Am Fam Physician. 2020;102(12):740-750
Patient information: See related handout on degenerative cervical myelopathy
Author disclosure: No relevant financial affiliations.
Degenerative cervical myelopathy encompasses a collection of pathologic conditions that result in progressive spinal cord dysfunction secondary to cord compression. Patients are typically male (3:1 male-to-female ratio), and the average age of presentation is 64 years. The exact incidence is unclear because of differences in terminology and because radiographic findings can be present in asymptomatic individuals. Common examination findings include neck pain or stiffness, a wide-based ataxic gait, ascending paresthesia in the upper or lower extremities, lower extremity weakness, decreased hand dexterity, hyperreflexia, clonus, Babinski sign, and bowel or bladder dysfunction in severe disease. Definitive diagnosis requires correlation of physical examination findings with imaging findings. Magnetic resonance imaging of the cervical spine with and without contrast media is the preferred imaging modality. Cervical spine computed tomography, computed tomography myelography, and plain radiography are helpful in certain situations. Treatment depends on the presence and severity of symptoms. Surgery is recommended for patients with moderate to severe symptoms or rapidly progressive disease. Conservative treatments with monitoring for progression may be considered in patients with mild to moderate disease. The evidence for the effectiveness of conservative treatments is scarce and of low quality, and outcomes can vary with individual patients. Primary care physicians play a vital role in recognizing the typical presentation of degenerative cervical myelopathy, coordinating treatment as indicated, and managing comorbidities.
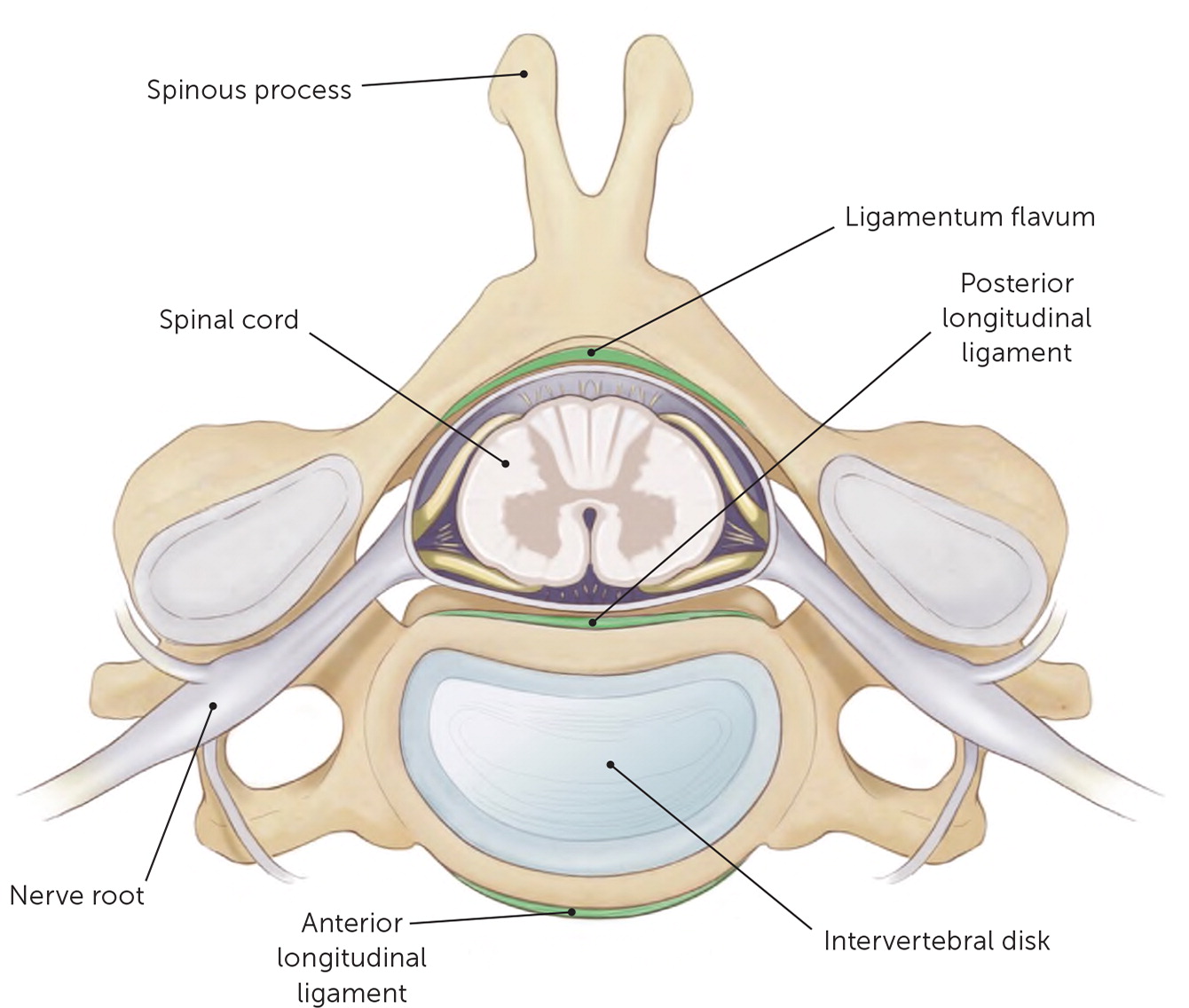
Degenerative deterioration of the vertebrae, intervertebral disks, the facet, and other joints of the spine can result in cervical spondylotic myelopathy.1,2 Hypertrophy and ossification of the posterior longitudinal ligament and the ligamentum flavum can lead to spinal cord compression, injury, and subsequent myelopathy.3
| Acute transverse myelitis | Liver disease |
| Alcohol abuse | Multiple sclerosis |
| Amyotrophic lateral sclerosis | Paraneoplastic syndrome |
| Copper or vitamin B12 deficiency | Parkinson disease |
| Cubital or carpal tunnel syndrome | Syphilis |
| Guillain-Barré syndrome | Syringomyelia |
| HIV or human T-lymphotropic virus 1 infection | Viral encephalitis |
A combination of static and dynamic factors plays a role in the development of symptomatic degenerative cervical myelopathy.5–7 Patients with the condition typically present in their late 50s to early 60s with signs and symptoms ranging from vague cervical spine pain to frank myelopathy from significant spinal cord compression. Patients with degenerative cervical myelopathy usually deteriorate over time; however, the rate of deterioration is unpredictable and highly variable.8,9
Patients with degenerative cervical myelopathy often first present to their primary care physicians with a wide range of symptoms. Although conservative treatment is an acceptable initial approach for patients with mild to moderate symptoms, 20% to 60% of these patients deteriorate over three to six years and may eventually require surgical intervention.7,10,11 Studies have shown that a delay in diagnosis and referral by primary care physicians can lead to poorer outcomes.12 Therefore, it is important to promptly recognize, evaluate, and appropriately refer patients with signs and symptoms of degenerative cervical myelopathy. Primary care physicians play a vital role not only in diagnosis but in treatment coordination and comorbidity management.
Incidence and Prevalence
Degenerative cervical myelopathy is the most common degenerative, nontraumatic, and progressive form of spinal cord compression worldwide.3,10,13,14 It is also recognized as the leading cause of spinal cord impairment and indication for cervical spine surgery worldwide.15,16 Because of differences in terminology, it is difficult to determine the exact incidence and prevalence of degenerative cervical myelopathy. In North America, the published annual incidence is 41 per 1 million and prevalence is 605 per 1 million.3,14 In the United States alone, 15,000 to 20,000 people are hospitalized every year for treatment of degenerative cervical myelopathy at a cost of several hundred million dollars.17 The average age at presentation is 64 years, it is more common in men (3:1 male-to-female ratio), and C5–C6 is the most common level of cord compression followed by C6–C7 and C4–C5.1,18,19
The high prevalence of asymptomatic individuals with radiographic evidence of cervical degeneration presents a challenge in determining the burden of this condition and supports the importance of a thorough clinical history and physical examination to avoid overdiagnosis. Multiple studies have shown that in patients older than 40 years, 50% to 60% have evidence of disk degeneration, 20% have foraminal stenosis, and upwards of 10% have clinically significant root or cord compression.1,8,9,19 These numbers increase with age, and 95% of men and 70% of women older than 70 years have evidence of cervical spondylosis.15,18
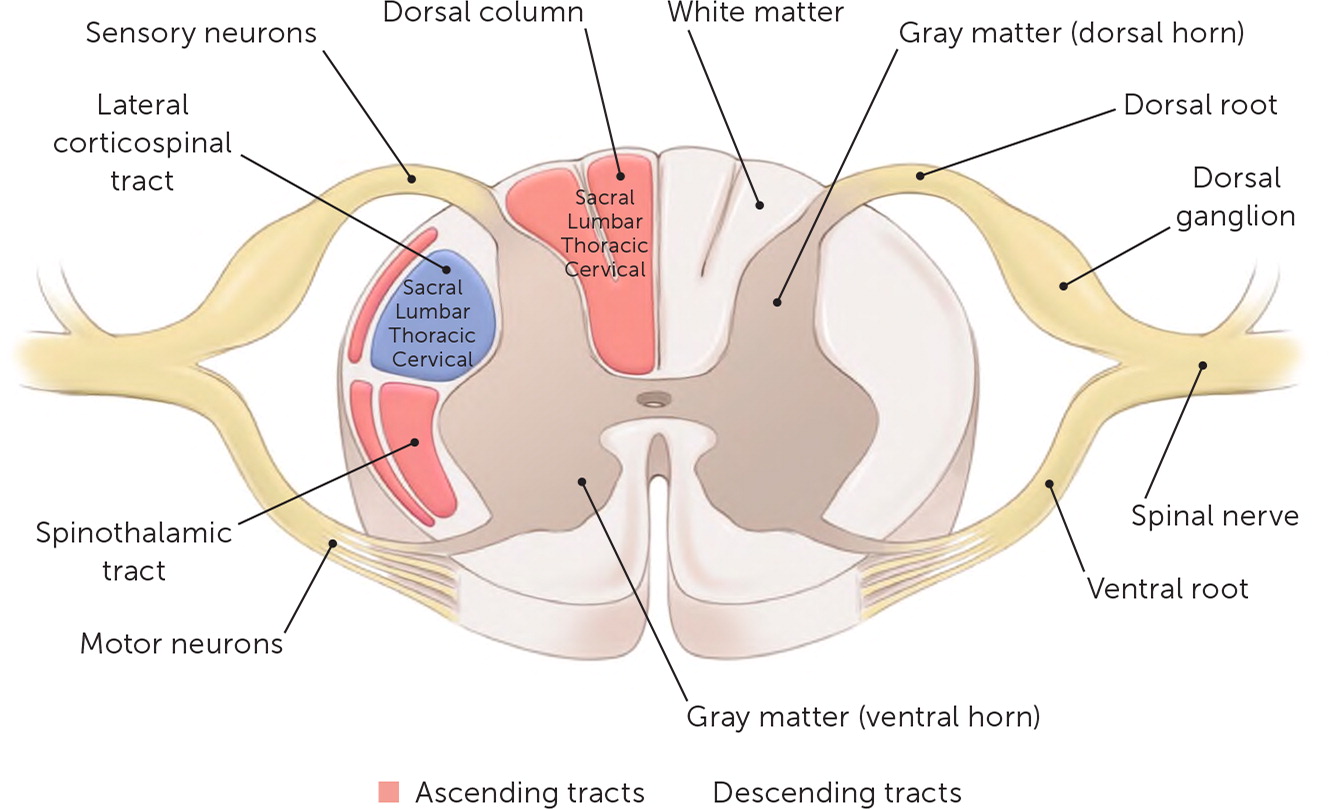
Anatomy
There are seven cervical vertebrae and eight cervical spinal nerves. The spinal nerves are composed of motor fibers from the ventral horn and sensory fibers from the dorsal horn. The ventral and dorsal horns make up the central gray matter of the spinal cord. The ascending and descending white matter tracts surround the central gray matter. There are multiple white matter tracts in the spinal cord. This article focuses on three major tracts (Table 2).20 The dorsal column and the spinothalamic tract are the ascending tracts and transmit sensory (ipsilateral pressure and vibration, and contralateral pain and temperature sensation) information to the brain. The lateral corticospinal tract is the largest, most significant descending tract and transmits information from the motor cortex to the periphery.21
| Spinal cord tracts | Location |
| Dorsal column | Located between the dorsal horns; carries ipsilateral pressure and vibration sensation |
| Lateral corticospinal tract | Lateral aspect of the spinal cord; controls ipsilateral motor function |
| Spinothalamic tract | Located in the anterior cord; carries contralateral pain and temperature sensations |
| Spinal cord pathology* | Physical examination findings |
| Dorsal column syndrome | Vibratory and proprioceptive loss below a dermatomal level with preservation of other sensory modalities |
| Hemicord (Brown-Séquard) syndrome | Ipsilateral weakness, vibratory and proprioceptive loss, contralateral pain, and temperature loss |
| Posterior lateral syndrome | Decreased vibratory and proprioceptive sensation and motor control impairments |
The nerve fibers corresponding to the lower extremities are the most peripherally located, and the upper extremity fibers are more central. Most of the pathologic processes that result in degenerative cervical myelopathy compress the cord, which is why symptoms predominantly occur in the lower extremities.20,22 Knowledge of the location of peripheral dermatomes in terms of sensory, motor, and reflex functions is also important when diagnosing the level of spinal cord involvement. Figure 1 and Figure 2 illustrate the anatomy of the spinal cord.
Etiology
Mechanical compression of the spinal cord is the underlying cause of degenerative cervical myelopathy. However, the exact pathobiological mechanism that leads to spinal cord dysfunction is not clearly understood. A combination of an inflammatory response, vascular changes, ischemia, and venous congestion likely plays a role in cellular apoptosis, axon degeneration, and changes in the myelin that result in the signs and symptoms of degenerative cervical myelopathy.22,23 Degenerative changes occur as a normal part of aging.1,6,22,24
| Static |
| Congenital stenosis |
| Degenerative disk disease |
| Ossification of the ligamentum flavum |
| Ossification of the posterior longitudinal ligament |
| Spondylosis |
| Vertebral body osteophytes |
| Dynamic |
| Degenerative spondylolisthesis |
| Physiologic narrowing of the canal |
| Strain and stretch placed on the spinal cord during movements |
Static factors include acquired or congenital conditions that narrow the spinal canal, increasing the risk of cord compression. Degeneration and deterioration of the intervertebral disk can lead to collapse and subsequent posterior bulging. Vertebral body osteophytes, ossification of the posterior longitudinal ligament, and hypertrophy and ossification of the ligamentum flavum can also lead to cord compression and compromise1,22,25 (Figure 3).
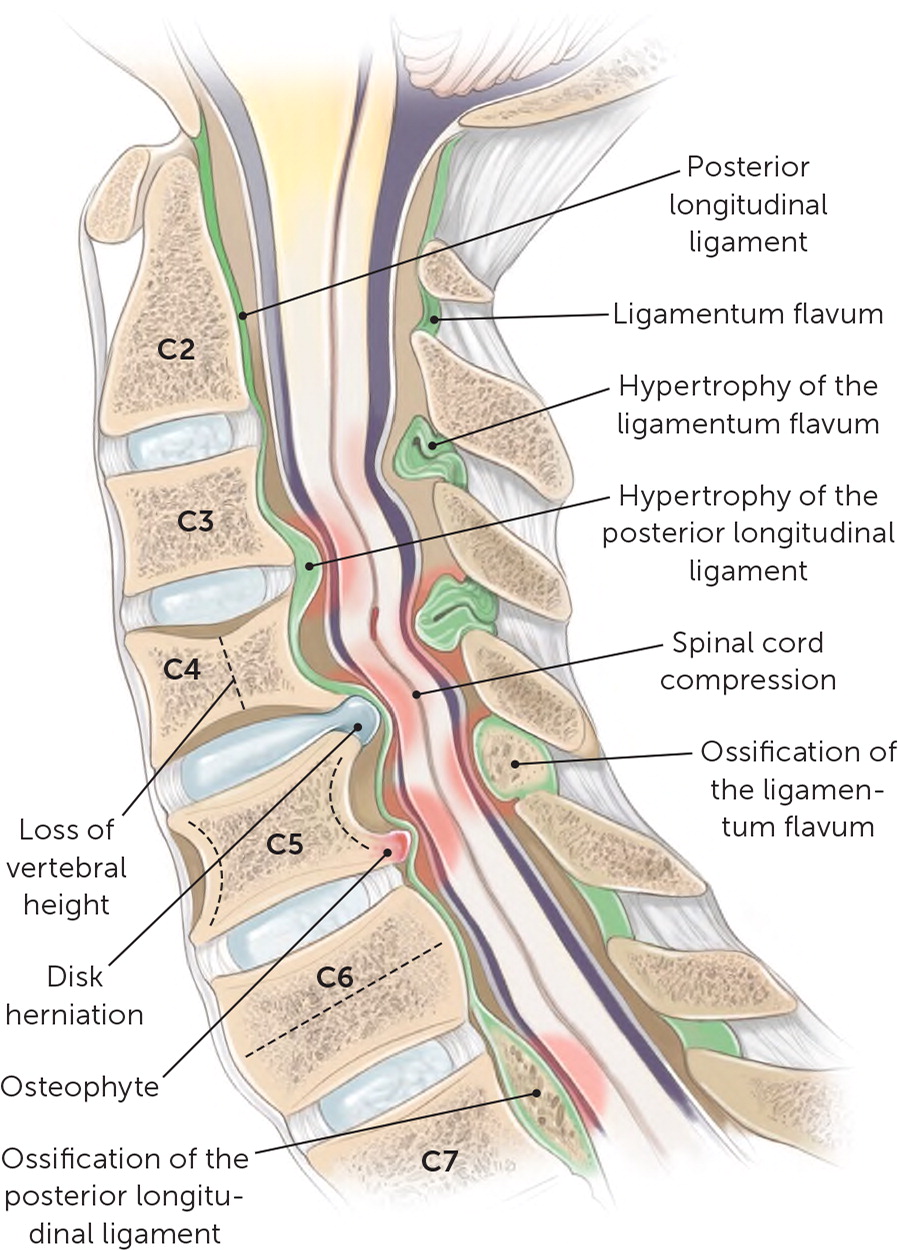
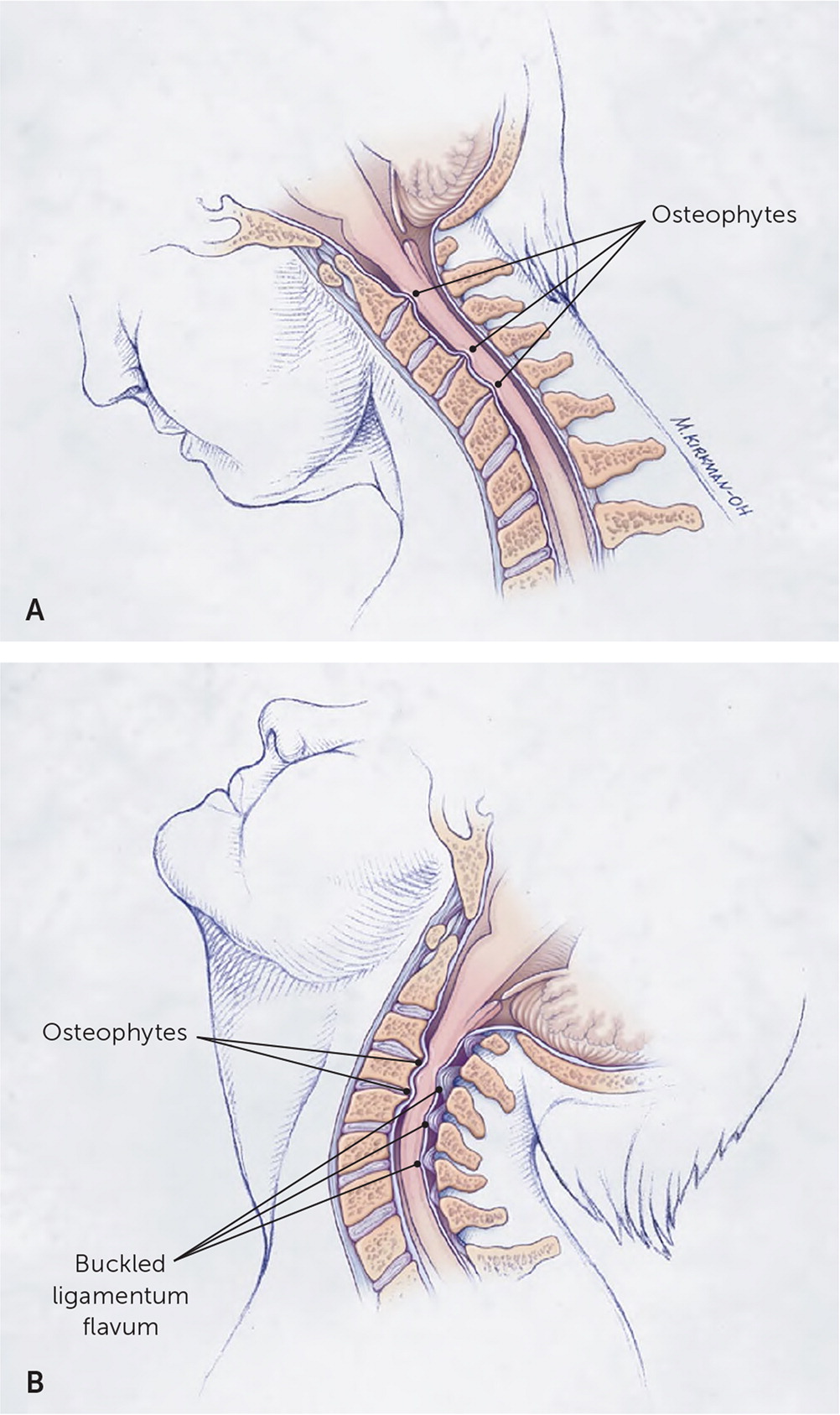
Dynamic factors include changes in the biomechanics of the cervical spine causing irritation, compression, tethering, and shearing of the spinal cord, which leads to degenerative cervical myelopathy. Flexion and extension are the primary motions that exacerbate underlying static pathology (Figure 426). During flexion and extension, the cord is compressed by the various pathologic changes.1,6,22
Degenerative cervical myelopathy typically involves multiple levels of the spinal cord as a result of segments adjacent to the pathology becoming hyper- or hypomobile, leading to more cord damage.6
Diagnosis
PHYSICAL EXAMINATION
The signs and symptoms of cervical myelopathy are variable and can mimic other conditions, especially in early disease, making the diagnosis challenging. Common symptoms include neck pain or stiffness, shoulder pain with potential radiation to the upper extremities, feeling unsteady, difficulty with fine motor tasks, decreased hand dexterity (e.g., change in handwriting, clumsiness), ascending paresthesia in the upper or lower extremities, lower extremity weakness, and bowel or bladder dysfunction. The symptoms of degenerative cervical myelopathy are persistent and not fluctuating or transient.2
Upper motor neuron signs/symptoms (Table 44,9,13,18,27,28) are the hallmark of cervical myelopathy, whereas lower motor neuron symptoms are manifestations of peripheral nerve pathology as seen in radiculopathies. Patients most often experience lower motor neuron symptoms at the level of the pathology and upper motor neuron symptoms below this level.21,29
| Signs |
| Atrophy of intrinsic hand muscles |
| Babinski sign |
| Clonus: Achilles tendon is more commonly affected than the patella |
| Gait disturbance: wide-based ataxic gait |
| Hyperreflexia of the deep tendon reflexes |
| Hyporeflexia of superficial reflexes (abdominal and cremasteric) |
| Lhermitte sign (27%) |
| Pathologic (upper motor neuron) reflexes: Hoffmann sign inverted brachioradialis reflex, Romberg sign, and Brissaud reflex |
| Pyramidal weakness: upper extremity extensors > upper and lower extremity flexors > lower extremity extensors |
| Spasticity |
| Synkinesis: involuntary movement in a limb associated with voluntary movement of other limbs |
| Symptoms |
| Ascending paresthesia in the upper and lower extremities |
| Autonomic: erectile dysfunction, difficulty with elimination (44%), or bowel or bladder incontinence |
| Decreased hand dexterity, changes in handwriting |
| Falls |
| Lower extremity stiffness, weakness, and sensory loss |
| Neck pain (50%) and stiffness |
| Radicular pain (38%) |
| Scapular pain |
The most common physical examination findings include decreased and possibly painful range of motion in the cervical spine, Lhermitte sign, hyperreflexia, clonus, upper motor neuron reflexes, a wide-based ataxic gait, spasticity, atrophy of intrinsic hand muscles, and upper extremity segmental weakness.20 These physical examination findings localize the pathology to the spinothalamic and corticospinal tracts, which are affected first because of their lateral location in the spinal cord.20,21
The physical examination findings associated with degenerative cervical myelopathy tend to be more specific than sensitive (Table 5).26,30–33 The presence of sustained clonus or the Babinski sign was found to have 13% sensitivity and 100% specificity for upper motor neuron–associated myelopathy.30 Presence of the Hoffmann sign (sensitivity = 59% to 67%; specificity = 81%) and inverted brachioradialis reflex, also called inverted supinator sign, (sensitivity = 51%; specificity = 81%) have demonstrated higher sensitivity while maintaining good specificity for the condition.30 Evaluation for the Hoffmann sign is shown in Figure 5, and a video is available at https://www.youtube.com/watch?v=blj6Y0rrmtw. The inverted brachioradialis reflex test is shown in Figure 6, and a video is available at https://www.youtube.com/watch?v=S8q4WuQABjc. The loss of the C5 (biceps) and C6 (brachioradialis) reflexes in the presence of a brisk C7 (triceps) reflex is almost a pathognomonic physical examination finding for spinal cord compression at C5–C6.26
| Sign | Positive finding | Sensitivity | Specificity |
|---|---|---|---|
| Sustained clonus | Rhythmic flexion and extension of the ankle, at least three beats, after a sudden and sustained dorsiflexion at the ankle | 13% | 100% |
| Babinski sign | Extension of the great toe with abduction of the remaining toes when a noxious stimulus is applied from the base of the lateral aspect of the calcaneus upward to the base of the toes | 13% | 100% |
| Hoffmann sign | Opposition of the thumb and slight flexion of the fingers after flicking the middle finger (Figure 5, https://www.youtube.com/watch?v=blj6Y0rrmtw) | 59% to 67% | 81% |
| Inverted brachioradialis reflex, also called inverted supinator sign | Tapping of the styloid process of the radius results in absence of brachioradialis muscle contraction and flexion of the wrist and digits (Figure 6, https://www.youtube.com/watch?v=S8q4WuQABjc) | 51% | 81% |
| Brissaud reflex | Stroking the sole of the foot results in a vigorous contraction of the ipsilateral tensor fasciae lata | Not reported | |
| Lhermitte sign | Flexion of the neck results in a shooting, electrical sensation down the spine | Not reported |


Central nervous system conditions, such as degenerative cervical myelopathy, and a concomitant peripheral lesion, such as radiculopathy, both can present as sensory and motor abnormalities. Deep tendon hyperreflexia is a key finding with myelopathies because radiculopathies cause hyporeflexia of the deep tendons.13 Physical examination findings help narrow the broad differential diagnosis, but a definitive diagnosis requires correlation of the physical findings with imaging findings.
IMAGING
According to American College of Radiology Appropriateness Criteria, magnetic resonance imaging (MRI) with and without contrast media is the imaging modality of choice for patients with suspected degenerative cervical myelopathy34 (Figure 7 and Figure 8). However, MRI can be costly, unavailable, or contraindicated.
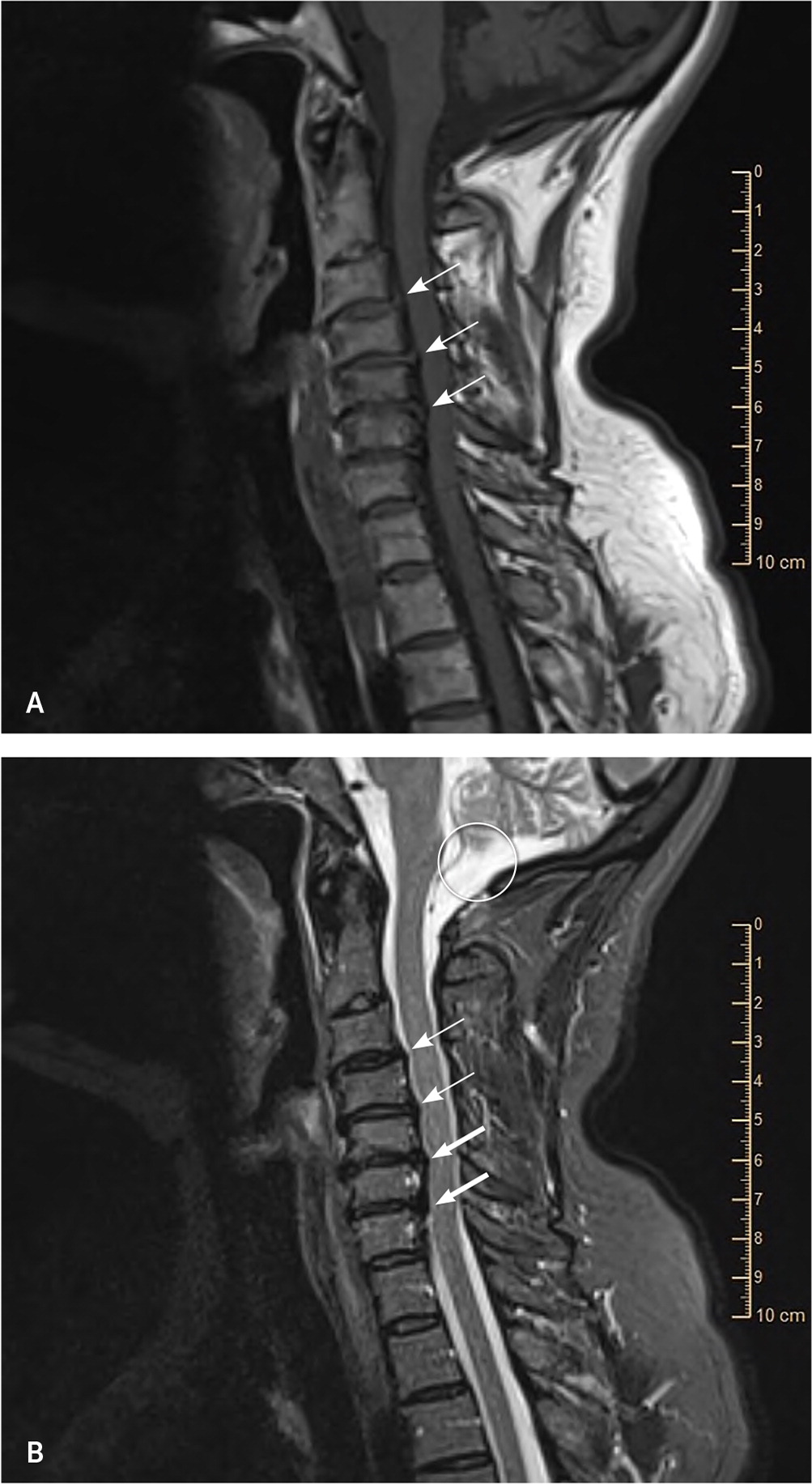
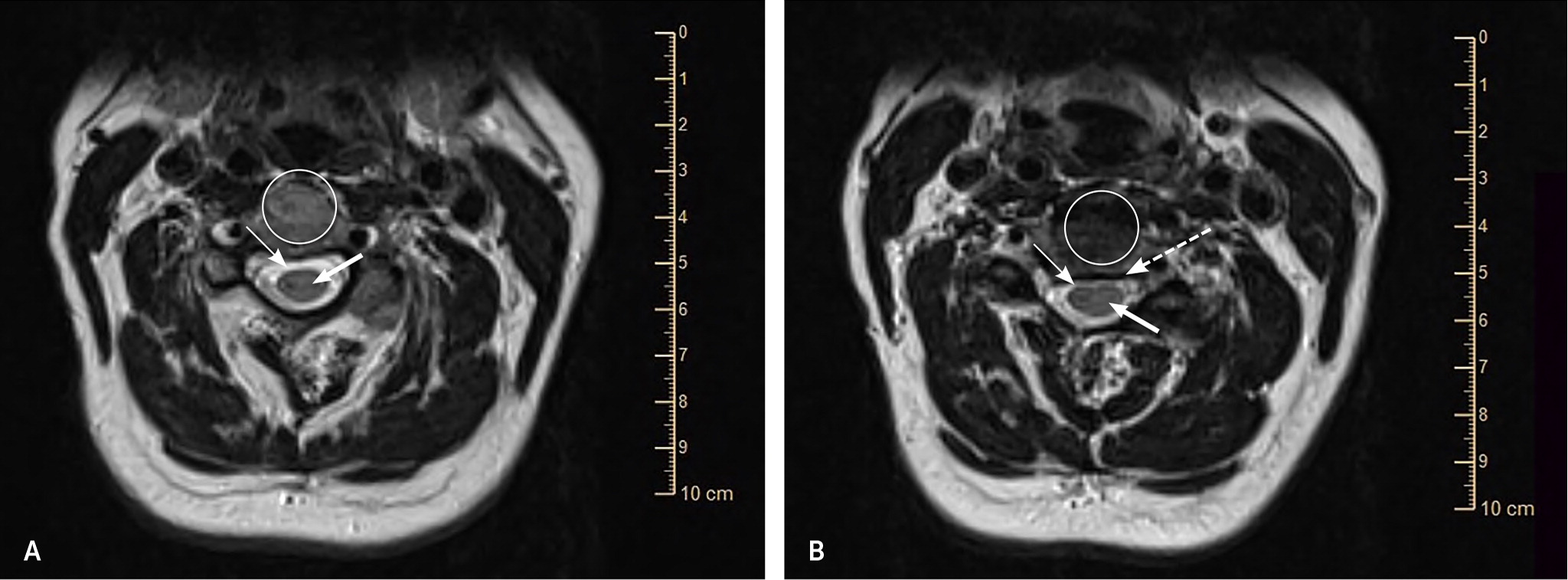
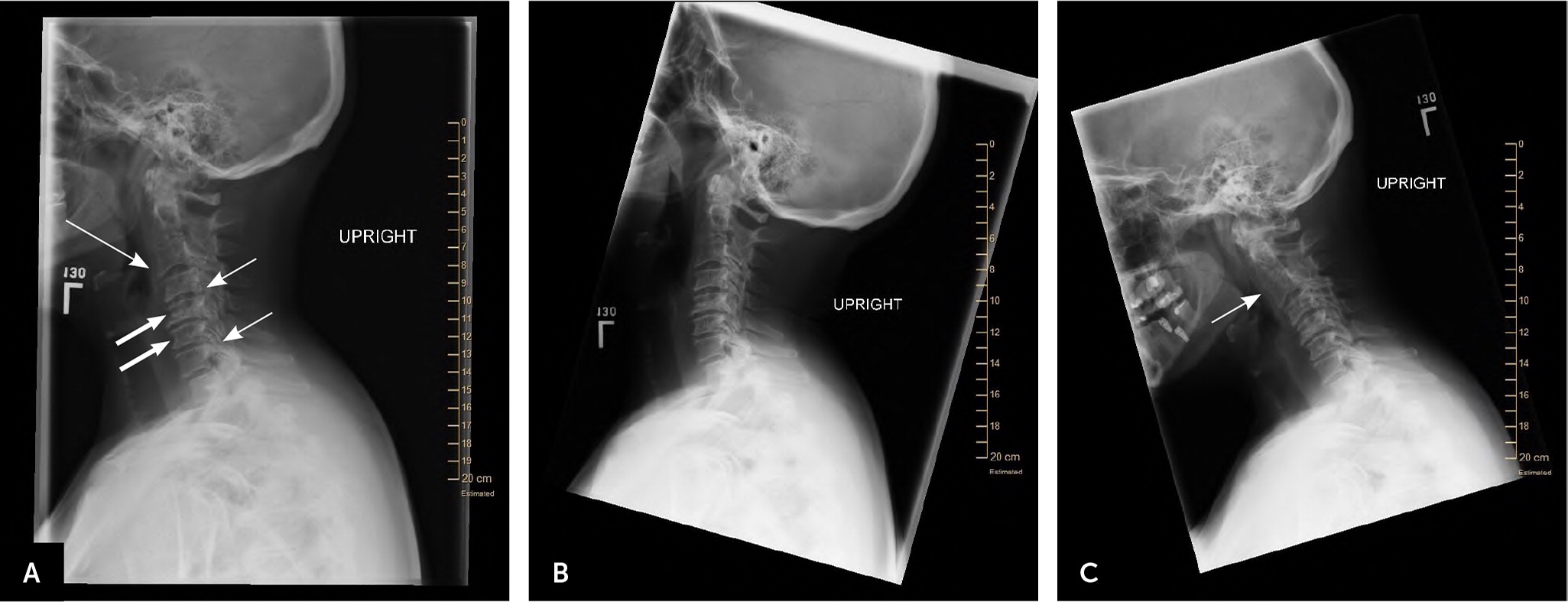
Despite not showing soft tissue details, plain radiography can be helpful in assessing spinal canal narrowing, cervical lordosis or kyphosis, and cervical stability35 (Figure 9). The best evidence for the use of computed tomography is in patients with chronic, progressive cervical pain and plain radiography showing ossification of the posterior longitudinal ligament. Computed tomography myelography can reproduce measurements of cervical intracanal dimensions, making it a valuable alternative if MRI is contraindicated. However, because of limitations in visualizing soft tissue changes prevalent in disk pathology and other pertinent findings and the need to inject contrast media into the spinal column, it is not the preferred imaging modality for degenerative myelopathy.10,24
FUNCTIONAL SCALES
| Level of dysfunction | Points |
|---|---|
| Motor dysfunction | |
| Upper extremities | |
| Unable to move hands | 0 |
| Unable to eat with a spoon but able to move hands | 1 |
| Unable to button shirt but able to eat with a spoon | 2 |
| Able to button shirt with great difficulty | 3 |
| Able to button shirt with slight difficulty | 4 |
| Lower extremities | |
| Complete loss of motor and sensory function | 0 |
| Sensory preservation without ability to move legs | 1 |
| Able to move legs but unable to walk | 2 |
| Able to walk on a flat floor with a walking aid (cane or crutch) | 3 |
| Able to walk up and/or down stairs with aid of a handrail | 4 |
| Moderate to significant lack of stability but able to walk up and/or down stairs without a handrail | 5 |
| Mild lack of stability but able to walk unaided with smooth reciprocation | 6 |
| No dysfunction | 7 |
| Sensory dysfunction | |
| Upper extremities | |
| Complete loss of hand sensation | 0 |
| Severe sensory loss or pain | 1 |
| Mild sensory loss | 2 |
| No sensory loss | 3 |
| Sphincter dysfunction | |
| Unable to urinate voluntarily | 0 |
| Marked difficulty with urination | 1 |
| Mild to moderate difficulty with urination | 2 |
| Normal urination | 3 |
| Total: | _______ |
| Sign/symptom | Points |
|---|---|
| Signs and symptoms of root involvement but without evidence of spinal cord disease | 0 |
| Signs of spinal cord disease but no difficulty walking | 1 |
| Slight difficulty in walking that does not prevent full-time employment | 2 |
| Difficulty in walking that prevents full-time employment or the ability to do all housework, but that is not so severe that someone else's help is required to walk | 3 |
| Able to walk only with someone else's help or with the aid of a walker or other assistance device | 4 |
| Chairbound or bedridden | 5 |
| Total: | ______ |
Treatment
The treatment of severe, progressive degenerative cervical myelopathy is primarily surgical, and patients should be referred to a surgeon when the diagnosis is initially suspected.35 However, the treatment approach for asymptomatic, mild to moderate disease is not as evident because of the unclear natural history of the disease and conflicting treatment outcomes.36 Although some low-quality studies demonstrated better short-term outcomes for pain relief, weakness, and sensory loss with surgery vs. physical therapy and immobilization, there were no significant differences between the groups at one and three years.5,36,37 Therefore, it is appropriate to initially consider nonsurgical treatments in patients with mild to moderate disease who are neurologically stable.23,25,28,37
CONSERVATIVE TREATMENT
Conservative treatments include physical therapy, immobilization with hard or soft cervical collars, cervical traction, massage, spinal manipulation therapy, spinal injections, and avoidance of high-risk activities.5 The evidence for the effectiveness of these treatments is scarce and of low quality, and outcomes can vary with individual patients.35,38,39 Nonsurgical treatments carry some risks. For example, spinal manipulation therapy and traction can cause ischemic neurologic complications, worsened myelopathy, and facial nerve paralysis.25 Therefore, it is important to refer patients to physical therapists who are comfortable managing degenerative cervical myelopathy.
SURGICAL TREATMENT
The overall goal of surgery is spinal cord decompression and stabilization in an effort to prevent further neurologic compromise. Patients with moderate to severe myelopathic signs and symptoms (i.e., evidence of cord compression) or those with progressive disease should be evaluated by a surgeon.9,28 Patients with mild to moderate disease who have not responded to physical therapy and other conservative treatments also warrant surgical evaluation.
The treatment approach in patients with radicular symptoms and evidence of cord compression on imaging but no supporting physical examination findings is more challenging. In these patients, surgical treatment for either radiculopathy or cord compression is appropriate, especially with good follow-up and supervised rehabilitation.9,17 Asymptomatic patients with evidence of cord compression that is found incidentally should not be offered prophylactic surgery.37
Spinal alignment, number of vertebral levels involved, patient age and comorbidities, preoperative pain, and evidence of instability are factors to consider when determining the surgical approach. In general, the anterior approach is preferred when there are one or two vertebral levels involved, and the posterior approach is preferred when more than two levels are involved.8,23,40 However, it should be noted that a low-quality systematic review did not show a difference in effectiveness or safety between the two approaches.8
Possible surgical complications include C5 nerve palsy (up to 30% of patients) and injuries to the recurrent laryngeal nerve (2.7%), superficial laryngeal nerve (1.3%), or vertebral artery (4.1%).25 Surgical outcomes tend to be better in younger, nonsmoking patients who have fewer comorbidities and no gait dysfunction. Even with surgery, many patients have residual deficits, including pain, spasticity, neurogenic bladder and bowel, sleep disturbance, and difficulties with self-care.6,31
Data Sources: A PubMed search was completed in Clinical Queries using the key terms degenerative cervical myelopathy, myelopathy, cervical spine pain, imaging of cervical myelopathy, treatment of cervical myelopathy, and management of myelopathy. The search included meta-analyses, randomized clinical trials, clinical trials, and reviews. We also searched the Agency for Healthcare Research and Quality evidence reports, Clinical Evidence, Cochrane database, Essential Evidence Plus, Institute for Clinical Systems Improvement, National Guideline Clearinghouse database, and the evidence summary provided by AFP editors. Search dates: October 2019 and May 2020.