
Am Fam Physician. 2022;105(2):144-151
Author disclosure: No relevant financial relationships.
Hemoptysis is the expectoration of blood from the lower respiratory tract, usually from bronchial arteries. The most common causes are acute respiratory infections, cancer, bronchiectasis, and chronic obstructive pulmonary disease. No cause is identified in 20% to 50% of cases. Hemoptysis must be differentiated from pseudohemoptysis, which is blood that originates from nasopharyngeal or gastrointestinal sources. The initial evaluation includes determining the severity of bleeding and stability of the patient and may require bronchoscopy for airway protection. Mild hemoptysis comprises more than 90% of cases and has a good prognosis, whereas massive hemoptysis has a high mortality rate. A history and physical examination can assist in identifying an etiology, but diagnostic testing is often required. Chest radiography is a good initial test, but it has limited sensitivity for determining the site and etiology of the bleeding. Computed tomography and computed tomography angiography of the chest with intravenous contrast are the preferred modalities to determine the etiology of bleeding; however, bronchoscopy may also be needed. In addition to supportive medical treatment, management should include treatment of the underlying etiology because recurrence often takes place in the absence of treatment of the identified cause. Bronchial arterial embolization is used to treat massive hemoptysis, particularly when an involved artery is noted on computed tomography angiography. Surgery is reserved for patients whose medical treatment and embolization are not effective.
Hemoptysis is the expectoration of blood from the lower respiratory tract (airways or lungs).1–6 The expectoration of blood-tinged sputum and mild to moderate hemoptysis should be distinguished from life-threatening, massive hemoptysis.4 More than 90% of hemoptysis cases are mild, self-limiting, and have a good prognosis with conservative management.5,7 However, massive hemoptysis has a mortality rate of greater than 50%.3,5,6,8
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Chest radiography should be performed as part of the initial evaluation of patients with hemoptysis.2,3,5 | C | Expert opinion |
| Computed tomography or computed tomography angiography with intravenous contrast should be performed to determine the etiology of hemoptysis when no cause is found on chest radiography.2,17,19 | C | Retrospective cohort studies showing that computed tomography with intravenous contrast is more effective in determining site and etiology of bleeding compared with bronchoscopy in patients with hemoptysis |
| Bronchial arterial embolization is the treatment of choice in patients with massive hemoptysis, and in patients with non-massive hemoptysis with a bleeding artery identified on computed tomography angiography.2,7,8 | C | Retrospective studies showing better outcomes of patients with hemoptysis who undergo bronchial arterial embolization compared with conservative treatment |
Causes
The differential diagnosis of hemoptysis is broad, with the incidence of various etiologies depending on geographic location and care setting (Table 11,3–6,9 and Table 210–13). Worldwide, tuberculosis is the most common cause of hemoptysis.2 In ambulatory settings of countries without limited resources, hemoptysis is often caused by acute respiratory infections, chronic obstructive pulmonary disease, cancer, and bronchiectasis.2,10,11 However, 20% to 50% of cases are cryptogenic, with no cause found on computed tomography (CT) or bronchoscopy.3–5
| Pulmonary: airway/tracheobronchial | Bronchial tumors, carcinomas, metastases Bronchiectasis (cystic fibrosis) Bronchitis (viral, bacterial [Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis]) Foreign body Trauma (hematoma, fistula) | ||
| Pulmonary: parenchymal | Infectious Fungal infections (mycetomas [aspergillosis], paragonimiasis) Leptospirosis Lung abscess Parasitic diseases Pneumonia Tuberculosis, nontuberculous mycobacteria | ||
| Rheumatologic diseases Anti–glomerular basement membrane disease (Goodpasture syndrome) Antiphospholipid syndrome Behçet disease Granulomatosis with polyangiitis and microscopic polyangiitis (Wegener granulomatosis) Henoch-Schönlein purpura Microscopic polyarteritis Mixed cryoglobulinemia Sarcoidosis Systemic lupus erythematosus Takayasu arteritis | |||
| Other Acute lung allograft rejection Cocaine inhalation Diffuse alveolar damage Idiopathic pulmonary hemosiderosis Lung contusion Lymphangiomyomatosis Pulmonary capillary hemangiomatosis | |||
| Vascular | Aneurysms, pseudoaneurysms (thoracic artery, bronchial artery, aorta) Arteriovenous malformations Artery rupture (pulmonary artery, thoracic artery) Bronchial telangiectasia, hemangioma Bronchovascular fistula Dieulafoy lesion Pulmonary embolism/infarction Pulmonary hypertension Pulmonary veno-occlusive disease | ||
| Cardiac | Pulmonary edema (e.g., heart failure, mitral stenosis, congenital heart disease) Right-sided endocarditis | ||
| Latrogenic | Medication: anticoagulation, thrombolytic/fibrinolytic agents, anti-angiogenics (bevacizumab [Avastin]) Postprocedural: lung biopsy, heart catheterization, endoscopic lung volume reduction, pulmonary artery catheterization, bronchoscopy, airway stent, endotracheal tube erosion | ||
| Miscellaneous | Coagulopathy Thoracic/pulmonary endometriosis (catamenial hemoptysis) Thrombocytopenia | ||
| Pseudohemoptysis | Gastrointestinal source (hematemesis):ulcer, gastritis, variceal bleed Serratia marcescens (gram-negative bacterium that produces a red pigment) Upper respiratory airway source | ||
| Etiologies | Outpatient (%) | Inpatient (%) | Limited-resource country, inpatient (%) | Pediatric (%) |
|---|---|---|---|---|
| Aspergillosis | 0.02 | 1.2 | – | – |
| Asthma | 3.2 | – | – | – |
| Bronchiectasis | 1.0 | 6.9 | 9.3 | – |
| Cancer | 4.0 | 17.8 | 6.25 | 7 |
| Cardiac/pulmonary edema | 0.2 | 4.6 | 1.56 | 11 |
| Chronic obstructive pulmonary disease | 2.5 | – | – | – |
| Coagulopathy/anticoagulation | 0.04 | 13.5 | – | – |
| Cryptogenic/idiopathic | – | 48.9 | 1.56 | 20 |
| Pulmonary embolism | 0.8 | 2.8 | – | – |
| Respiratory infections | 18.7 | 23.1 | 10.7 | 65 |
| Tuberculosis | 0.2 | 2.5 | 65 | – |
The etiology of hemoptysis often determines the source of bleeding. In 90% of cases of severe hemoptysis requiring treatment, bleeding is from the bronchial arteries.4–6 Bleeding from the pulmonary arteries (5%) and nonbronchial systemic arteries (5%) is less common.4,6 Bronchial arteries supply the intrapulmonary airways and are connected to pulmonary arteries by anastomoses.4–6 When pulmonary arterial perfusion is impaired (e.g., pulmonary embolism, vasculitis, hypoxic pulmonary vasoconstriction), increases in bronchial arterial flow result in greater flow through the anastomoses, which can hypertrophy, become thin-walled, and break into alveoli and bronchi, causing hemoptysis.5,6 Bleeding from pulmonary arteries usually results from pseudoaneurysms that are created by erosion of the artery caused by the destruction of nearby pulmonary parenchyma from chronic inflammation (e.g., cancer, tuberculosis, aspergillosis/mycetoma, lung abscess, trauma [e.g., Swan-Ganz catheter placement]).4,5,8 In inflammatory states, angiogenic growth factors cause neovascularization and recruitment of collateral vessels from nearby nonbronchial systemic arteries, which form anastomoses with the pulmonary arterial circulation that are fragile and can rupture into airways, causing hemoptysis.5,6,8,14
Initial Evaluation
Massive hemoptysis, previously defined as a specific volume of expectorated blood within a particular amount of time, has transitioned to a more functional definition focused on the effects of the bleeding.3–6 The definition has shifted because of the difficulty in quantifying the volume of hemoptysis.1,4 Clinical factors such as the rate of bleeding, the patient's ability to maintain a patent airway (dependent on the rate of blood clearance, internalized bleeding, airway obstruction, and respiratory status), and the patient's physiologic reserve (a function of hemodynamic stability, cardiopulmonary reserve, and risk of recurrent bleeding) are more important than volume.4,5 The mortality rate from untreated massive hemoptysis is greater than 50%.8 The most immediate life-threatening risk is usually asphyxia due to airway obstruction, rather than exsanguination; therefore, any degree of hemoptysis causing cardiovascular collapse should be considered life-threatening.5,6
HISTORY AND PHYSICAL EXAMINATION
Initial evaluation of hemoptysis includes a primary assessment to ensure the patient's stability and to identify life-threatening hemoptysis. This involves evaluating signs of airway obstruction and respiratory failure such as dyspnea, tachypnea, increased work of breathing, wheezing, cyanosis, altered mental status and hypoxia, and signs of hemodynamic instability, such as hypotension and tachycardia.4,6 These findings require a transfer to an emergent or intensive care setting where workup can immediately follow airway and hemodynamic stabilization.
In cases of non–life-threatening hemoptysis where the clinical timeline and coexistent symptoms allow for a complete history and physical examination, goals of the initial evaluation include confirming the hemoptysis, locating the site of bleeding, and determining the etiology of the bleeding.
The confirmation of hemoptysis requires distinguishing it from pseudohemoptysis (Table 33,4). This may be accomplished through direct observation of bleeding or, based on accompanying symptoms, the appearance of blood, and patient comorbidities. The oral cavity and nasal fossa must be examined to ensure the bleeding is subglottic, noting that nasal or gingival bleeding overnight may result in hemoptysis the following morning. Occasionally, endoscopic evaluations, which may include nasal endoscopy and upper gastrointestinal endoscopy, may be needed to confirm hemoptysis vs. pseudohemoptysis.
| Etiology | Hemoptysis | Pseudohemoptysis | ||
|---|---|---|---|---|
| Cardiorespiratory | Gastrointestinal | Upper respiratory (mouth, nose, throat) | Serratia marcescens | |
| Associated symptoms and findings | Cough, dyspnea, chest pain Anemia is rare | Abdominal pain/tenderness, nausea/vomiting, black/tarry stools, history or signs of chronic hepatic disease, chronic nonsteroidal anti-inflammatory drug use, heavy alcohol use, history of peptic ulcer disease Anemia frequently associated | Bleeding in oral cavity or nasal fossa (epistaxis, bleeding gums, gingivitis, telangiectasias, ulcers, varices) | Recent hospitalization, mechanical ventilation, presence of invasive device, recent procedure |
| Characteristics of blood | Bright red, foamy Alkaline pH | Coffee ground (dark brown/black), mixed with food particles, present in nasogastric aspirate Acidic pH | Bright red Also present in upper respiratory tract | No red blood cells in sputum |
| Possible diagnostic tests | Chest radiography, computed tomography, computed tomography angiography, bronchoscopy | Esophagogastroduodenoscopy | Nasopharyngoscopy | Positive culture |
History and physical examination should focus on determining the etiology of bleeding (Table 4).1 The presence of symptoms suggestive of infection; recent surgical procedures; administration of anticoagulant or antiplatelet medications; or a known history of tuberculosis, malignancy, an autoimmune condition, or chronic lung disease may suggest a likely etiology. Factors such as recent travel, immobilization, and a family history with clotting disorders and a history of bleeding may further indicate etiologies. Physical examination findings may assist in determining the etiology but may suggest other systemic disease processes such as ecchymosis, clubbing, synovitis, or dermatologic signs of autoimmune disease. It is important to determine the cause of bleeding even if it has stopped because management includes treatment of the underlying etiology.6,8
| Clinical clues | Suggested diagnoses/etiology |
|---|---|
| Anticoagulant use History of cirrhosis, hepatic disease, or renal disease History of thrombocytopenia Personal or family history of bleeding disorders Symptoms or signs of bleeding in other areas of the body | Coagulatory cause |
| B symptoms (fever, weight loss) | Cancer, tuberculosis, rheumatologic disease |
| Cough, sputum production | Bronchitis, chronic obstructive pulmonary disease, bronchiectasis, pneumonia, tuberculosis |
| Fever | Bronchitis, pneumonia, lung abscess, pulmonary embolism, tuberculosis, neoplasm |
| History of heart disease (valvular, heart failure) | Pulmonary edema |
| Personal or family history of venous thromboembolism or thrombophilia Recent immobilization or flight Recent surgery | Pulmonary embolism |
| Smoking history | Bronchitis, chronic obstructive pulmonary disease, cancer, bronchiectasis |
DIAGNOSTIC EVALUATION
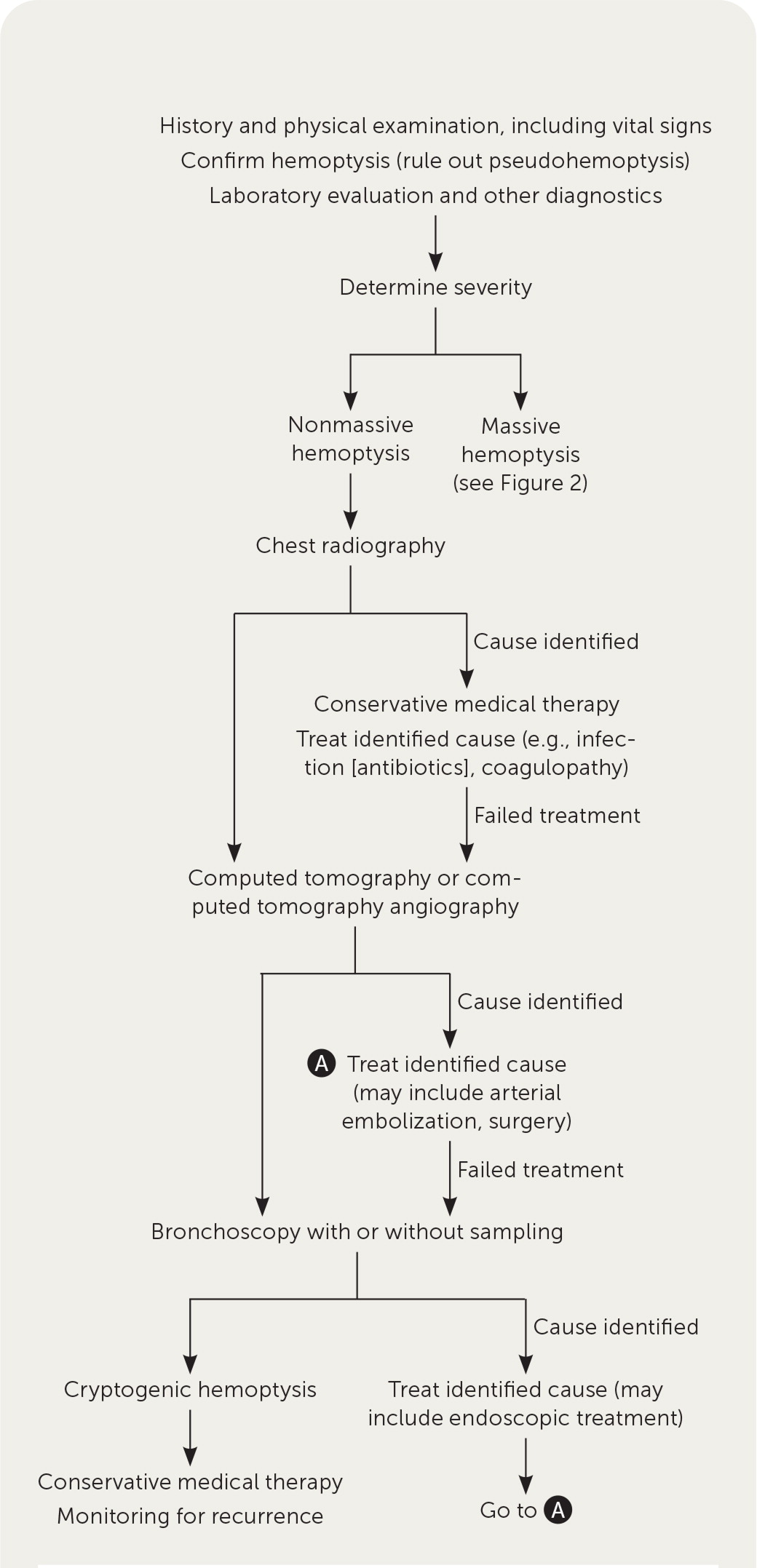
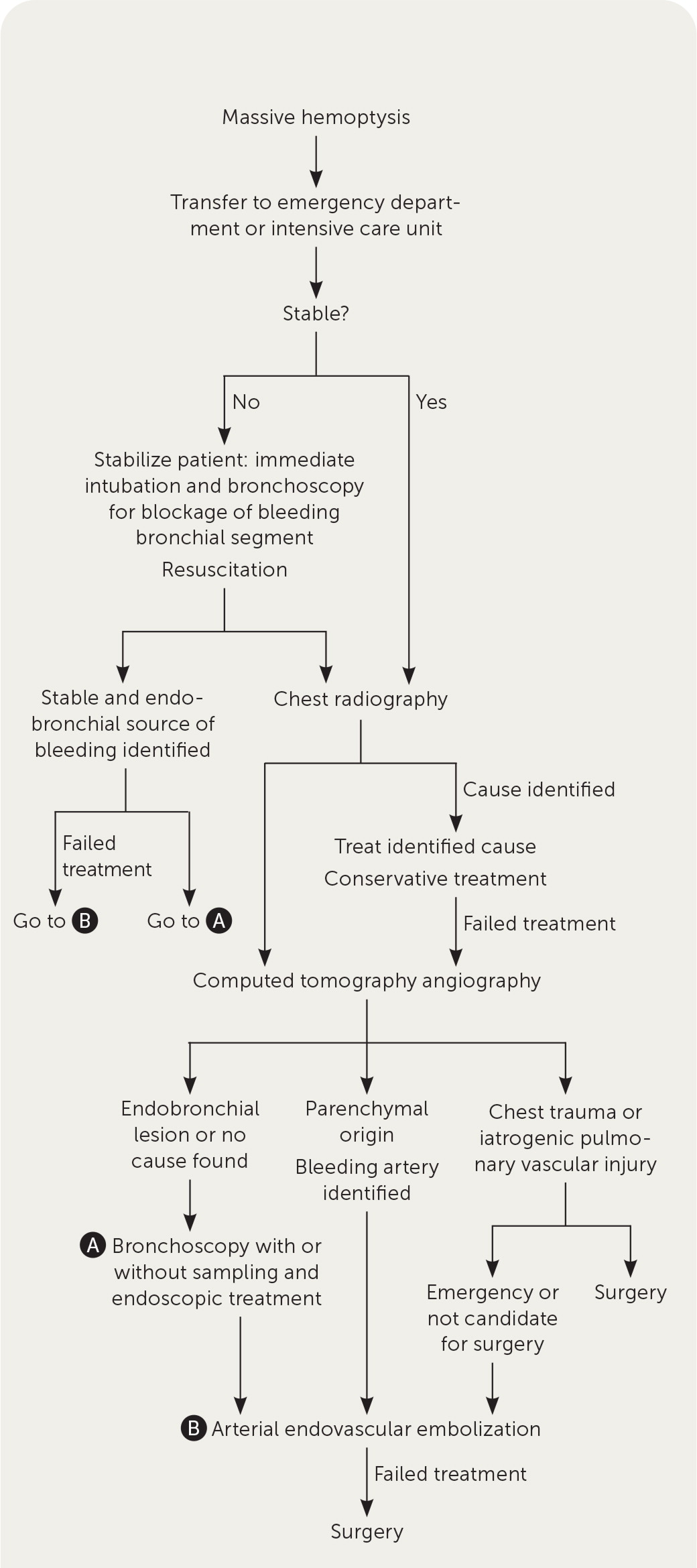
Figure 1 and Figure 2 outline a recommended diagnostic approach to the patient presenting with non-massive and massive hemoptysis, respectively.5,6 Laboratory evaluation for underlying coagulopathy should be obtained and additional laboratory workup should be based on clinical suspicion of other contributors (Table 51,3,6).
| Tests for all patients | Indications |
|---|---|
| Complete blood count | Evaluate for anemia* Leukocytosis can point to infectious or inflammatory cause Rule out thrombocytopenia as cause |
| Complete metabolic panel | Evaluate kidney function before use of imaging with contrast Hepatic abnormalities can cause platelet dysfunction and coagulopathy |
| Prothrombin time/partial thromboplastin time | Determine coagulation status In patients with history of coagulopathy or anticoagulant use |
| Vital signs, including pulse oximetry | Evaluate hemodynamic stability and oxygenation status |
| Tests to consider | |
| Arterial blood gases | To determine impact of hemoptysis on oxygenation and ventilation |
| Blood culture | Concern for infectious cause |
| Blood type and crossmatch | If massive hemoptysis or anemia |
| B-type natriuretic peptide | Concern for congestive heart failure |
| Echocardiography | Concern for cardiac cause, pulmonary hypertension |
| Electrocardiography | Concern for cardiac cause or pulmonary embolism |
| Immunologic antibodies (antineutrophil cytoplasmic antibodies, antinuclear antibodies, double-stranded DNA antibodies, anti–glomerular basement membrane antibody, anticardiolipin) | Concern for immunologic/rheumatologic/vasculitic disease |
| Inflammatory markers | Concern for inflammatory condition |
| Interferon-gamma release assay | Concern for tuberculosis |
| Spirometry | Active hemoptysis is absolute contraindication |
| Sputum cytology | Concern for malignancy |
| Sputum Gram stain/culture, acid-fast bacillus, fungal cultures | Concern for infectious cause |
The American College of Radiology appropriateness criteria for initial imaging for nonmassive hemoptysis include chest radiography, chest CT with intravenous contrast, and chest CT angiography with intravenous contrast.2 Posteroanterior and lateral chest radiography is a good initial test for most cases of hemoptysis because it is readily available, quick, and inexpensive.3,5 Chest radiography may demonstrate pneumonia, cavitary lesions, abscess, masses, or alveolar opacities due to alveolar hemorrhage5,6; however, malignancy may not be found on chest radiography.15 There is evidence on the utility of portable posteroanterior chest radiography often performed in patients who are unstable. Although chest radiography may show if bleeding is focal or diffuse,5 it is less sensitive than CT or CT angiography for determining the site and etiology of the bleeding. Some causes of hemoptysis may not produce changes on chest radiography.16 Therefore, if no cause is found on chest radiography, further evaluation is necessary.3,5
After chest radiography, there is no consensus on whether CT or bronchoscopy should be performed first to determine the etiology of hemoptysis; however, CT has become the preferred modality.2 CT and bronchoscopy have similar effectiveness for identifying the site of bleeding, but CT is more effective for ascertaining the etiology.17,18
Compared with chest radiography, chest CT with intravenous contrast is more sensitive for determining the site and etiology of the bleeding (eTable A). CT angiography with intravenous contrast accurately identifies arteries that may be the source of bleeding and allows for detection of a pulmonary embolism.4,5 Although hemoptysis usually originates from the bronchial arteries, pulmonary and nonbronchial systemic arteries should also be visualized to guide proper embolization.2 Although CT with intravenous contrast and CT angiography with intravenous contrast are similarly effective at diagnosing the site and etiology of the bleeding, CT angiography is more helpful for preprocedural planning if embolization will be performed.2,19,20
| Test | Determines site of bleeding (%) | Identifies etiology of bleeding (%) |
|---|---|---|
| Chest computed tomography | 63 to 100 | 48 to 100 |
| Bronchoscopy | 42 to 93 | 2.5 to 8 |
| Chest radiography (posteroanterior and lateral views) | 35 to 82 | 25 to 35 |
Bronchoscopy can be diagnostic and therapeutic,3,4 and is most helpful for detecting endobronchial lesions.21 Bronchogenic carcinomas are found in 9.6% of patients with hemoptysis and normal chest radiography.15 Bronchoscopy can also evaluate the bronchial mucosa; however, changes are nonspecific.4 Bronchoscopy allows for sampling for tissue pathology and microbial tests.3
When used, rigid bronchoscopy can secure the airway and ventilate the patient; this may be required for massive hemoptysis. Rigid bronchoscopy also allows for the removal of blood or foreign bodies and tumor debulking. However, rigid bronchoscopy is performed in the operating room under general anesthesia and can access only proximal airways unless a flexible scope is inserted to perform a flexible bronchoscopy. Flexible bronchoscopy can be performed at the bedside in the intensive care unit (ICU; with sedation rather than anesthesia), and can access lower airways, but intubation beforehand is needed if airway management is required.3,14
A therapeutic scope also allows for the removal of blood or foreign bodies. To determine the site of bleeding, active bleeding must be visualized. This is more likely to occur during or within 24 to 48 hours of active hemoptysis.4 Bronchoscopy performed in addition to CT may increase sensitivity for the site of bleeding and may also identify etiology of bleeding when none is found on CT.22
Management
The severity of hemoptysis should determine the setting for evaluation and management. Blood-streaked sputum may be managed in an outpatient setting, whereas gross hemoptysis generally should be managed in the emergency department or inpatient setting.4 Outpatient treatment may be considered in patients who are in stable condition, and a suspected cause can be followed up in an outpatient setting, provided the bleeding has stopped. Antitussive medications can assist in controlling coughing, which may trigger continued hemoptysis, and etiology-specific treatment (e.g., antibiotics if an infection is suspected) should be administered, with repeat evaluation in 24 to 48 hours.4
Patients with massive hemoptysis, hemodynamic instability, or airway compromise should be managed in an ICU with access to radiologic, endovascular, bronchoscopic, and surgical care.4,6 eTable B lists other indications for ICU admission. Table 61 shows a model predicting in-hospital mortality that can aid in the decision about ICU admission.23
| Etiology with high risk of bleeding (e.g., aspergillosis, lesions with pulmonary artery involvement) |
| Gas-exchange abnormalities (respiratory rate > 30 breaths per minute, oxygen saturation < 88% in room air, or need for high-flow oxygen [> 8 L per minute] or mechanical ventilation) |
| Hemodynamic instability (hemoglobin < 8 g per dL [80 g per L] or a decrease of more than 2 g per dL [20 g per L] from baseline, consumptive coagulopathy, or hypotension requiring fluid bolus or vasopressors) |
| Massive hemoptysis (> 200 mL per 48 hours or > 50 mL per episode in patients with chronic pulmonary disease) |
| Respiratory comorbidities (e.g., previous pneumonectomy, chronic obstructive pulmonary disease, cystic fibrosis) |
| Other comorbidities (e.g., ischemic heart disease, need for anticoagulation) |
| Chest radiography on admission shows involvement of 2 or more quadrants (1 point) | _________ | |||||||
| Chronic alcoholism (1 point) | _________ | |||||||
| Pulmonary artery involvement (1 point) | _________ | |||||||
| Aspergillosis (2 points) | _________ | |||||||
| Malignancy (2 points) | _________ | |||||||
| Mechanical ventilation required (2 points) | _________ | |||||||
| Score | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Mortality | 1% | 2% | 6% | 16% | 34% | 58% | 79% | 91% |
During active bleeding, patients should be placed on strict bed rest in a lateral decubitus position on the side of the bleeding and allowed nothing by mouth.4,7 Patients should have their vital signs, including oxygenation, monitored closely and intravenous access maintained. If needed, patients should be given supplemental oxygen.4,7 Airway protection, with intubation and bronchial blockage by rigid bronchoscopy, and hemodynamic stabilization are important. Peripheral bleeding, pulmonary isolation by selective bronchial blockage, tamponade, or a balloon catheter prevents blood from the affected area from flowing into other airways.3,4 There are limited data for antifibrinolytics, such as tranexamic acid, but they can be considered in the treatment of severe hemoptysis to reduce bleeding volume and time, and in nonmassive hemoptysis to reduce bleeding volume, further intervention risk, and the length of hospital stay.3,24–27
Surgery has a high mortality risk (2% to 18%), which increases to 25% to 50% during active hemorrhage and emergencies. This is due to a high risk of complications, including perioperative bleeding, asphyxia, bronchopleural fistula, and respiratory failure.3–5,8 Surgery is the treatment of choice only in cases of chest trauma and iatrogenic pulmonary artery rupture.5 Surgery is also performed in patients with hemoptysis refractory to other options or as a definitive treatment after a patient has been stabilized.3
Arterial embolization is the treatment of choice for massive or recurrent hemoptysis (Figure 25,6) and is increasingly being used for nonmassive hemoptysis because it is effective and minimally invasive.2,4,7,8 To prevent a recurrence, all pathologic arteries must be embolized.4 Bronchial arterial embolization is most commonly performed (75%) because bronchial arteries are the most common source of bleeding and most amenable to treatment.8
Prognosis
For mild hemoptysis, recurrences affect 19% of patients (more if medically managed), with 24% occurring in the first three months and 73% in the first two years. Risk factors for recurrence include aspergillosis, nontuberculous mycobacterial infection, smoking, and active bleeding or blood clots on bronchoscopy.7 The mortality rate from mild hemoptysis is 0.3%.7 Moderate and severe hemoptysis, oozing and active bleeding on bronchoscopy, and smoking are associated with higher mortality.30
Embolization symptomatically treats bleeding; therefore, treatment of the underlying disease is often needed to prevent rebleeding.6,8 After bronchial arterial embolization, the rate of rebleeding is high (9.8% to 57.5%), with a median time to recurrence of six months to one year.28,31 Patients who have no recurrence within three years have a good prognosis and are less likely to rebleed, but patients who rebleed tend to have multiple recurrences.31,32 Risk factors for rebleeding after arterial embolization include aspergillomas, tuberculosis, malignancy, greater severity of hemoptysis, and oozing or active bleeding on bronchoscopy.3,6,28,30 Early recurrences are due to incomplete embolization, and later recurrences are due to recanalization of embolized arteries or recruitment of new arteries.28,32 Recurrences are usually treated with repeat embolization, often of nonbronchial systemic or pulmonary arteries, or surgery.2,28,32 Repeat embolizations help manage long-term hemoptysis, but surgery is often needed for definitive treatment after multiple embolizations.28
This article updates previous articles on this topic by Earwood and Thompson1 and Bidwell and Pachner.33
Data Sources: PubMed and OVID were searched using the key terms hemoptysis, nonmassive hemoptysis, mild hemoptysis, severe hemoptysis, computed tomography (CT), bronchoscopy, bronchial artery embolization, prognosis, and mortality from 2010 to 2021. Also searched was the Cochrane database. Search dates: March 2021 and September 2021.
