
A more recent article on slipped capital femoral epiphysis is available.
Am Fam Physician. 2017;95(12):779-784
Author disclosure: No relevant financial affiliations.
Slipped capital femoral epiphysis (SCFE) is the most common hip disorder in adolescents, occurring in 10.8 per 100,000 children. SCFE usually occurs in those eight to 15 years of age and is one of the most commonly missed diagnoses in children. SCFE is classified as stable or unstable based on the stability of the physis. It is associated with obesity, growth spurts, and (occasionally) endocrine abnormalities such as hypothyroidism, growth hormone supplementation, hypogonadism, and panhypopituitarism. Patients with SCFE usually present with limping and poorly localized pain in the hip, groin, thigh, or knee. Diagnosis is confirmed by bilateral hip radiography, which should include anteroposterior and frog-leg views in patients with stable SCFE, and anteroposterior and cross-table lateral views in unstable SCFE. The goals of treatment are to prevent slip progression and avoid complications such as avascular necrosis, chondrolysis, and femoroacetabular impingement. Stable SCFE is usually treated using in situ screw fixation. Treatment of unstable SCFE also usually involves in situ fixation, but there is controversy about timing of surgery and the value of reduction. Postoperative rehabilitation of patients with SCFE may follow a five-phase protocol.
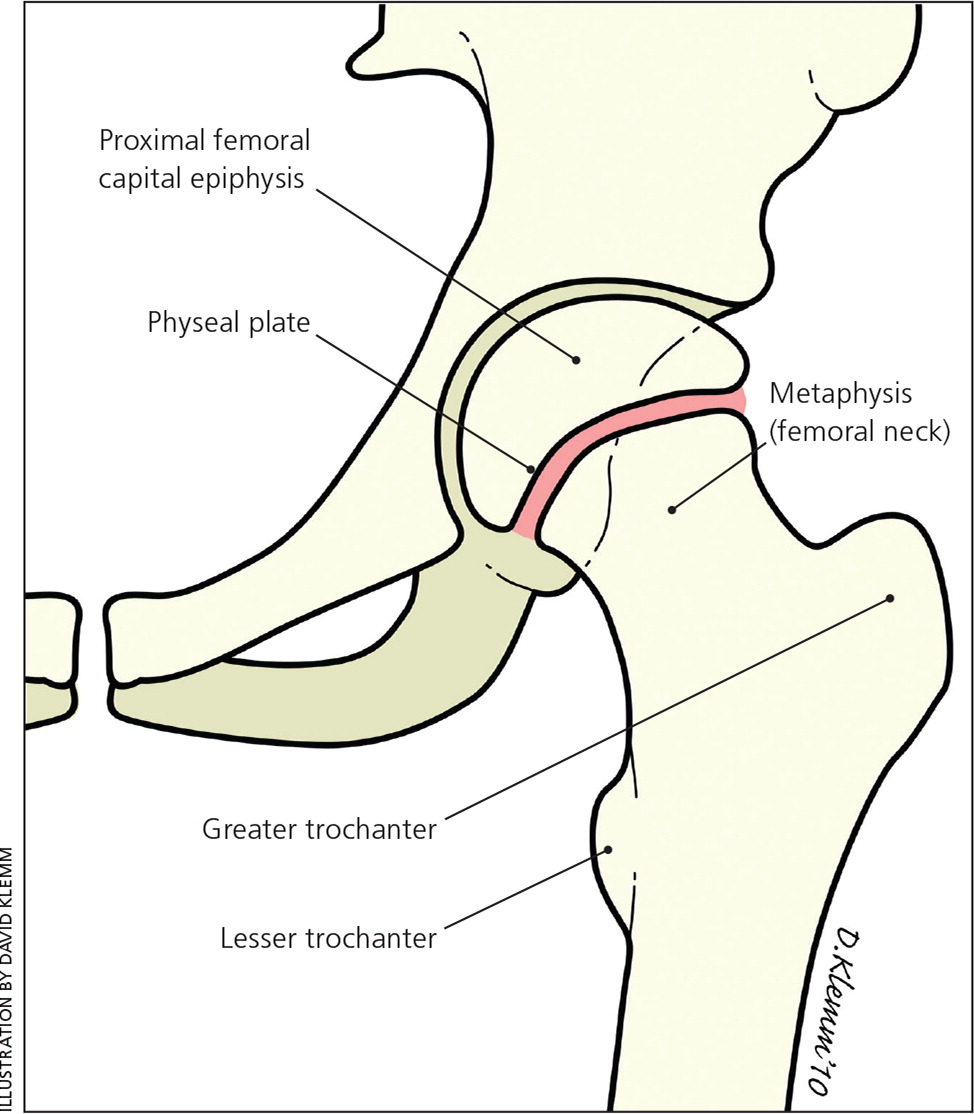
Slipped capital femoral epiphysis (SCFE) is the most common hip disorder in adolescents, usually occurring between eight and 15 years of age.1,2 SCFE is defined as the posterior and inferior slippage of the proximal femoral epiphysis on the metaphysis (femoral neck), which occurs through the epiphyseal plate (growth plate).1,2 Figure 1 illustrates developing hip anatomy.3 Because of various factors, physicians often miss SCFE when patients initially present with vague symptoms.4,5 In particular, physicians should be careful not to dismiss the patient's symptoms by diagnosing an adductor muscle strain (groin pull); this is rare in an adolescent. The prognosis is related to how quickly SCFE is diagnosed and treated.4,6 Delays in diagnosis can lead to disabling conditions and early-onset degenerative hip arthritis that eventually require hip reconstruction.7,8 SCFE should be considered in children who present with limping and vague pain in the hip, groin, thigh, or knee.1,4,7–9 These patients should be evaluated with appropriate radiography.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Family physicians should consider SCFE when a child presents with limping and groin, hip, thigh, or knee pain. | C | 1, 4, 7–9 |
| Physical examination findings in patients with SCFE include antalgic gait or nonambulatory decreased internal rotation of the hip and obligate external rotation. | C | 1, 5, 9 |
| Radiography should include anteroposterior and frog-leg lateral views for stable SCFE, and anteroposterior and cross-table lateral views for unstable SCFE. | C | 1, 10 |
| Single screw fixation is the standard treatment for stable SCFE. | C | 1, 5, 10, 32 |
| Rehabilitation for SCFE includes a five-phase protocol that focuses on protection, pain-free ambulation, neuromuscular control, strengthening, and performance enhancement. | C | 37 |
Classification
Classification of SCFE is based on the stability of the physis.10 If the patient is able to ambulate with or without crutches, the SCFE is considered stable.11 If the patient is unable to ambulate even with crutches, it is considered unstable.10 Stable SCFE accounts for about 90% of all slips.12 Classification is important because stable SCFE generally has a much better prognosis than unstable SCFE, which has a higher rate of complications.13 Another classification scale uses symptom duration; it defines acute symptoms as those that have been present for less than three weeks, chronic symptoms as those that have been present three weeks or longer, and acute-on-chronic symptoms as those that involve an acute exacerbation of chronic symptoms.14
Epidemiology
The prevalence of SCFE is 10.8 cases per 100,000 childern.2,13 It is typically more common in boys than girls. However, the prevalence is changing because of increasing body weight, which may also account for increased incidence in blacks and Pacific Islanders.13 The average age at diagnosis is 13.5 years for boys and 12 years for girls.13 SCFE presents bilaterally in 18% to 50% of patients.15–17 Some slips present sequentially, often occurring within 18 months of each other.11 There is a seasonal variation in the rate of SCFE in the northern United States, with increased rates in late summer and fall in patients who live north of 40 degrees latitude.18,19 This may be caused by increased physical activity in the summer or from impaired vitamin D synthesis.
Etiology
The etiology of SCFE is thought to be multifactorial and may include obesity, growth spurts, and, less commonly, endocrine disorders.20–23 Among children diagnosed with SCFE, 63% have a weight in the 90th percentile or higher.24,25 Related endocrine abnormalities include hypothyroidism, growth hormone supplementation, hypogonadism, and panhypopituitarism.2 An endocrine disorder should be considered in patients with SCFE who have unusual presentations, including those who are younger than eight years or older than 15 years, who are underweight, or who have short stature.4,22
History and Physical Examination
The differential diagnosis of hip pain in young patients is broad (Table 1).3 The most common symptoms of SCFE are limping and pain that is poorly localized to the hip, groin, thigh, or knee.9 Knee or distal thigh pain is the presenting symptom in 15% of patients with this condition.26 History of trauma to the area is rare.10,27 Approximately 88% of patients with unstable SCFE had antecedent symptoms before presentation.15 Because delayed diagnosis of SCFE may result in a poorer prognosis, it is imperative that physicians strongly consider SCFE when a child presents with vague hip or knee pain.
| Condition* | Age (years) | Clinical features | Incidence | Diagnosis |
|---|---|---|---|---|
| Apophyseal avulsion fracture of the anterosuperior and anteroinferior iliac spine | 12 to 25 | Pain after sudden forceful movement | Common | History of trauma; radiography |
| Apophysitis of the anterosuperior and anteroinferior iliac spine | 12 to 25 | Activity-related hip pain | Common | History of overuse; radiography to rule out fractures |
| Transient synovitis | < 10 | Limping or hip pain | Common | Radiography, laboratory testing, ultrasonography |
| Fracture | All ages | Pain after traumatic event | Less common | History of trauma; radiography |
| Slipped capital femoral epiphysis | 8 to 15 | Hip, groin, thigh, or knee pain; limping | Less common | Bilateral hip radiography |
| Legg-Calvé-Perthes disease | 4 to 9 | Vague hip pain, decreased internal rotation of hip | Uncommon | Hip radiography or magnetic resonance imaging |
| Septic arthritis | All ages | Fever, limping, hip pain | Uncommon | Radiography; laboratory testing; joint aspiration |
| Adductor muscle strain (groin pull) | 12 to 20 | Groin pain after activity | Very uncommon | Radiography to rule out fracture; physical examination |
On physical examination, the patient may have an antalgic gait or may be unable to bear weight with a severe slip. Limited internal rotation of the hip is the most telling sign.9 Obligatory external rotation (Drehmann sign) is noted in the involved hip of patients with SCFE when the hip is passively flexed to 90 degrees1,5,9 (Figure 23 ). Unless the patient has bilateral SCFE, it is helpful to compare range of motion with the uninvolved hip.

Radiography
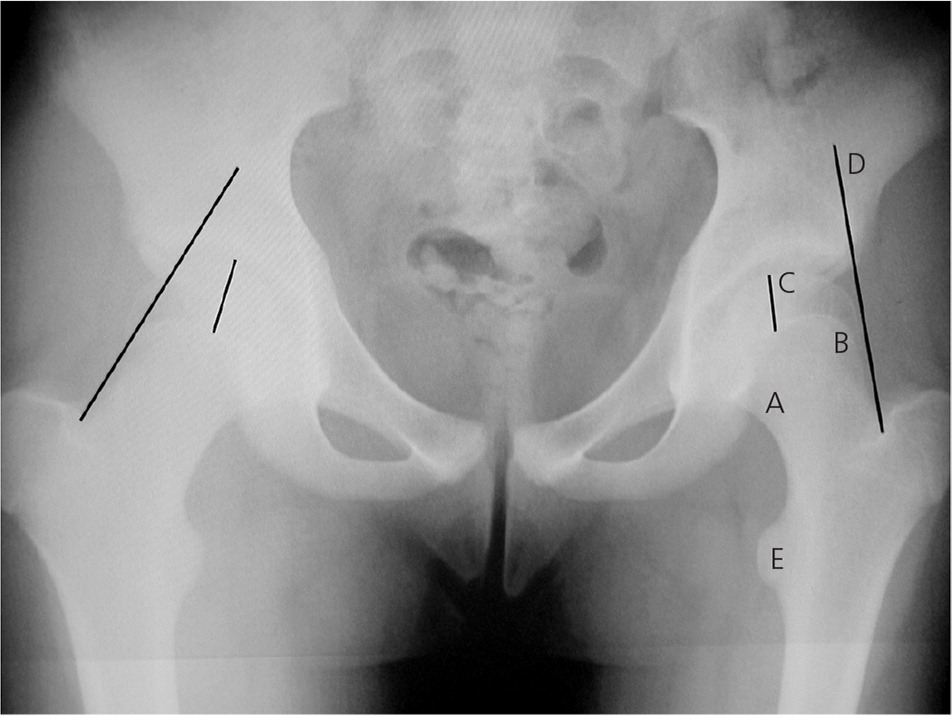
Radiography is required to evaluate for SCFE in patients eight to 15 years of age who have new-onset limping and pain in the hip, groin, thigh, or knee. It is important to inform the radiologist that SCFE is suspected because radiography should include anteroposterior and frog-leg lateral views of both hips to diagnose stable SCFE (Figure 33 ), whereas in unstable SCFE, anteroposterior and cross-table lateral views of the involved side should be obtained. These radiographs should be compared with the uninvolved side to evaluate the decreased range of motion of the affected side.1,10 The radiologic signs of SCFE are shown in Figures 4 and 5.3
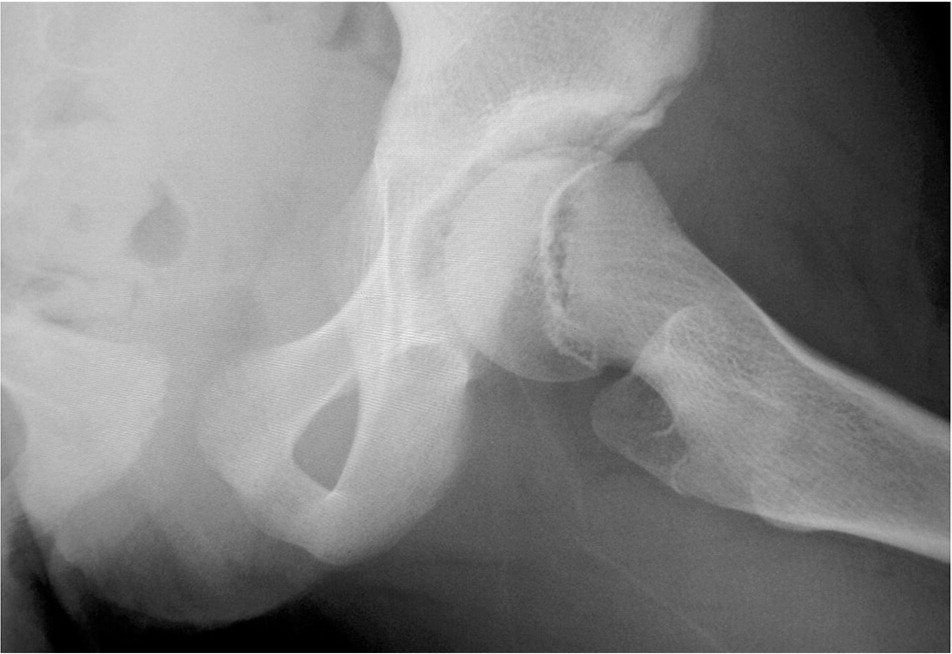
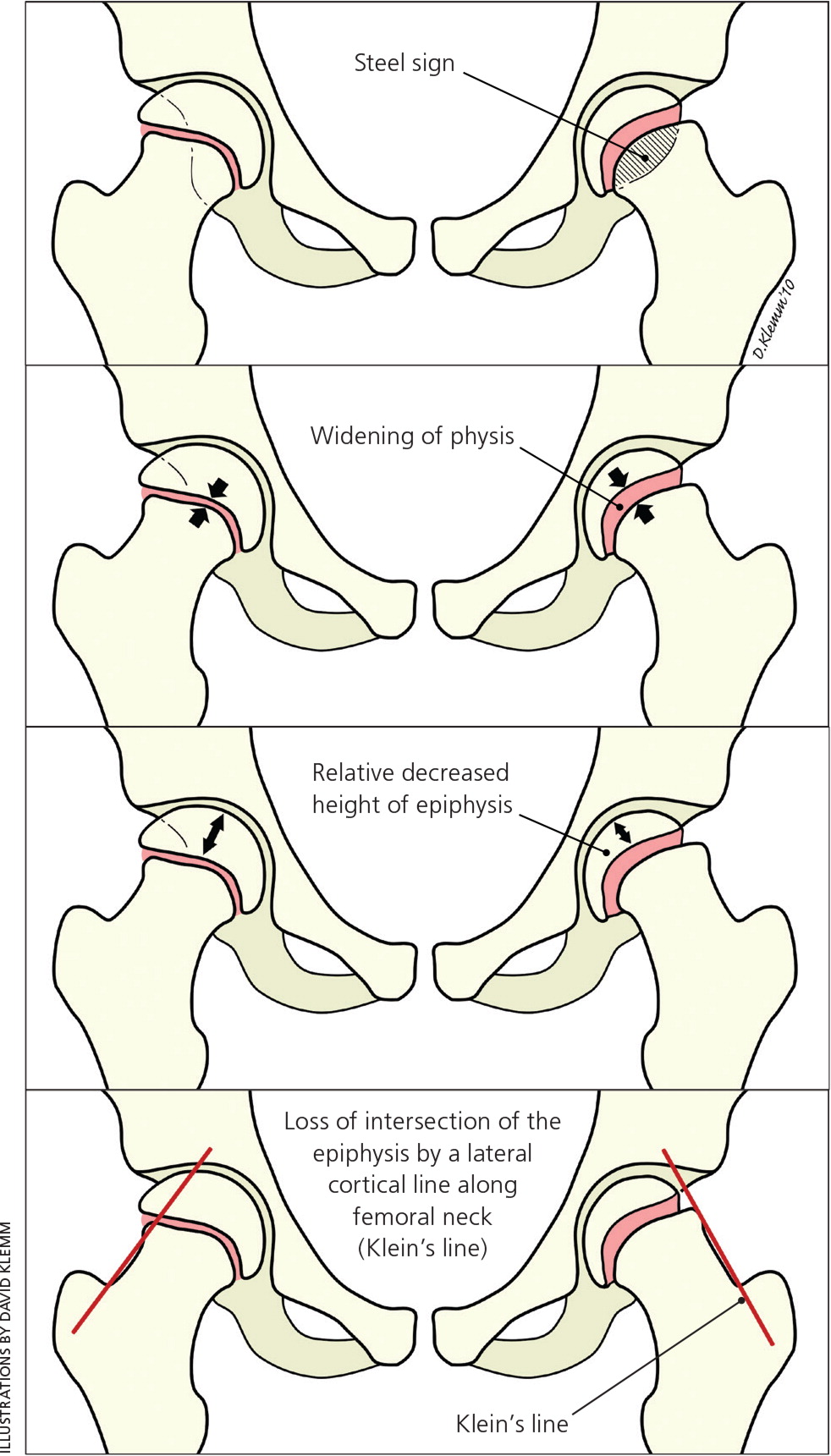
Radiography is used to grade the severity of the slip in SCFE. The Wilson method measures the relative displacement of the epiphysis on the metaphysis in a frog-leg lateral radiograph. A mild slip involves epiphysis displacement of less than one-third of the width of the metaphysis; a moderate slip involves displacement of one-third to one-half of the width; and a severe slip involves displacement of greater than one-half of the width.10
Treatment
Once the diagnosis of SCFE is made, the patient should be placed on non–weight-bearing crutches or in a wheelchair and urgently referred to an orthopedic surgeon familiar with the treatment of SCFE.1 The initial goals of treatment are to prevent slip progression and avoid complications.10,28 A forceful relocation of the injury should not be attempted; such maneuvers can result in avascular necrosis caused by restricted blood supply to the femoral head.29
Prophylactic treatment of the contralateral hip is controversial, but it is not recommended in most patients.30,31 Prophylactic pinning may be indicated in patients at high risk of subsequent slips, such as younger patients and those with obesity or an endocrine disorder, or those who have a low likelihood of follow-up.12,17,30
STABLE SCFE
The standard treatment of stable SCFE is in situ fixation with a single screw.1,5,10,32 Case series and animal studies have shown this to be a simple technique with low rates of recurrence and complications.5,10,32 After closure of the growth plate, progression of athletic activities may be allowed, including running and eventual participation in contact sports.1 Most patients with mild to moderate stable SCFE who are treated with in situ fixation have good to excellent long-term outcomes.12
UNSTABLE SCFE
Unstable SCFE is a much more severe injury than stable SCFE. The rate of osteonecrosis is as high as 20% to 50% in patients with the unstable type.10,33 Treatment goals are similar to those of stable SCFE with in situ fixation, but there is controversy as to the specifics of treatment, including timing of surgery, value of reduction, and manner of reduction.1,32 The currently recommended approach is the modified Dunn procedure, which is a surgical hip dislocation that helps restore the alignment of the proximal femur to decrease the rate of femoroace-tabular impingement.29 Femoroacetabular impingement is considered a complication of treated unstable SCFE, and research is underway to minimize this complication, such as with open treatment.
Complications
AVASCULAR NECROSIS
Avascular necrosis (i.e., osteonecrosis of the femoral epiphysis) occurs in up to 50% of patients with unstable SCFE.32 It results from kinking of the blood vessels or hematoma formation, which disrupts the tenuous blood supply to the femoral head and is associated with severe displacement and/or fixation with more than one screw.9,28 Avascular necrosis often leads to advanced and early degenerative osteoarthritis.34
CHONDROLYSIS
Chondrolysis is the acute loss of articular cartilage, which causes joint stiffness and pain.10 It is usually reported as a complication of surgical treatment of SCFE, but can occur with the use of a hip spica cast and in untreated advanced SCFE. The most common cause is unrecognized pin penetration of the femoral head. As surgical techniques have improved, the incidence of chondrolysis has decreased from 7% to 1% in patients treated for SCFE.9,28
FEMOROACETABULAR IMPINGEMENT
Femoroacetabular impingement derives from the abnormal shape of the proximal femur or the prominence of the acetabular rim that may lead to early onset of hip osteoarthritis. Recent studies have shown clinical and radiologic evidence of femoroacetabular impingement in the first 10 years after SCFE treatment.29,35 It occurs when a severe slip heals in poor position. It may be prevented by a subtrochanteric osteotomy.36 Recent research has shown that some of the newer open surgical techniques may decrease the incidence of femoroacetabular impingement, thus decreasing the effects of early-onset osteoarthritis.29,35
Rehabilitation
Postoperative rehabilitation protocols for SCFE are poorly described in the literature. Most physiatrists recommend a five-phase protocol with predictable recovery times.37 Phase 1 focuses on reducing joint inflammation, protecting soft-tissue repair, synergistic muscle activation, and range of motion. Appropriate ambulatory aids are used, and gait analysis is performed to observe the patient's heel-to-toe pattern. Phase 2 includes discarding crutches if the patient has a normal pain-free gait and can perform straight leg raise abduction without pain. Phases 3 and 4 involve strengthening within functional movement patterns, increasing range of motion, and aerobic conditioning. Phase 5 involves ensuring adequate functional power for return to play or daily functioning. The time frame for return to play is variable and set by the orthopedic surgeon.
This article updates previous articles on this topic by Loder1 and Peck.3
Data Sources: A PubMed search was completed in Clinical Queries using the key term slipped capital femoral epiphysis. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports and the Cochrane database. Search date: October 9, 2015.