
Am Fam Physician. 2021;104(6):609-617
Author disclosure: No relevant financial affiliations.
Thyroiditis is a general term for inflammation of the thyroid gland. The most common forms of thyroiditis encountered by family physicians include Hashimoto, postpartum, and subacute. Most forms of thyroiditis result in a triphasic disease pattern of thyroid dysfunction. Patients will have an initial phase of hyperthyroidism (thyrotoxicosis) attributed to the release of preformed thyroid hormone from damaged thyroid cells. This is followed by hypothyroidism, when the thyroid stores are depleted, and then eventual restoration of normal thyroid function. Some patients may develop permanent hypothyroidism. Hashimoto thyroiditis is an autoimmune disorder that presents with or without signs or symptoms of hypothyroidism, often with a painless goiter, and is associated with elevated thyroid peroxidase antibodies. Patients with Hashimoto thyroiditis and overt hypothyroidism are generally treated with lifelong thyroid hormone therapy. Postpartum thyroiditis occurs within one year of delivery, miscarriage, or medical abortion. Subacute thyroiditis is a self-limited inflammatory disease characterized by anterior neck pain. Treatment of subacute thyroiditis should focus on symptoms. In the hyperthyroid phase, beta blockers can treat adrenergic symptoms. In the hypothyroid phase, treatment is generally not necessary but may be used in patients with signs and symptoms of hypothyroidism or permanent hypothyroidism. Nonsteroidal anti-inflammatory drugs and corticosteroids are indicated for the treatment of thyroid pain. Certain drugs may induce thyroiditis, such as amiodarone, immune checkpoint inhibitors, interleukin-2, interferon-alfa, lithium, and tyrosine kinase inhibitors. In all cases of thyroiditis, surveillance and clinical follow-up are recommended to monitor for changes in thyroid function.
Thyroiditis is a general term for inflammation of the thyroid gland, and it can be associated with thyroid dysfunction. Thyroiditis is classified according to clinical symptoms (painful or painless), onset of symptoms (acute, subacute, chronic), and underlying etiology (autoimmunity, infection, drugs, radiation). Painful types of thyroiditis include subacute, suppurative, and radiation induced. Painless types include drug induced, fibrous (Riedel thyroiditis), Hashimoto thyroiditis (HT), postpartum, and silent.
| Recommendation | Sponsoring organization |
|---|---|
| Avoid routinely performing thyroid ultrasonography in children who have simple goiters or autoimmune thyroiditis. | American Academy of Pediatrics – Section on Endocrinology |
| Do not routinely perform thyroid ultrasonography in patients with abnormal thyroid function tests if there is no palpable abnormality of the thyroid gland. | Endocrine Society/American Association of Clinical Endocrinologists |
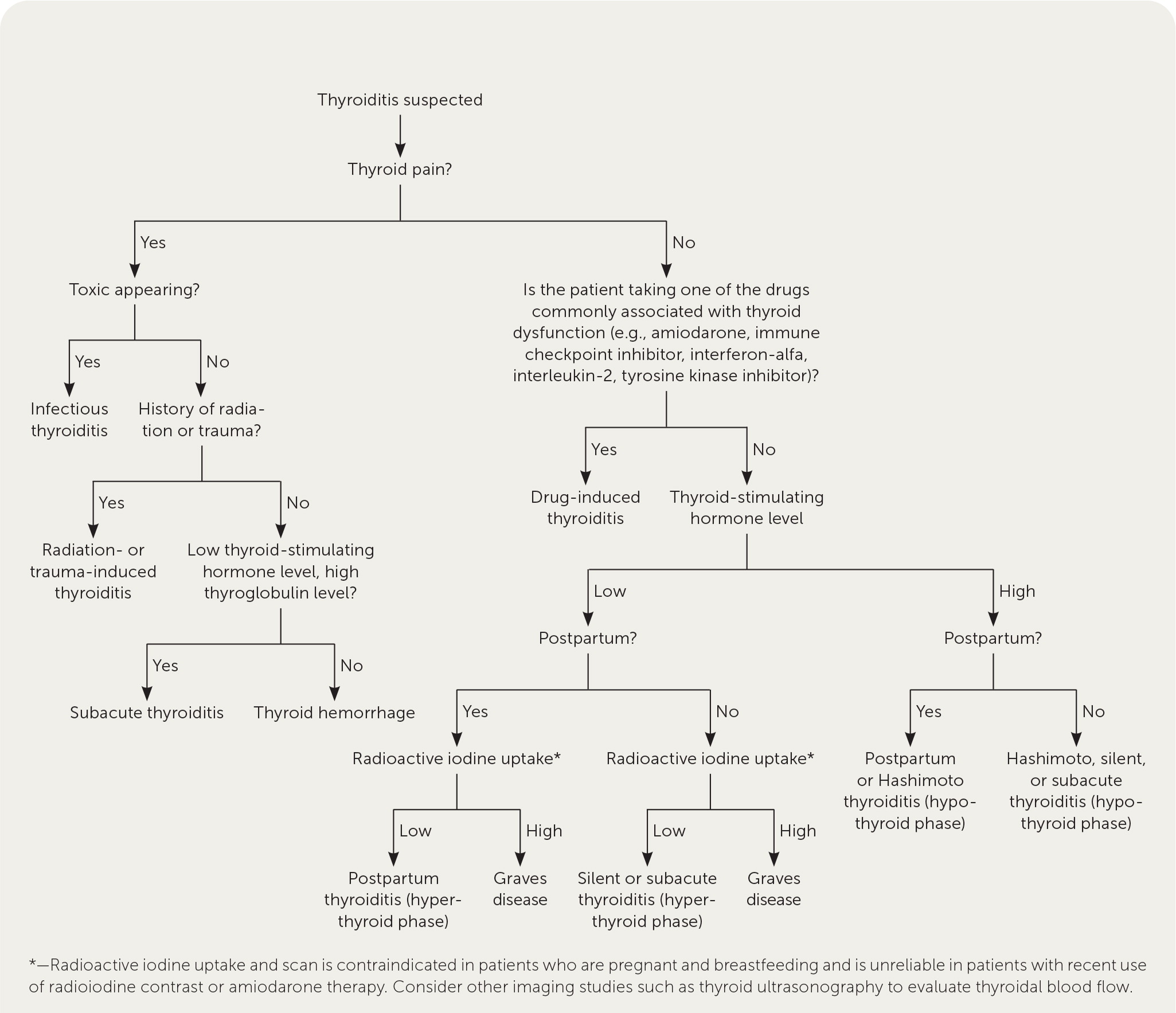
Most forms of thyroiditis result in a triphasic disease pattern of thyroid dysfunction. Patients have an initial phase of hyperthyroidism (thyrotoxicosis) attributed to the release of preformed thyroid hormone from damaged thyroid follicular cells. This is followed by hypothyroidism, when the thyroid stores are depleted, and then eventual restoration of normal thyroid function. Some patients may develop permanent hypothyroidism requiring thyroid hormone therapy with levothyroxine. The three most common forms of thyroiditis are HT, postpartum, and subacute. Table 1 summarizes the etiology, clinical presentation, diagnosis, complications, and management for different types of thyroiditis, including less common types.1–13 Figure 1 is an algorithm for the diagnosis of suspected thyroiditis.14
| Type | Etiology | Clinical presentation | Diagnosis | Complications | Management |
|---|---|---|---|---|---|
| Chronic autoimmune thyroiditis (Hashimoto thyroiditis, chronic lymphocytic thyroiditis) | Autoimmune | Painless goiter; euthyroidism, hypothyroidism, subclinical hypothyroidism, and, rarely, transient hyperthyroidism (hashitoxicosis) | Presence of atrophic thyroid gland or nontender goiter with or without compressive symptoms (e.g., dysphagia); thyroid function tests (differ with phase); TPO* and increase in thyroglobulin antibodies | Hypothyroidism | Levothyroxine |
| Drug-induced thyroiditis | See Table 2 | ||||
| Suppurative thyroiditis (infectious thyroiditis) | Multiple infectious organisms, most commonly Staphylococcus aureus, Streptococcus spp. | Anterior neck pain, swelling, tenderness, odynophagia, fever, chills, and local lymphadenopathy | Complete blood count with differential, complete metabolic panel, blood cultures; computed tomography of the neck and chest with intravenous contrast; thyroid function tests are usually normal (hypo- or hyperthyroidism may occur); thyroid antibodies are often absent; thyroid ultrasonography and fine-needle aspiration (diagnostic and therapeutic) if evidence of a mass or fluid collection | Acute complications may include sepsis and airway compromise; in some patients, destructive thyroiditis may lead to permanent hypothyroidism | Hospitalization, airway monitoring and stabilization, and empiric antibiotic therapy with penicillinase-resistant penicillin and beta-lactamase inhibitor (e.g., piperacillin/tazobactam [Zosyn]), vancomycin if methicillin-resistant S. aureus is suspected; antibiotic therapy should be adjusted to microbiology and antimicrobial susceptibility data; urgent transcutaneous or open-surgical abscess drainage is recommended if airway is compromised |
| Postpartum thyroiditis | Autoimmune | Hyperthyroidism alone, hyperthyroidism followed by transient or permanent hypothyroidism, or hypothyroidism alone within 1 year of delivery, miscarriage, or medical abortion | Presence of TPO antibodies and increase in thyroglobulin antibodies; thyroid function tests (differ with phase); low radioactive iodine uptake in the hyperthyroid phase† | Up to 70% of patients develop recurrence with subsequent pregnancies; permanent hypothyroidism occurs in 15% to 50% of women | Beta blockers for hyperthyroid symptoms; levothyroxine for symptomatic hypothyroidism or patients who are attempting pregnancy or breastfeeding (in the hypothyroid phase), and permanent hypothyroidism |
| Radiation-induced thyroiditis | Radiation (radioiodine and external radiation) | Anterior neck pain, thyroid gland enlargement and tenderness; transient hyperthyroidism; occurs typically within 2 weeks after radiation | Clinical diagnosis made in the setting of recent radiation | Self-limited; hyperthyroidism generally resolves within 1 month | Beta blockers for hyperthyroid symptoms; NSAIDs usually provide sufficient analgesia, and prednisone (20 to 40 mg per day) is rarely required for thyroid pain |
| Riedel thyroiditis (fibrous thyroiditis) | Unknown, auto-immunity may contribute to the pathogenesis | Destructive thyroiditis characterized by dense fibrosis that can extend into adjacent tissues; firm goiter; compressive symptoms (e.g., hoarseness, dyspnea, dysphagia); hypocalcemia may occur due to fibrotic transformation of the parathyroid glands | Thyroid biopsy | Most patients are euthyroid, approximately 30% develop hypothyroidism | No standardized treatment; glucocorticoids with mycophenolate mofetil (Cellcept) or tamoxifen have been described in the literature, subtotal thyroidectomy is indicated to relieve compressive symptoms |
| Silent thyroiditis (silent sporadic thyroiditis, painless sporadic thyroiditis, subacute lymphocytic thyroiditis) | Autoimmune | Hyperthyroidism alone, hyperthyroidism followed by hypothyroidism, or hypothyroidism alone | Increase in TPO antibodies; thyroid function tests (differ with phase); low radioactive iodine uptake in the hyperthyroid phase | 10% to 20% of patients develop permanent hypothyroidism; 5% to 10% recurs | Beta blockers for hyperthyroid symptoms; levothyroxine for symptomatic hypothyroidism (in the hypothyroid phase) and permanent hypothyroidism |
| Subacute thyroiditis (granulomatous thyroiditis, giant cell thyroiditis, de Quervain thyroiditis) | Post-viral | Anterior neck pain, dysphagia, reported recent upper respiratory tract infection; hyperthyroidism followed by transient hypothyroidism, and eventual restoration of thyroid function | Thyroid function tests (differ with phase); elevated erythrocyte sedimentation rate and C-reactive protein level; increase in TPO antibodies (up to 25% of patients have low titers); low radioactive iodine uptake in the hyperthyroid phase | Self-limited; most patients are euthyroid within 12 months of onset; 5% to 15% of patients develop permanent hypothyroidism; 1% to 4% recurs | Beta blockers for hyperthyroid symptoms; NSAIDs (e.g., ibuprofen, 1,200 to 3,200 mg per day in divided doses) and steroids (prednisone, 15 to 40 mg per day for 1 to 6 weeks, then taper) for thyroid pain; levothyroxine for hypothyroidism |
Hashimoto Thyroiditis (Chronic Autoimmune Thyroiditis)
EPIDEMIOLOGY
HT (i.e., chronic autoimmune thyroiditis or chronic lymphocytic thyroiditis) is the most commonly encountered autoimmune disease worldwide.1,15 The estimated incidence of HT is 0.3 to 1.5 cases per 1,000 people per year.2 HT may present with other autoimmune disorders, such as type 1 diabetes mellitus, Addison disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren syndrome, autoimmune hepatitis, and vitiligo.1,16 HT occurs due to the formation of autoantibodies and direct injury to the thyroid from an environmental trigger (e.g., infection, stress, iodine intake) in patients with genetic susceptibility. The degree of injury can differ among individuals but is often progressive over time and can result in fibrotic transformation of the gland.17
CLINICAL PRESENTATION
Patients with HT often present with a painless goiter, with or without overt hypothyroidism.1 In patients who are asymptomatic, HT is usually the incidental finding of the goiter that prompted an evaluation. Other patients may report typical symptoms of hypothyroidism such as fatigue, weight gain, cold intolerance, constipation, depression, myalgia, menorrhagia, and dry skin. Many of these symptoms overlap with other disorders and may not always correlate with the degree of thyroid dysfunction. In a 20-year follow-up study, clinical or biochemical hypothyroidism developed in 55% of the women who initially had positive thyroid antibodies and an elevated thyroid-stimulating hormone (TSH) level (greater than 6 mIU per L) but a normal serum free thyroxine (T4) level.15
DIAGNOSIS
The diagnosis of HT can be established by a combination of clinical features, thyroid function test results consistent with subclinical hypothyroidism (elevated serum TSH level, but normal serum levels of T4 and free triiodothyronine [T3]) or overt hypothyroidism (elevated TSH level with low T4 and T3 serum levels), and elevated thyroglobulin and thyroid peroxidase (TPO) antibodies.1,15 TPO antibodies are found in 95% of patients with HT, whereas thyroglobulin antibodies are elevated in 60% to 80% of patients with HT.1 Some patients may present with self-limited transient thyrotoxicosis or a hyperthyroid phase (i.e., hashitoxicosis) caused by destructive inflammation attributed to HT damaging the thyroid follicles, releasing excess thyroid hormone.18 The thyroid gland is often diffusely enlarged and firm with an irregular surface on examination.15 Some patients have a small thyroid volume if underlying atrophy of the thyroid gland has occurred.2 Patients with goiter may have compressive symptoms such as dysphonia, dyspnea, and dysphagia.1
TREATMENT
All patients with HT and hypothyroidism require treatment, even if they are asymptomatic. The goals of treatment include normalizing the TSH level and ameliorating symptoms of hypothyroidism. When deciding on the initial replacement dose of levothyroxine, the patient's age and cardiac status should be considered. A healthy, young patient without coexisting heart disease can be started on a full replacement dosage of levothyroxine (1.6 mcg per kg per day). A lower dosage of levothyroxine (12.5 to 25 mcg per day) is appropriate in older adults, patients with underlying coronary heart disease, and those with tachyarrhythmias such as atrial fibrillation. Treatment with T3 is not routinely recommended. The patient's TSH level should be remeasured four to six weeks after initiation and the dose of levothyroxine adjusted to achieve a value in the normal reference range (0.5 to 4.0 mIU per L). Clinicians may try to achieve slightly higher TSH levels (4.0 to 6.0 mIU per L) in older patients. It is reasonable to make dosage adjustments of 12.5 to 25 mcg of levothyroxine per day at four- to six-week intervals until the intended TSH level is reached.
In patients with subclinical hypothyroidism and elevated TPO antibodies, especially those with a serum TSH level of at least 10 mIU per L or with symptoms, treatment with low-dose levothyroxine should be considered. An initial dosage of 25 to 50 mcg per day can be established and titrated in these patients similarly to patients who have overt hypothyroidism. If therapy with levothyroxine is not initiated, patients should be monitored annually for the development of overt hypothyroidism.15,19
Postpartum Thyroiditis
EPIDEMIOLOGY
Postpartum thyroiditis is an autoimmune-mediated destructive thyroiditis that results in transient or persistent thyroid dysfunction and occurs within one year of delivery, miscarriage, or medical abortion. The lifetime incidence of postpartum thyroiditis is 5.4% in the general population and is increased in individuals with other autoimmune diseases such as type 1 diabetes or a personal or family history of thyroid disease.6,12 Recurrence rates approach 70% with each subsequent pregnancy.12
CLINICAL PRESENTATION
Postpartum thyroiditis is a painless condition. A total of 40% of patients with postpartum thyroiditis present with isolated hypothyroidism, whereas 25% to 40% experience a triphasic pattern of hyperthyroidism (thyrotoxicosis), followed by hypothyroidism and then euthyroidism. During the thyrotoxic phase, symptoms are usually mild and begin two to six months postpartum. This phase typically lasts two to three months. The hypothyroid phase occurs three to 12 months postpartum and is often symptomatic.12
DIAGNOSIS
The differential diagnosis in the thyrotoxic phase includes Graves disease, which can also present during the postpartum period.7 Measurement of thyroid antibodies can help distinguish between postpartum thyroiditis and Graves disease. The presence of thyrotropin receptor antibodies usually indicates Graves disease. Elevated TPO and thyroglobulin antibodies are often found in patients with postpartum thyroiditis, and mildly positive thyrotropin receptor antibodies have also been reported.12,20 In postpartum thyroiditis, there is a release of preformed thyroid hormone, and the T4:T3 ratio is usually higher than in Graves disease. Physical examination features specific to Graves disease, such as exophthalmos and thyroid bruit, are not found in postpartum thyroiditis. Radioactive iodine uptake and scan will generally find a decreased uptake in postpartum thyroiditis and increased diffuse uptake in Graves disease. This imaging is contraindicated in patients who are pregnant or breastfeeding.7,12,21
TREATMENT
Treatment with beta blockers (e.g., propranolol, 10 to 20 mg every eight hours), titrated to a dosage that provides symptomatic relief, is recommended for patients who are symptomatic during the thyrotoxic phase.21 Postpartum thyroiditis is a destructive process, and antithyroid medications are not indicated.6,22 Treatment of the hypothyroid phase with levothyroxine is recommended, especially if the patient is symptomatic, attempting pregnancy, or breastfeeding. Thyroid function testing should be performed every four to eight weeks. It is recommended to begin tapering the levothyroxine dose around 12 months postpartum if the patient is not pregnant, attempting to conceive, or breastfeeding, followed by periodic monitoring of thyroid function. The eventual development of permanent hypothyroidism has been described in 15% to 50% of patients with a history of postpartum thyroiditis.12 Those with a history of postpartum thyroiditis should have an annual TSH test to evaluate for permanent hypothyroidism.22
Subacute Thyroiditis
EPIDEMIOLOGY
Subacute thyroiditis (i.e., subacute granulomatous thyroiditis or de Quervain thyroiditis) is a self-limited inflammatory disease of the thyroid gland. The incidence has been reported at 4.9 cases per 100,000 people per year.16 Women are more likely to be affected, with a peak incidence between 40 and 50 years of age.23,24 More cases are noted in the late summer and fall.23,24 Subacute thyroiditis results from the inflammatory destruction of thyroid follicles; the condition often occurs after infection of the upper respiratory tract caused by Coxsackie virus, Epstein-Barr virus, adenovirus, influenza viruses, and most recently SARS-CoV-2 virus.12,25 However, 25% of patients report symptoms of an upper respiratory tract infection in the 30 days before initial presentation.23,24
CLINICAL PRESENTATION
Subacute thyroiditis is the most common cause of thyroid pain. Anterior neck pain is usually the presenting feature and prompts patients to seek medical attention. The neck pain can be unilateral or bilateral and may radiate to the jaw or ear.23,24,26 Dysphagia may be present due to diffuse thyroid gland enlargement (i.e., up to three to four times its normal size). Patients may also present with a prodrome of fatigue, myalgias, low-grade fever, and pharyngitis. Most cases of subacute thyroiditis follow the triphasic pattern. About 50% of patients present with the thyrotoxic phase, which typically lasts for three to six weeks. Symptoms are often mild and may include diaphoresis, heat intolerance, tremors, palpitations, and weight loss. Following the thyrotoxic phase, one-third of patients develop hypothyroidism, which can last up to six months. There is no thyroid pain during this phase. Most patients return to euthyroidism within 12 months of the onset of disease. Between 5% and 15% of patients develop permanent hypothyroidism.12
DIAGNOSIS
The diagnosis of subacute thyroiditis is mainly clinical. During the initial thyrotoxic phase, the patient presents with anterior neck pain, tenderness to palpation of the thyroid gland, and signs and symptoms of thyrotoxicosis. Inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are elevated. In the thyrotoxic phase, TSH is usually suppressed with elevated or normal T4 and T3 levels. To differentiate from other causes of thyrotoxicosis, radioactive iodine uptake and scan should be performed to demonstrate diffusely low iodine uptake in the thyroid gland during the thyrotoxic phase.12 The differential diagnosis of thyroid pain includes hemorrhage into a thyroid cyst and suppurative thyroiditis caused by a bacterial infection.27 Imaging is not usually necessary; however, thyroid ultrasonography could help distinguish between these entities. Thyroid ultrasonography in subacute thyroiditis typically shows heterogeneous hypoechoic parenchyma and decreased vascularity, whereas acute thyroid hemorrhage and suppurative thyroiditis show a focal cystic and/or solid mass in the area of the thyroid pain.27,28 Patients with severe thyroid pain and systemic symptoms (e.g., high fever, leukocytosis, cervical lymphadenopathy) should have fine-needle aspiration to rule out suppurative thyroiditis.28 Otherwise, fine-needle aspiration is not routinely recommended.
TREATMENT
The goal of treatment is to ameliorate the pain and thyrotoxicosis-related symptoms. Antibiotics have no role in the treatment of subacute thyroiditis.26 Because subacute thyroiditis is a destructive process, the use of antithyroid drugs is not indicated. Treatment with beta blockers for control of severe symptoms during the thyrotoxic phase is recommended, although often no treatment is needed if symptoms are mild.12 In the thyrotoxic and painful phase, patients may be treated with high-dose acetylsalicylic acid, nonsteroidal anti-inflammatory drugs (NSAIDs), or corticosteroids. 26 NSAIDs are considered the first-line treatment (e.g., ibuprofen, 1,200 to 3,200 mg per day in divided doses). Glucocorticoids are used for severe cases or if acetylsalicylic acid or NSAIDs were not effective after four days of therapy.12,26 Pain resolution is faster with glucocorticoids than with NSAIDs.12 Prednisone in dosages of 15 to 40 mg per day has been proposed for one to six weeks, followed by tapering dosages of 5 mg every two weeks.12,13,23 During the transient hypothyroid phase, thyroid hormone supplementation is used for patients with signs and symptoms of hypothyroidism or in patients of reproductive age who wish to become pregnant. Levothyroxine should be used for 12 months and may then be discontinued because subacute thyroiditis is generally self-limited.12
Drug-Induced Thyroiditis
Several drug therapies have been associated with the development of thyroiditis, including amiodarone, immune checkpoint inhibitors, interferon-alfa, interleukin-2, lithium, and tyrosine kinase inhibitors. Table 2 summarizes these drugs and the resulting thyroid dysfunction.21,29–46 Management begins with discontinuing the medication and treating acute symptoms.
| Drug | Clinical use | Thyroid dysfunction | Mechanism |
|---|---|---|---|
| Amiodarone | Atrial fibrillation, ventricular arrhythmia | Hypo- or hyperthyroidism | Hypothyroidism: direct toxic effect on the thyroid gland Hyperthyroidism: 2 types of amiodarone-induced thyrotoxicosis In type 1, there is increased synthesis of thyroid hormone (usually in patients with preexisting goiter); in type 2, there is excess release of free thyroxine and free triiodothyronine due to destructive thyroiditis |
| Immune check-point inhibitors | Treatment of diverse types of cancer (e.g., melanoma, non–small cell lung cancer, small cell lung cancer, hepatocellular carcinoma, renal cell carcinoma, triple-negative breast cancer) | Hypo- or hyperthyroidism | Destructive thyroiditis mediated by cytotoxic T cells against the thyroid gland |
| Interferon-alfa | Hairy cell leukemia, follicular lymphoma, melanoma, AIDS-related Kaposi sarcoma, chronic hepatitis B and C | Hypo- or hyperthyroidism Chronic autoimmune thyroiditis Silent thyroiditis | Autoimmune |
| Interleukin-2 | Renal cell carcinoma, melanoma | Hypo- more often than hyperthyroidism | Autoimmune |
| Lithium | Depression, bipolar disorder | Goiter Hypo- more often than hyperthyroidism Chronic autoimmune thyroiditis | Impaired iodine uptake; inhibition of thyroid hormone synthesis and release; increased thyroid autoimmunity; direct toxic effect on the thyroid gland |
| Tyrosine kinase inhibitors | Treatment of diverse types of cancer (e.g., non–small cell lung cancer, chronic myelogenous leukemia, renal cell carcinoma, breast cancer, hepatocellular carcinoma, colorectal cancer) | Hypothyroidism | Destructive thyroiditis; impaired iodine uptake; capillary regression induced by vascular endothelial growth factor inhibition; inhibition of thyroid peroxidase activity |
This article updates previous articles on this topic by Sweeney, et al.,14 Bindra and Braunstein,47 and Slatosky, et al.48
Data Sources: A PubMed search was completed in Clinical Queries using the key terms thyroiditis, subacute thyroiditis, subacute granulomatous thyroiditis, postpartum thyroiditis, silent thyroiditis, chronic lymphocytic thyroiditis, Hashimoto's thyroiditis, drug-induced thyroiditis, steroid therapy and thyroiditis, COVID-19 and thyroiditis, immune-checkpoint inhibitor therapy and thyroiditis, ICI-related thyroiditis. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were UpToDate and Essential Evidence Plus. Search dates: November 2020 through March 2021, and July 2021.
The views expressed in this article are those of the authors and do not reflect the policy or position of the U.S. Army Medical Department, Department of the Army, Department of Defense, or the U.S. government.
