
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2021;103(2):81-89
Related letter: Additional Differential Diagnosis for Adult Hip Pain
Patient information: See related handout on hip pain in adults, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
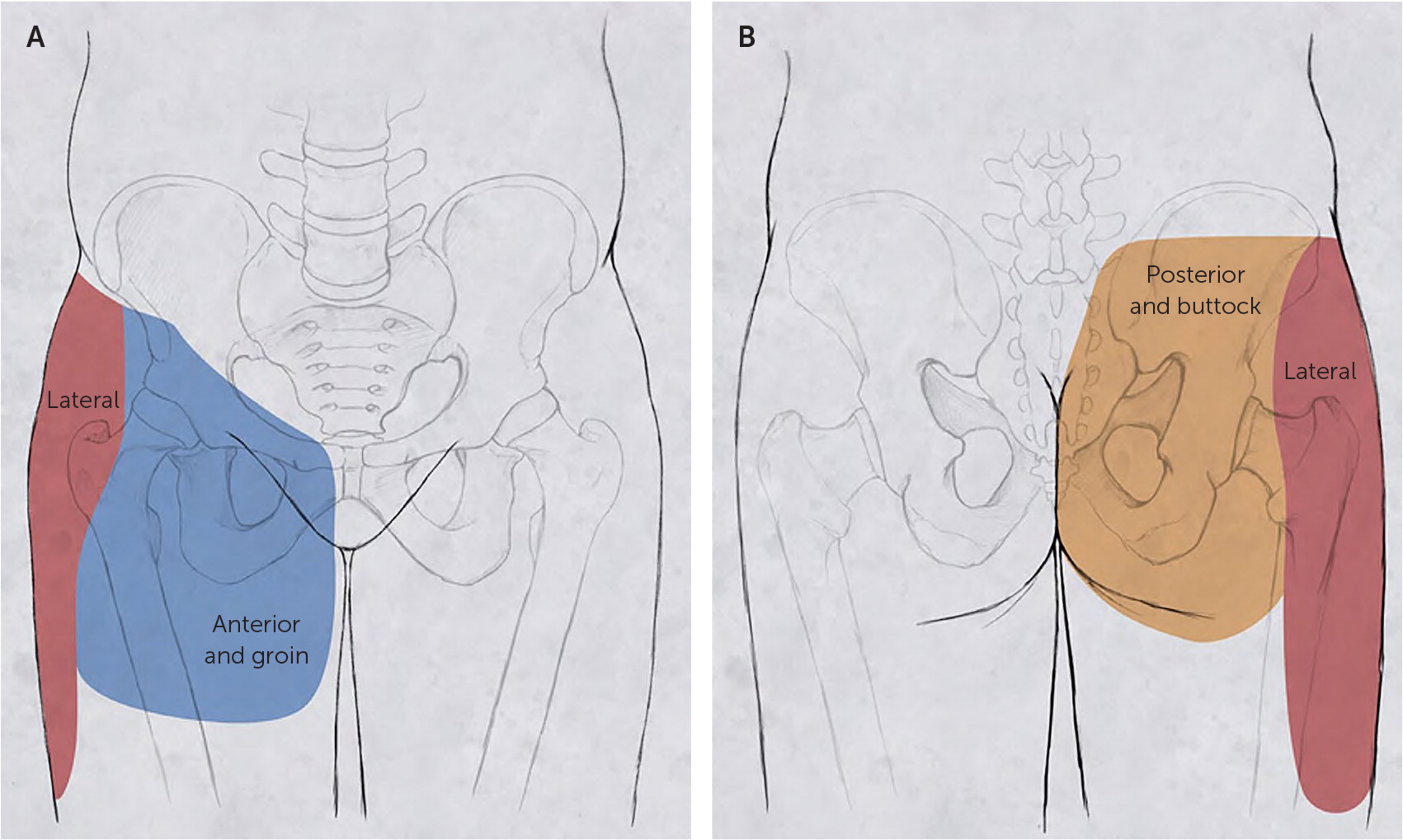
Adults commonly present to their family physicians with hip pain, and diagnosing the cause is important for prescribing effective therapy. Hip pain is usually located anteriorly, laterally, or posteriorly. Anterior hip pain includes referred pain from intra-abdominal or intrapelvic causes; extra-articular etiologies, such as hip flexor injuries; and intra-articular etiologies. Intra-articular pain is often caused by a labral tear or femoroacetabular impingement in younger adults or osteoarthritis in older adults. Lateral hip pain is most commonly caused by greater trochanteric pain syndrome, which includes gluteus medius tendinopathy or tear, bursitis, and iliotibial band friction. Posterior hip pain includes referred pain such as lumbar spinal pathology, deep gluteal syndrome with sciatic nerve entrapment, ischiofemoral impingement, and hamstring tendinopathy. In addition to the history and physical examination, radiography, ultrasonography, or magnetic resonance imaging may be needed for a definitive diagnosis. Radiography of the hip and pelvis should be the initial imaging test. Ultrasound-guided anesthetic injections can aid in the diagnosis of an intra-articular cause of pain. Because femoroacetabular impingement, labral tears, and gluteus medius tendon tears typically have good surgical outcomes, advanced imaging and/or early referral may improve patient outcomes.
Hip pain is common in adults of all ages and activity levels. In nonelite adult soccer players, hip and groin injuries represent 28% to 45% of all injuries in women and 49% to 55% in men.1 The prevalence of the cam deformity (deformity of the femoral head) is 41% in nonelite male soccer players and 17% in male nonathletes.2 In adults older than 45 years, 6.7% to 9.7% have osteoarthritis of the hip, and one in four adults will develop symptomatic hip osteoarthritis in their lifetime.3 In the United States in 2009, hip replacements accounted for $13.7 billion in health care costs.3
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| If imaging is performed in the evaluation of a patient with undifferentiated chronic hip pain, standing anteroposterior hip and pelvic radiographs should be the first choice.4,21 | C | Expert opinion and consensus guidelines |
| For patients with anterior hip pain and history suggestive of a labral tear,stress fracture of the femoral neck, orearly avascular necrosis, magnetic resonance imaging should be performed for accurate diagnosis.5,11,12,21–23 | C | Expert opinion and reviews of prospective and randomized trials |
| For intra-articular pain, ultrasound-guided anesthetic injection of the hip may be diagnostic, and corticosteroid injection may be therapeutic.30 | C | Clinical review and expert opinion |
| For patients with greater trochanteric pain syndrome not responding to conservative therapy, ultrasonography or magnetic resonance imaging should be considered to evaluate for gluteus medius tendon tears.15,16,21 | C | Clinical reviews and expert opinion |
Approach to Evaluation
| Type of pain | History | Physical examination |
|---|---|---|
| Anterior | ||
| Referred | ||
| Intra-abdominal or intrapelvic4–6 | Pain associated with urinary or bowel symptoms, cyclic pain associated with menses | Abdominal and/or pelvic examination |
| Extra-articular | ||
| Flexor tendon5,6 | Overuse activities, acute strain or injury with hip flexion activities | Pain over the hip bony prominence, anterior superior iliac spine, anterior inferior iliac spine, or pubic symphysis; pain with hip flexion strength testing |
| Intra-articular | ||
| Femoroacetabular impingement2,5,7,8 | Young, athletic patient; gradual onset; pain with hip range of motion; history of slipped capital femoral epiphysis or developmental dysplasia | Positive FADDIR and FABER test results |
| Labral tear5,9 | Young, athletic patient; acute injury (vs. gradual onset); pain with hip range of motion; mechanical symptoms | Positive FADDIR and FABER test results |
| Femoral neck stress fracture5,10 | Overuse/overtraining, energy imbalance in athletes | Antalgic gait, pain with range of motion and ambulating |
| Avascular necrosis11,12 | Middle or older age, smoking, alcohol use, systemic corticosteroid use, hemoglobinopathies, chemotherapy, metabolic syndrome, and obesity | Antalgic gait, pain with range of motion, limited range of motion |
| Osteoarthritis3,4,7,13 | Older age, gradual onset, pain with sitting or ambulating for long periods | Antalgic gait, pain with flexion and internal and external rotation, limited range of motion |
| Hip fracture4,14 | Older age, osteoporosis, fall/trauma | Inability to walk on the affected limb; shortened, externally rotated, abducted leg |
| Lateral | ||
| Greater trochanteric pain syndrome, including bursitis, gluteus medius tendinopathy or tear, external snapping, or iliotibial band friction7,15,16 | No injury, middle age, female sex, overweight, pain with sleeping on affected hip, pain aggravated by physical activity or sitting for long periods | Tenderness to palpation over the lateral hip/greater trochanter, Trendelenburg gait or positive Trendelenburg test, positive resisted external derotation test |
| Posterior | ||
| Referred pain | ||
| Intra-abdominal or intrapelvic4,17 | Pain associated with urinary or bowel symptoms, cyclic pain associated with menses | Abdominal and/or pelvic examination |
| Deep gluteal syndrome17,18 | Deep buttock pain; no injury; worse with sitting, especially in a car; sciatica (burning pain shooting down the leg) | Seated piriformis stretch test |
| Ischiofemoral impingement19 | Gradual onset of deep buttock pain that worsens with activities requiring a long stride (e.g., running) | Long-stride walking test |
| Lumbar spine or muscle4,17 | Pain in the low back (above L5) and hip/buttock, history of lumbar spinal problems | Tenderness over the lumbar spine or lumbar musculature above L5 |
| Sacroiliac joint pain17 | No history of lumbar spinal issues | Tenderness over the sacroiliac joint, no tenderness above L5 |
| Proximal hamstring tendinopathy or tear20 | Overuse injury with hip extension activities (vs. acute injury with forceful hip extension) | Tenderness to palpation over the ischial tuberosity, pain with hamstring strength testing; acute tears cause ecchymosis of the posterior thigh |
The history should include personal history of developmental hip dysplasia, slipped capital femoral epiphysis, sports activities, and injuries; family history of hip problems; and the location and quality of pain, aggravating and alleviating factors, and mechanical symptoms.4,8 Physical examination should include gait analysis with particular attention to antalgic or Trendelenburg gait, evaluation of the range of motion in the hip joint and associated pain, strength testing of the muscles overlying the hip joint, palpation of the painful area, and special tests as indicated.
If imaging is performed in the evaluation of a patient with undifferentiated chronic hip pain, standing anteroposterior hip and pelvic radiography is typically the initial imaging study.4,21 Magnetic resonance imaging (MRI) or ultrasonography may be helpful in the diagnosis, depending on history and physical examination findings.21–23
Anterior Hip Pain
Intra-articular hip pain predominately presents anteriorly.4,5 In young adults, anterior hip or groin pain that is aggravated by hip flexion or rotation warrants evaluation for intra-articular pathologies. Hip flexor strains, tears, and avulsion fractures can cause anterior hip pain, with the patient history often including a sports-related or traumatic incident consistent with a flexor injury.5 Because referred pain from intra-abdominal problems can present as anterior hip pain, the abdomen should be examined for gastrointestinal causes of pain, such as a mass; appendicitis; hernia; or pain originating in the bladder (e.g., from a mass) or the female reproductive system (e.g., from ovarian cysts).4,6
FEMOROACETABULAR IMPINGEMENT
Femoroacetabular impingement is one of the most common causes of hip pain in young adults.24 It can be caused by a cam deformity, which is bony overgrowth of the femoral head and neck, a pincer deformity of the acetabulum (too much coverage of the femoral head), or both (Figure 225). Femoroacetabular impingement often has a gradual onset without a specific injury. It usually presents earlier in the disease process with less bony changes in athletes than in nonathletes and is more bothersome to athletes whose activities require hyperflexion and wide range of motion at the hip joint.2,5,9 Positive results on the flexion adduction internal rotation and flexion abduction external rotation tests (Figure 3 and Figure 4) are indicative of intra-articular hip pathology.4,7
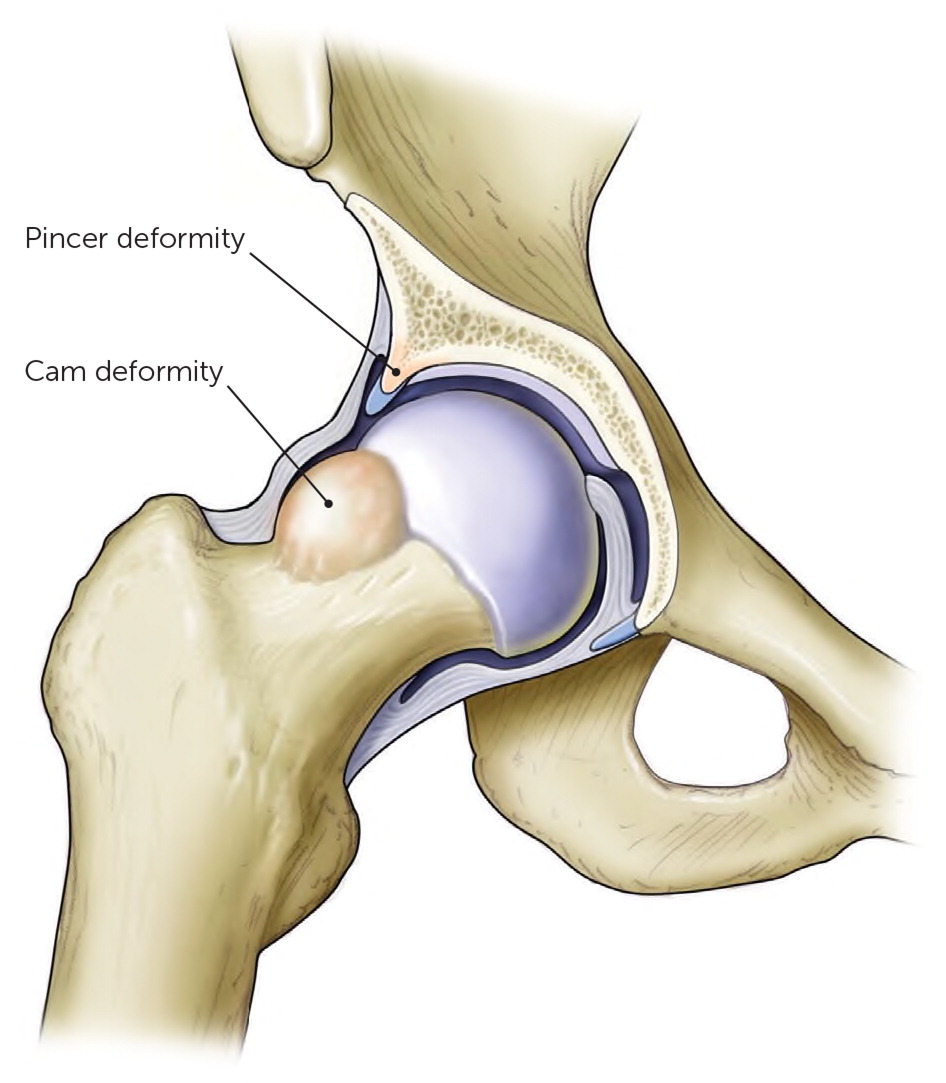

Radiography is used to help diagnose femoroacetabular impingement, although the preferred radiographic views may vary. Standing anteroposterior radiographs of the pelvis may be most helpful for diagnosing of the pincer deformity,26 whereas Meyer lateral and 90-degree Dunn views may be best to visualize the cam deformity.27
LABRAL TEARS
Patients with labral tears may present with anterior hip pain and a history of a sports-related or traumatic injury. They may also be associated with repetitive motions. Labral tears may cause a popping, catching, or clicking sound associated with activities such as dance, gymnastics, hockey, basketball, and soccer.2,5,9 Physical examination for labral tears should include flexion adduction internal rotation and flexion abduction external rotation tests.7
A standing radiograph should be the initial imaging test.24 Previously, magnetic resonance arthrography (1.5 tesla) with gadolinium injection of the hip was the diagnostic standard for labral tears. However, with recent advances to 3-tesla MRI and specialized hip protocols, noncontrast 3-tesla MRI is as sensitive and specific as magnetic resonance arthrography and does not require a procedure for contrast injection.22,23 Physicians should consult with a local radiologist to determine the most appropriate test in their area.
Labral tears and femoroacetabular impingement are often comorbid conditions in young active patients. Athletes are more likely to require surgical intervention for these conditions, especially those with both conditions.9
FEMORAL NECK STRESS FRACTURES
Stress fractures of the femoral neck are typically associated with overuse and may also be associated with energy imbalance in athletes. Femoral neck stress fractures are more common in women than men but should not be excluded in men with a history of overuse.10 Early in the disease process, stress fractures are typically not visible on radiographs and therefore MRI is required for definitive diagnosis. Early diagnosis of a femoral neck stress fracture is important because conversion to a complete fracture can be a devastating injury.5,28
AVASCULAR NECROSIS
Avascular necrosis of the femoral head most commonly presents in middle-aged to older adults. Risk factors include alcohol use, smoking, systemic corticosteroid use, hemoglobinopathies, chemotherapy, metabolic syndrome, and obesity. Early detection of avascular necrosis can be joint sparing, but no physical examination finding is specific for this diagnosis.11 Late-stage disease may be visible on a radiograph, but earlier diagnosis often requires MRI or computed tomography.12,21
OSTEOARTHRITIS
In older adults, osteoarthritis of the femoroacetabular joint is the most common cause of anterior hip pain.3 It can lead to significant morbidity and decrease in physical activity. Osteoarthritis of the hip typically has a gradual onset, but some patients recall a specific injury or fall. Patients with this condition may have pain with sitting and ambulating for long periods and may have an antalgic gait. Physical examination maneuvers such as flexion and internal and external rotation may reproduce pain, and range of motion may be decreased.4,6
Standing anteroposterior radiography of the pelvis is the radiologic test of choice and will show joint space narrowing and osteophyte formation. However, presence of these findings does not always correlate with symptom severity.7,13,29 Ultrasound-guided anesthetic injection of the hip joint may help differentiate an intra-articular cause of pain from other causes (e.g., lumbar spine or extra-articular pain), and corticosteroid injection may be therapeutic for intra-articular pain.30
HIP FRACTURES
Hip fractures are more common in older adults and often present after a fall or other trauma or may be associated with osteoporosis. Physical examination usually reveals an inability to walk on the affected limb and a shortened, externally rotated, abducted leg while in the supine position.14 Most hip fractures are visible on a radiograph and require surgical fixation.4
Lateral Hip Pain
The most common cause of lateral hip pain is greater trochanteric pain syndrome (previously called greater trochanteric bursitis).15 Although this syndrome may be associated with bursitis, gluteus medius tendinopathy or tears are now thought to be more common.16,31 Iliotibial band friction and external snapping hip can contribute to greater trochanteric pain syndrome.15
Greater trochanteric pain syndrome presents as lateral hip pain aggravated by ambulation or other physical activities, sitting for long periods, and sleeping on the affected hip. It most commonly affects women 40 to 60 years of age.16 There is typically no inciting injury. The patient may walk with a Trendelenburg gait or have positive findings on the Trendelenburg test or resisted external derotation test.7,16 (Figure 5).

If a patient with greater trochanteric pain syndrome does not improve with anti-inflammatory medications and physical therapy, a gluteus medius tendon tear should be considered. MRI and musculoskeletal ultrasonography performed by an experienced sonographer are sufficiently sensitive and specific for diagnosing a gluteus medius tendon tear.15,16,21 Referral to an orthopedic hip specialist is often indicated for large partial or complete tears because surgery is typically associated with good outcomes in patients with this condition.15,16
Posterior Hip Pain
The cause of posterior hip pain can be difficult to diagnose. The differential diagnosis includes musculoskeletal causes and referred pain from intrapelvic and gynecologic issues. Patients with intrapelvic problems may have a history of cyclic pain associated with menses or urinary or bowel symptoms.17
PIRIFORMIS AND DEEP GLUTEAL SYNDROME
Piriformis syndrome is thought to be a result of the piriformis muscle entrapping the sciatic nerve, causing hip and buttock pain and sciatica (burning pain shooting down the leg). Piriformis syndrome is a subset of deep gluteal syndrome, which includes entrapment of the sciatic nerve and/or pudendal nerve by the piriformis muscle, gemelliobturator internus, or proximal hamstrings.18 Patients with deep gluteal syndrome have deep buttock pain that is aggravated by sitting and sciatica symptoms. The seated piriformis stretch test (Figure 6) may reproduce this pain.18

Although conservative treatments are often helpful, MRI may be needed to identify pathology in the deep gluteal muscles or sciatic and pudendal nerves. Additionally, electrodiagnostic nerve testing can help localize the area of nerve entrapment.18
ISCHIOFEMORAL IMPINGEMENT
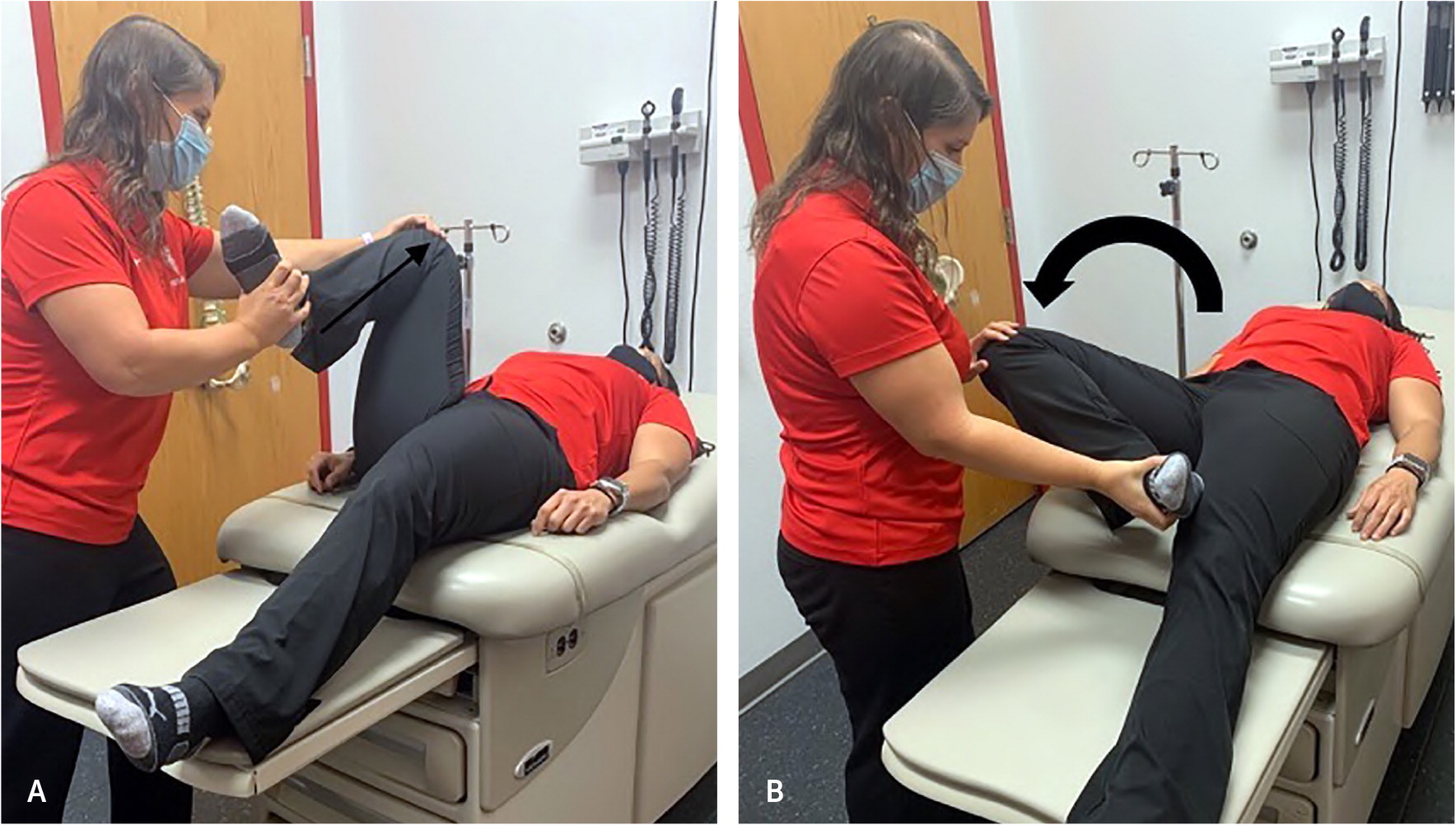
Ischiofemoral impingement is impingement of the quadratus femoris muscle and nerve between the proximal femur at the level of the lesser trochanter and the ischial tuberosity.19 Patients with ischiofemoral impingement have gradual onset of deep buttock pain that is worsened with activities requiring a long stride, such as running. The long-stride walking test (Figure 7) is the most sensitive and specific test for this condition.18,19

LUMBAR SPINE AND SACROILIAC JOINT PATHOLOGY
Lumbar spinal issues can present as posterior hip pain. Patients typically have pain in the lumbar spine or musculature and in the posterior hip/buttock area and may report previous lumbar spinal problems. Radiography of the lumbar spine may show degenerative disease, and MRI can help identify disk herniation or nerve entrapment.17
Sacroiliac joint dysfunction and/or arthritis may also present as posterior hip pain. The most common physical examination finding is tenderness to palpation over the sacroiliac joint. Sacroiliac pain typically does not occur above the L5 level, which would indicate a lumbar spinal etiology of pain.17 Radiography may show sacroiliac joint arthritis. Image-guided injections may be a helpful diagnostic and therapeutic tool. If diagnosis is uncertain, MRI can show inflammation or arthritis at the sacroiliac joint.17
HAMSTRING INJURIES
Posterior hip/buttock pain around the ischium may be indicative of a hamstring strain, tear, or avulsion. Patients may have a history of a traumatic, sports-related, or overuse injury. A complete hamstring tear or avulsion often causes ecchymosis of the posterior thigh.20 Hamstring tendinopathy or partial tears are typically exacerbated by hamstring strength testing but do not cause obvious bruising or deformity. Patients with acute tears should be referred to an orthopedic surgeon.20 If it is unclear whether the patient has a hamstring injury, MRI may be helpful in determining the diagnosis.17
This article updates previous articles on this topic by Wilson and Furukawa,4 and O'Kane.6
Data Sources: A PubMed search was conducted using the following key words, with filters set for the previous five years and humans only: hip pain, anterior hip pain, femoroacetabular impingement, gluteus medius tendinitis, hip physical exam, 3-tesla hip MRI, ultrasound guided hip injection, greater trochanteric pain syndrome, deep gluteal syndrome, ischiofemoral syndrome, hamstring avulsion. Additional searches included the Cochrane Database of Systematic Reviews and Essential Evidence Plus. Search dates: November 8, 2019, to September 30, 2020.
