rash, which responds to prednisone. A Loxosceles antivenom is manufactured in South America but is unavailable in the United States.
Management of recluse bites is controversial, and there are no published clinical trials to guide therapy. Most experts believe that overly aggressive bite management does more harm than good, and cutting out the bite site to prevent necrosis is contraindicated.3 Good wound care and minor debridement usually suffice. Antihistamines have been suggested as an unproven adjunctive therapy that poses little risk to the patient.7 Although controversial, dapsone at a dosage of 50 to 100 mg twice per day for 10 days has been recommended for severe bites based on its theoretical ability to prevent neutrophil degranulation/necrosis.8 If this treatment is used, glucose-6-phosphate dehydrogenase (G6PD) testing should be performed because dapsone may cause hemolysis in patients with G6PD deficiency.
Ticks
Ticks are vectors of multiple diseases (Table 3).9,10 There are two major types of ticks: hard ticks (Ixodidae) have shield-like scutum with the head visible from above, whereas the less medically important soft ticks (Argasidae) have a leathery skin with the head invisible from above. Hard ticks latch onto their hosts and feed for days, whereas soft ticks are localized in animal nests. Hard ticks inhabit brushy fields and tall grass where they await potential hosts.
| Bite source | Associated diseases |
|---|---|
| Ticks | |
| American dog tick (Dermacentor variabilis) | Q fever (Coxiella burnetii) |
| Rocky Mountain spotted fever (Rickettsia rickettsii); most common in the southeastern United States | |
| Tick paralysis (toxin) | |
| Tularemia (Francisella tularensis) | |
| Black-legged or deer tick (Ixodes scapularis) and western black-legged tick (Ixodes pacificus) | Babesiosis (Babesia microti), a parasitic disease mimicking malaria in the northeastern and upper midwestern United States (I. scapularis only) |
| Human granulocytic anaplasmosis (formerly human granulocytic ehrlichiosis) | |
| Lyme disease (Borrelia burgdorferi) | |
| Brown dog tick (Rhipicephalus sanguineus) | Q fever |
| Rocky Mountain spotted fever | |
| Lone Star tick (Amblyomma americanum) | Alpha-gal sensitivity (red meat allergy) |
| Human monocytic ehrlichiosis caused by Ehrlichia chaffeensis | |
| Q fever | |
| Southern tick-associated rash illness or Masters disease, a southern Lyme disease–like illness with rash, previously thought to be caused by Borrelia lonestari (etiology still uncertain) | |
| Tularemia | |
| Pacific Coast tick (Dermacentor occidentalis) | 364D rickettsiosis (Rickettsia phillipi, proposed), newly identified in California |
| Rocky Mountain spotted fever | |
| Tularemia | |
| Rocky Mountain wood tick (Dermacentor andersoni) | Colorado tick fever (orbivirus) |
| Potential vector of Powassan encephalitis and Q fever | |
| Rocky Mountain spotted fever | |
| Tick paralysis (toxin) | |
| Tularemia | |
| Soft ticks (Ornithodoros spp.), such as Pajaroello tick (Ornithodoros coriaceus) | Pajaroello tick bites of the southwestern United States are associated with pain and localized necrosis, probably mediated by a toxin |
| Relapsing fever (Borrelia spp.) in the western United States | |
| Woodchuck tick (Ixodes cookei) | Powassan virus (Powassan encephalitis), a tick-borne encephalitis found in northern United States and Canada |
| Mites and fleas | |
| House mouse mites (Liponyssoides sanguineus) | Rickettsial pox (Rickettsia akari) |
| Various fleas | Cat flea typhus or flea-borne spotted fever (Rickettsia felis) |
| Cat-scratch disease (Bartonella henselae), transmitted between cats by fleas | |
| Murine typhus (Rickettsia typhi) | |
| Plague (Yersinia pestis), endemic to western United States with occasional human cases from contact with rodent fleas | |
| Tularemia |
Tick nymphs and adults feed on different hosts, and humans are usually incidentally involved. In the case of the deer or black-legged tick (Ixodes scapularis; Figure 4), nymphs feed on mice and adults feed on deer. Both stages of ticks can transmit Lyme disease, which manifests as a characteristic bull's-eye rash (i.e., erythema migrans) at the site of an infected bite (Figure 5). Ixodes ticks are also capable of transmitting babesiosis, which is a malaria-like protozoal illness, and human granulocytic anaplasmosis.9


Prophylactic treatment for Lyme disease with a single 200-mg dose of doxycycline is recommended only if the following criteria are met: the tick is identifiable as I. scapularis, it has been attached for more than 36 hours (engorged), antibiotics can be administered within 72 hours of removal, the local infection rate of the vector is greater than 20%, and the patient can tolerate doxycycline.11 For an interactive Lyme disease map showing reported cases across the United States from 2001 to 2011, visit http://www.cdc.gov/lyme/stats/maps/interactivemaps.html.
The American dog tick (Dermacentor variabilis) is a common hard tick that may transmit Rocky Mountain spotted fever and tularemia (Figure 6). The Lone Star tick (Amblyomma americanum) of the southeast United States is identifiable by a white spot on its shield (Figure 7). It is a potential vector of human monocytic ehrlichiosis, tularemia, Q fever, and southern tick-associated rash illness, which is a Lyme-like disease that may produce a circular rash, headache, and fever. The infectious agent has not been conclusively identified but generally responds to doxycycline.9 Recently, Lone Star tick bites have provoked a persistent allergy to red meat (and cetuximab [Erbitux]) caused by immunoglobulin E antibodies to galactose-alpha-1,3-galactose, better known as alpha-gal. Persons who are bitten develop delayed hives or, in some cases, anaphylaxis after eating beef, pork, or lamb.12 Tick paralysis, which results from gravid female bites, is a toxin-mediated ascending paralysis that generally resolves after tick removal.


Tick bites can be prevented by spraying clothes with permethrin, a synthetic insecticide. In one study, persons wearing permethrin-treated socks and sneakers received almost 75% fewer bites than persons wearing untreated items.13 Applying diethyltoluamide (DEET)-containing repellents to exposed skin can provide additional benefit. Tucking pants into socks, wearing hats, and performing a daily tick check also reduce exposure.
Ticks should be removed with a pair of forceps (or tick-removal device), grasping the tick as close to the skin as possible. A gentle, steady pull, perpendicular to the skin, without twisting, usually dislodges the tick without leaving mouthparts behind.14 Applying viscous lidocaine 2% (Xylocaine) is another option, but is often too slow to be satisfactory.15 Petroleum jelly, alcohol, nail polish remover, and lit matches should not be used because they may cause ticks to regurgitate infectious material into the bite.14
Mites and Chiggers
Mites are tiny eight-legged arthropods that, in their larval form, cause itchy bites and sometimes transmit diseases, such as scrub typhus (overseas) and rickettsial pox. The six-legged larval form is called the chigger, also known as harvest bug or red bug (Trombicula spp.). The larvae appear on the skin as tiny red specks that crawl until they reach constrictive clothing; thus, bites tend to be located at belt or sock lines. Occasionally, the penis is severely affected, resulting in summer penile syndrome.16 The resulting welts are significantly larger than the size of the chigger and are caused by an allergic reaction to the saliva. Chiggers do not burrow into the skin.
The same precautions used for ticks are effective for chiggers. Immediate showering is likely to dislodge most of them. Bites can be treated with antihistamines, cold compresses, calamine lotion, or rubbing alcohol. No treatment has been demonstrated to be particularly effective.
Fleas
Fleas (Siphonaptera) are wingless jumping insects that feed on blood. Flea bites are usually from dog or cat fleas (Ctenocephalides), which attack humans when their preferred hosts are unavailable. For example, a common scenario involves a vacationing family returning home to fleas after their pets have been in a kennel. Typical flea bites are pruritic ankle papules, but other sites may be involved after coming in contact with infested areas. The human flea species (Pulex irritans) is usually associated with poor hygiene. Flea bites may transmit plague, tularemia, cat-scratch disease, and cat flea typhus (Rickettsia felis).
Bedbugs
Temperate bedbugs (Cimex lectularius), tropical bedbugs (Cimex hemipterus), and bat bugs (Cimex pilosellus) are oval, flat insects measuring about 5 mm in length. Bedbugs hide inside box springs, under mattresses, and behind headboards where they may survive for up to one year without feeding.17 Examination of infested bedding typically reveals reddish stains and a characteristic sweet smell sometimes likened to coriander. A previous American Family Physician article provides additional information on identifying and eradicating bedbugs (https://www.aafp.org/afp/2012/1001/p653.html).18
Diptera
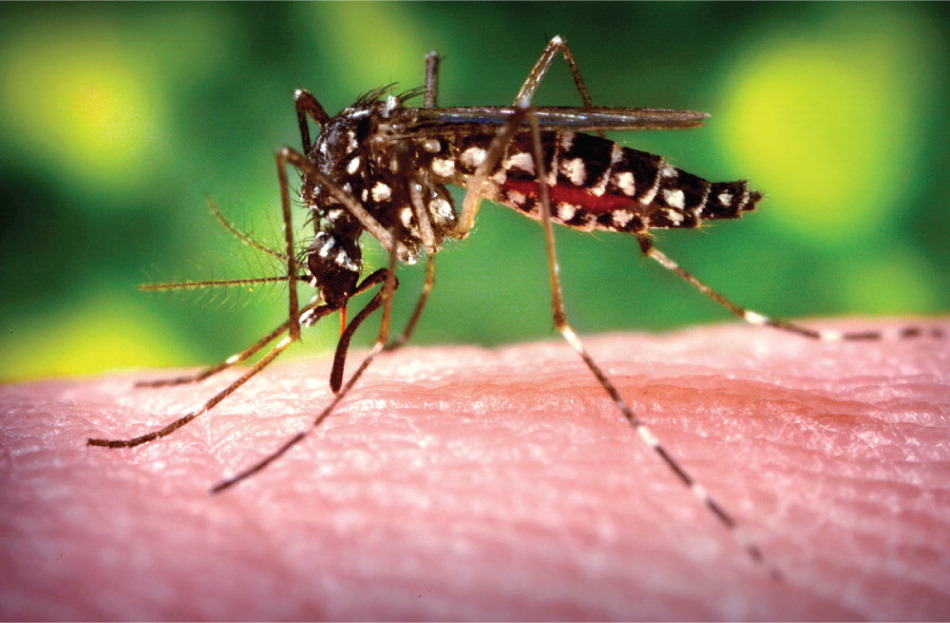
Diptera (two-winged insects) include mosquitoes, midges, gnats, and flies, all of which can act as disease vectors (Table 4).19 Mosquito bites can spread West Nile virus, certain types of encephalitis, and, more recently, dengue fever, with cases reported in Key West, Fla., Hawaii, and Texas.20 The vector for dengue fever is Aedes aegypti (Figure 8). Most mosquito bites in the United States provoke nothing more than an itchy welt. Typical bites appear as pruritic pink papules, often with a central punctum. Sensitivity varies widely, however, and some persons experience a severe or prolonged reaction. The more extreme cases have been termed skeeter syndrome, which describes an intense hypersensitivity reaction with fever related to allergens in mosquito saliva.21 Antihistamines and prednisone are used to treat this condition.
| Insect | Comments |
|---|---|
| Biting midge (Culicoides) | Also called no-see-ums, punkies, “flying teeth,” sand flies, no-no's; all attracted to still air and low light |
| Black fly (Simuliidae) | Onchocerciasis vectors in Africa; day-feeding flies; mostly near streams; attracted to dark moving objects |
| Horsefly and deer fly (Tabanidae) | Also called gadflies; like to bite on warm overcast days; deer fly of western Africa (Chrysops; vector of Loa loa) |
| Louse fly (Hippoboscidae) | Sheep and deer keds (Melophagus, Lipoptena); pigeon fly (Pseudolynchia) |
| Mosquito (Culicidae) | Vectors of malaria (Anopheles), yellow fever (Aedes or Haemagogus), Japanese encephalitis (Culex), dengue fever (Aedes), chikungunya (Aedes), West Nile virus (Culex), Rift Valley fever (Culex), St. Louis encephalitis (Culex), eastern equine encephalitis (Aedes, Culiseta), western equine encephalitis (Culex, Aedes), and various other arboviruses (arthropod-borne viruses) |
| Sandfly (Lutzomyia in the Americas or Phlebotomus in the Eastern hemisphere) | Vectors of leishmaniasis; moth-like small flies residing in damp shade; bite at night |
| Snipe fly (Symphoromyia) | Day-biters that cause occasional severe allergic reactions (western United States) |
| Stable fly (Stomoxys) | Day-biters stimulated to bite by thunderstorms; resemble house flies but rest with head higher |
| Tsetse fly (Glossina) | Vectors of African trypanosomiasis; day-biters; often penetrate clothing |
Prevention
Bite prevention strategies include avoiding high-risk sites (e.g., marshes, pools of standing water) and avoiding going outdoors at certain times of day (after dusk); wearing protective light-colored clothing, ideally treated with permethrin; and employing insect screens or bed nets. Bug zappers are ineffective and destroy beneficial insects. The most effective approach is applying insect repellents containing DEET 35% or picaridin 20%. Combination repellent-sunscreen preparations are not recommended because they have differing durations of effectiveness.22 Repellents should be applied after applying sunscreen, because applying DEET first increases skin absorption.23
DEET is the most effective repellent and is safe if guidelines are followed. Optimal concentrations are 10% to 35%, and a sustained-release 35% preparation (Ultrathon) is effective for up to 12 hours.24 Although higher concentrations may provide longer protection, those greater than 50% should be avoided because of minimal additional benefit and increased skin absorption.24,25 DEET 10% to 30% may be used in children older than two months if an adult supervises application and if it is not applied to the lips or hands.25,26 DEET is considered safe during pregnancy after the first trimester.26,27
Picaridin lacks the oiliness and odor of DEET, and does not damage synthetic fabrics, although it has a shorter duration of action.28 It is not approved for children younger than two years. Most natural repellents are less effective, but the best of these is oil of lemon eucalyptus, which contains the active ingredient p-menthane-3,8-diol.25 Unreliable alternatives that are not recommended include ultrasonic devices, oral thiamine, garlic, and wristbands impregnated with repellents.25
Data Sources: A literature search was performed in PubMed, Cochrane Database of Systematic Reviews, the Centers for Disease Control and Prevention, the Medical Letter, and Essential Evidence Plus. Initial search terms were insect bites, spider bites, bedbugs, ticks, tick-borne diseases, mites, and fleas. Secondary searches were conducted on STARI (southern tick-associated rash illness), Powassan encephalitis, and other vector-borne diseases. References were also identified from UpToDate and other pertinent review articles on these topics. Search dates: August and September 2011, and July 31, 2013.
