
A more recent article on common foot fractures is available.
Am Fam Physician. 2016;93(3):183-191
Author disclosure: No relevant financial affiliations.
Foot fractures are among the most common foot injuries evaluated by primary care physicians. They most often involve the metatarsals and toes. Patients typically present with varying signs and symptoms, the most common being pain and trouble with ambulation. Diagnosis requires radiographic evaluation, although emerging evidence demonstrates that ultrasonography may be just as accurate. Management is determined by the location of the fracture and its effect on balance and weight bearing. Metatarsal shaft fractures are initially treated with a posterior splint and avoidance of weight-bearing activities; subsequent treatment consists of a short leg walking cast or boot for four to six weeks. Proximal fifth metatarsal fractures have different treatments depending on the location of the fracture. A fifth metatarsal tuberosity avulsion fracture can be treated acutely with a compressive dressing, then the patient can be transitioned to a short leg walking boot for two weeks, with progressive mobility as tolerated after initial immobilization. A Jones fracture has a higher risk of nonunion and requires at least six to eight weeks in a short leg non–weight-bearing cast; healing time can be as long as 10 to 12 weeks. Great toe fractures are treated with a short leg walking boot or cast with toe plate for two to three weeks, then a rigid-sole shoe for an additional three to four weeks. Lesser toe fractures can be treated with buddy taping and a rigid-sole shoe for four to six weeks.
Primary care physicians are often the first clinicians patients see for foot injuries, and fractures are among the most common foot injuries they evaluate.1 This article will highlight some common foot fractures that can be managed by primary care physicians.
Foot fractures range widely in severity, prognosis, and treatment. Healing rates also vary considerably depending on the age of the patient and comorbidities. Thus, this article provides general healing ranges for each fracture.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The use of musculoskeletal ultrasonography may be considered to diagnose subtle metatarsal fractures. | C | 9, 10 |
| Nondisplaced or minimally displaced (less than 3 mm) fractures of the second to fifth metatarsal shafts with less than 10° of angulation can be treated conservatively with a short leg walking boot, cast shoe, or elastic bandage, with progressive weight bearing as tolerated. | C | 2–4, 6 |
| The Ottawa Ankle and Foot Rules should be used to help determine whether radiography is needed when evaluating patients with suspected fractures of the proximal fifth metatarsal. | A | 14, 16 |
| Early surgical management of a Jones fracture allows for an earlier return to activity than nonsurgical management and should be strongly considered for athletes or other highly active persons. | B | 2, 6, 13, 20–22 |
| Nondisplaced or minimally displaced (less than 2 mm) fractures of the lesser toes with less than 25% joint involvement and no angulation or rotation can be managed conservatively with buddy taping or a rigid-sole shoe. | C | 6, 24, 25 |
The fractures reviewed in this article are summarized in Table 1. These include metatarsal fractures, which account for 35% of foot fractures.2,3 About 80% of metatarsal fractures are nondisplaced or minimally displaced, which often makes conservative management appropriate.4 In adults and children older than five years, fractures of the fifth metatarsal are most common, followed by fractures of the third metatarsal.5 Toe fractures, the most common of all foot fractures, will also be discussed.
| Fracture type | Radiographic evaluation | Acute treatment | Definitive treatment | Follow-up imaging | Indications for orthopedic referral |
|---|---|---|---|---|---|
| First metatarsal shaft | Three-view foot series | Posterior splint; non–weight bearing; follow-up in three to five days | Short leg walking cast with toe plate or boot for six weeks; follow-up every two to four weeks; healing time of six weeks | Repeat radiography at one week and again at four to six weeks | Open fractures; fracture-dislocations; intra-articular fractures; fractures with displacement or angulation |
| Lesser metatarsal shaft | Three-view foot series | Posterior splint; non–weight bearing; follow-up in three to five days | Short leg walking boot or cast for six weeks; follow-up every two to four weeks; healing time of six weeks | Repeat radiography at one week and again at four to eight weeks | Open fractures; fracture-dislocations; multiple metatarsal fractures; displacement > 3 to 4 mm in the dorsoplantar plane; angulation > 10° in the dorsoplantar plane |
| Fifth metatarsal tuberosity | Three-view foot series with attention to the oblique view | Compressive dressing; ambulate as tolerated; follow-up in four to seven days | Short leg walking boot for two weeks, with progressive mobility and range of motion as tolerated; follow-up every two to four weeks; healing time of four to eight weeks | Repeat radiography at six to eight weeks to document healing | Displacement > 3 mm; step-off > 1 to 2 mm on the cuboid articular surface; fracture fragment that includes > 60% of the metatarsal-cuboid joint surface |
| Proximal fifth metatarsal (Jones) | Three-view foot series with attention to the oblique view | Posterior splint; non–weight bearing; follow-up in three to five days | Short leg non–weight-bearing cast for six to eight weeks; cast removal and gradual weight bearing and activity if radiography shows healing at six to eight weeks, or continue immobilization for four more weeks if no evidence of healing; healing time of six to 12 weeks | Repeat radiography at one week for stability and at the six- to eight-week follow-up; if no healing at six to eight weeks, repeat radiography at the 10- to 12-week follow-up | Displacement > 2 mm; 12 weeks of conservative therapy ineffective with nonunion revealed on radiography; athletes or persons with high activity level |
| Great toe | Three-view foot series or dedicated phalanx series | Short leg walking boot; ambulate as tolerated; follow-up in seven days | Short leg walking boot or cast with toe plate for two to three weeks, then may progress to rigid-sole shoe for additional three to four weeks; follow-up every two to four weeks; healing time of four to six weeks | Repeat radiography at one week if fracture is intra-articular or required reduction | Fracture-dislocations; displaced intra-articular fractures; nondisplaced intra-articular fractures involving > 25% of the joint; physis (growth plate) fractures |
| Lesser toes | Three-view foot series or dedicated phalanx series | Buddy taping and rigid-sole shoe; ambulate as tolerated; follow-up in one to two weeks | Buddy taping and rigid-sole shoe for four to six weeks; follow-up every two to four weeks; healing time of four to six weeks | Repeat radiography at one week if fracture is intra-articular or required reduction | Displaced intra-articular fractures; angulation > 20° in dorsoplantar plane; angulation > 10° in the mediolateral plane; rotational deformity > 20°; nondisplaced intra-articular fractures involving > 25% of the joint; physis fractures |
Metatarsal Shaft Fractures
HISTORY
Metatarsal shaft fractures most commonly occur as a result of twisting injuries of the foot with a static forefoot, or by excessive axial loading, falls from height, or direct trauma.2,3,6 Patients may have varying histories, ranging from an ill-defined fall to a remote injury with continued pain and trouble ambulating. Most patients with acute metatarsal fractures report symptoms of focal pain, swelling, and difficulty bearing weight.
PHYSICAL EXAMINATION
Examination of the metatarsals should include palpation of the metatarsal base, shaft, and head, as well as examination of the proximal tarsometatarsal and distal metatarsophalangeal joints. Adjacent metatarsals should be examined, and neurovascular status should be assessed.
There is typically swelling, ecchymosis, and point tenderness to palpation at the fracture site. Bony deformity is often subtle or absent. A positive metatarsal loading test, which involves manual axial loading of the metatarsal, may exacerbate the pain and help differentiate a fracture from a soft tissue injury.3
IMAGING
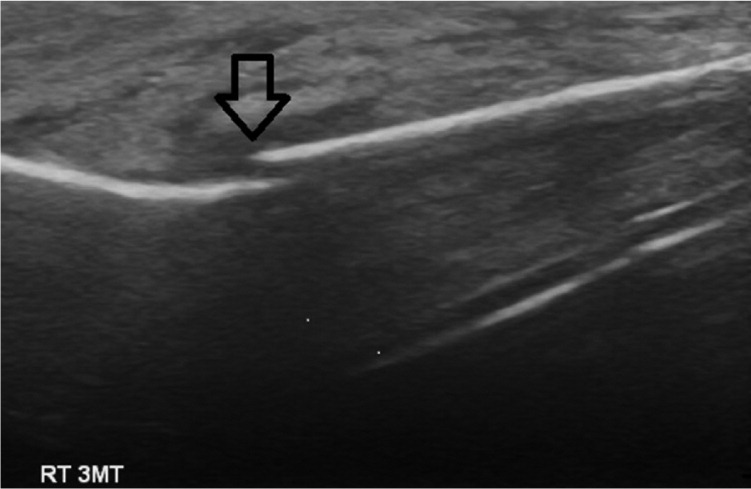
A standard foot series with anteroposterior, lateral, and oblique views is sufficient to diagnose most metatarsal shaft fractures, although diagnostic accuracy depends on fracture subtlety and location.7,8 However, musculoskeletal ultrasonography can provide a quick bedside assessment without radiation exposure that accurately assesses overt and subtle nondisplaced fractures. Recent studies have demonstrated that musculoskeletal ultrasonography and traditional radiography have comparable accuracy, sensitivity, and specificity in the diagnosis of foot and ankle fractures9,10 (Figure 1).
MANAGEMENT
Nondisplaced acute metatarsal shaft fractures generally heal well without complications. Minimally displaced (less than 3 mm) fractures of the second to fifth metatarsal shafts (Figure 2) and fractures with less than 10° of dorsoplantar angulation in the absence of other injuries can generally be managed in the same manner as nondisplaced fractures.2–4,6 Initial management includes immobilization in a posterior splint (Figure 311 ), use of crutches, and avoidance of weight-bearing activities. Patients should be instructed to apply ice, elevate the foot above heart level, and use analgesics as needed.


Follow-up should occur within three to five days to allow for reduction of soft tissue swelling. At the first follow-up visit, radiography should be performed to assure fracture stability. If stable, the patient can be transitioned to a short leg walking cast or boot3,6 (Figures 411 and 5). The choice of immobilization device depends on the patient's ability to ambulate with the device with minimal to no pain. There is evidence that transitioning to a walking boot and then to a rigid-sole shoe (Figure 6) at four to six weeks, with progressive weight bearing as tolerated, results in improved functional outcomes compared with cast immobilization, with no differences in healing time or pain scores.12



ORTHOPEDIC REFERRAL
For acute metatarsal shaft fractures, indications for surgical referral include open fractures, fracture-dislocations, multiple metatarsal fractures, intra-articular fractures, and fractures of the second to fifth metatarsal shaft with at least 3 mm displacement or more than 10° angulation in the dorsoplantar plane. Indications for referral of patients with first metatarsal fractures are different because the first metatarsal has a vital role in weight bearing and arch support. Referral is indicated for patients with first metatarsal fractures with any displacement or angulation.
Proximal Fifth Metatarsal Fractures
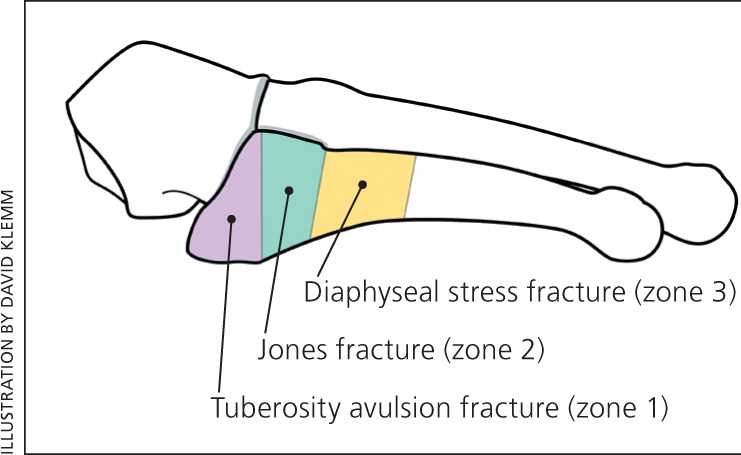
The fifth metatarsal has the least cortical thickness of all the metatarsals.13 There are multiple strong ligamentous and capsular attachments surrounding the proximal fifth metatarsal; these allow stresses to be directed through this portion of the bone.13 Classically, fractures of the proximal fifth metatarsal can be classified based on anatomic location into one or more of three zones (Figure 7).3
HISTORY
Patients with a proximal fifth metatarsal fracture often present after an acute inversion of the foot or ankle. Patients have localized pain, swelling, and inability to bear weight on the lateral aspect of the foot.
PHYSICAL EXAMINATION
Examination should consist of a neurovascular evaluation and palpation of the foot and ankle. There is typically focal tenderness, swelling, and ecchymosis at the base of the fifth metatarsal. Patients usually cannot bear full weight and sometimes will ambulate only on the medial aspect of the foot.
IMAGING
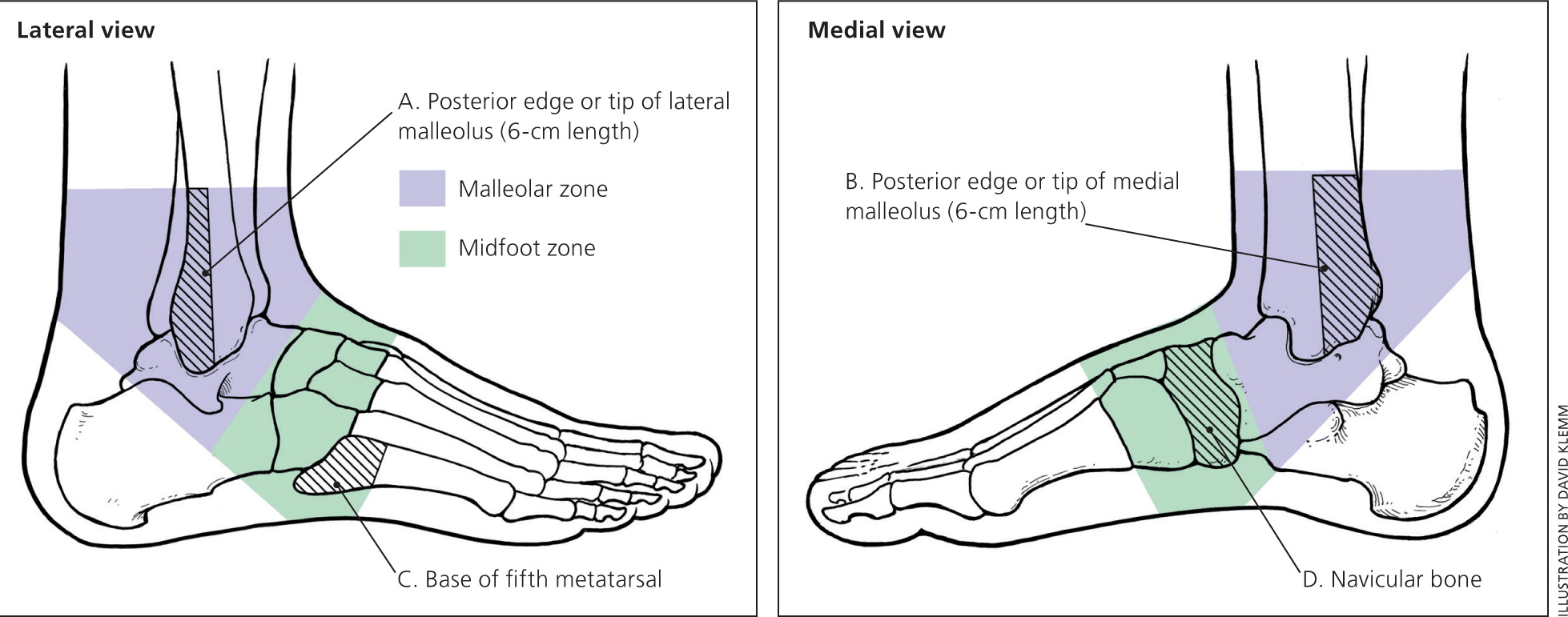
The Ottawa Ankle and Foot Rules should be applied when examining patients with suspected fractures of the proximal fifth metatarsal to help decide whether radiography is needed14 (Figure 815 ). Foot radiography is required if there is pain in the midfoot zone and any of the following: bone tenderness at point C (base of the fifth metatarsal) or D (navicular), or inability to bear weight immediately after the injury and at the time of examination.14 When used properly, the Ottawa Ankle and Foot Rules have a sensitivity of 99% and specificity of 58%, with a positive likelihood ratio of 2.4 and a negative likelihood ratio of 0.02 for detecting fractures. These rules have been validated in adults and children.16 If radiography is indicated, a standard foot series with anteroposterior, lateral, and oblique views is sufficient to make the diagnosis.
If a fracture is present, it will typically be one of two types: a tuberosity avulsion fracture or a Jones fracture (i.e., proximal fifth metatarsal metadiaphyseal fracture). Tuberosity avulsion fractures are generally found in zone 1 and do not extend into the joint between the fourth and fifth metatarsal bases (Figures 7 and 9). Jones fractures are located in a “watershed” area for blood supply (zones 2 and 3) and have high rates of delayed union and nonunion17 (Figure 10).


MANAGEMENT: TUBEROSITY AVULSION FRACTURES

Minimally displaced (less than 3 mm) avulsion fractures typically require immobilization and support with a short leg walking boot. Evidence has shown that, depending on symptoms, short leg walking boots are superior to short leg walking casts.18,19 Immobilization in a cast or boot is typically only needed for two weeks, with progressive ambulation and range of motion thereafter as tolerated. Follow-up visits should be scheduled every two weeks, and healing time varies from four to eight weeks.3,6 Follow-up radiography is typically required only at six to eight weeks to document healing, or earlier if the patient has persistent localized pain or continued painful ambulation at four weeks.2,3,6
MANAGEMENT: JONES FRACTURES
Initial management of a Jones fracture includes a posterior splint and avoidance of weight-bearing activity, with follow-up in three to five days. After that, nonsurgical treatment options include six to eight weeks of short leg non–weight-bearing cast with radiographic follow-up to document healing at six to eight weeks.2,6,20 If evidence of healing is present (callus formation and lack of point tenderness) at that time, weight-bearing activity can progress gradually, along with physical therapy and rehabilitation. If no healing has occurred at six to eight weeks, avoidance of weight-bearing activity should continue for another four weeks.2,6,20 Typical length of immobilization is six to 10 weeks, and healing time is typically up to 12 weeks.
For athletes and other highly active persons, evidence shows earlier return to activity with surgical management; therefore, surgery is recommended.13,21,22 In contrast, patients treated with nonsurgical techniques should be counseled about longer healing time and the possibility that surgery may be needed despite conservative management.2,13,20–22
ORTHOPEDIC REFERRAL
Patients with fifth metatarsal tuberosity avulsion fractures should be referred to an orthopedist if there is more than 3 mm of displacement, if step-off is greater than 1 to 2 mm on the cuboid articular surface, or if a fragment includes more than 60% of the metatarsal-cuboid joint surface. Patients with Jones fractures should be referred if there is more than 2 mm of displacement, if conservative therapy is ineffective after 12 weeks of immobilization and radiography reveals nonunion, or if the patient is an athlete or is highly active.2,13,20–22
Toe Fractures
Toe fractures are the most common fractures of the foot.23,24 Most fractures involve minimal displacement and are treated nonsurgically. Lesser toe fractures are about twice as common as great toe fractures.23,24 The great toe has an increased role in weight bearing and balance; thus, injury to the great toe is associated with higher morbidity.6,24
The primary goals of treating toe fractures include reestablishing and maintaining alignment, regaining range of motion, and preventing complications. In an analysis of 339 toe fractures, 95% involved less than 2 mm of displacement and all fractures were managed conservatively with good outcomes.25
HISTORY
The most common mechanisms of injury are axial loading (stubbing) or crush injury. Patients typically present with pain, swelling, ecchymosis, and difficulty with ambulation. Hyperflexion or hyperextension injuries most commonly lead to spiral or avulsion fractures. Spiral fractures often lead to rotation or shortening, and transverse fractures lead to angulation.6
PHYSICAL EXAMINATION
Physical examination findings typically include tenderness to palpation, swelling, ecchymosis, and sometimes crepitation at the fracture site. The injured toe should be compared with the same toe on the other foot to detect rotational deformity, which can be done by comparing nail bed alignment. Nail bed injury and neurovascular status should also be assessed.
IMAGING
Radiographic evaluation is dependent on the toe affected; a complete foot series is not always necessary unless the patient has diffuse pain and tenderness. There should be at least three images of the affected toe, including anteroposterior, lateral, and oblique views, with visualization of the adjacent toes and of the joints above and below the suspected fracture location.
MANAGEMENT: GREAT TOE FRACTURES

Great toe fractures are generally treated with a short leg walking cast with a toe plate (Figure 1311 ) that extends past the great toe or with a short leg walking boot for two to three weeks.6 After this time, and in the absence of significant symptoms, the patient can progress to buddy taping and use of a rigid-sole shoe for three to four weeks.6,23,24 Range-of-motion exercises can generally be initiated at four weeks. Repeat radiography is indicated and should be obtained one week post-fracture if there was intra-articular involvement or if a reduction was required.

Healing time is typically four to six weeks. However, return to work and sport can generally take six to eight weeks depending on activity level; some high-level athletes may require more time.6
MANAGEMENT: LESSER TOE FRACTURES
Initial management of lesser toe fractures (Figure 14) includes buddy taping to an adjacent toe, use of a rigid-sole shoe, and ambulation as tolerated. Initial follow-up should occur within one to two weeks, then every two to four weeks for a total healing time of four to six weeks.6,23,24 Radiographic follow-up in seven to 10 days is necessary for fractures that required reduction or that involve more than 25% of the joint.6

ORTHOPEDIC REFERRAL
Indications for referral of toe fractures include a fracture-dislocation, displaced intra-articular fractures, nondisplaced intra-articular fractures involving more than 25% of the joint, and physis (growth plate) fractures. Patients with lesser toe fractures with angulation of more than 20° in the dorsoplantar plane, more than 10° in the mediolateral plane, or more than 20° rotational deformity should also be referred.6,23,24
Data Sources: We searched the Cochrane database, Essential Evidence Plus, and PubMed from 1900 to the present, human studies only, using the key words foot fractures, metatarsal, toe, and phalanges fractures. Search dates: February and June 2015.
