
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2022;105(2):177-186
Author disclosure: No relevant financial relationships.
Induction of labor is a common obstetric procedure, and approximately one-fourth of pregnant patients undergo the procedure. Although exercise and nipple stimulation can increase the likelihood of spontaneous labor, sexual intercourse may not be effective. Acupuncture has been used for labor induction; however, it has not been shown to increase vaginal delivery rates. There is strong evidence that membrane sweeping can increase the likelihood of spontaneous labor within 48 hours. Cervical preparation or ripening is often needed before induction. Some evidence shows that the use of nonpharmacologic approaches such as osmotic dilators and cervical ripening balloons reduce time to delivery. The effect of amniotomy on labor is uncertain. Pharmacologic intervention with oxytocin or prostaglandins is effective for cervical ripening and induction of labor. Combining a balloon catheter with misoprostol is a common practice and has been shown to decrease time to delivery in a small study.
| Recommendation | Sponsoring organization |
|---|---|
| Do not schedule non–medically indicated (elective) inductions of labor or cesarean deliveries before 39 weeks 0 days gestational age. | American Academy of Family Physicians American College of Obstetricians and Gynecologists |
Indications for Induction
Induction of labor is indicated when the risks of continuing the pregnancy outweigh the risks of induction, with the goal of delivery while minimizing risks to the mother and newborn. Maternal, fetal, and placental conditions can increase the risk of continuing a pregnancy. Common medical indications for induction of labor and recommended timing are covered in Table 1.4 [corrected]
| Indication | Suggested timing (weeks' gestation) | |
|---|---|---|
| Earliest | Before | |
| Maternal | ||
| Chronic hypertension | ||
| No medications | 38 | 40 |
| Well controlled | 37 | 40 |
| Poorly controlled or proteinuria | 36 | 38 |
| Gestational hypertension | 37 | At diagnosis if later than 37 |
| Preeclampsia | ||
| No severe features | 37 | At diagnosis if later than 37 |
| Severe features (immediate if unstable) | 34 | At diagnosis if later than 34 |
| Prepregnancy diabetes mellitus | ||
| Well controlled | 39 | 40 |
| Well controlled but vascular disease | 36 | 39 |
| Poorly controlled | 36 | 39 |
| Gestational diabetes | ||
| Well controlled with diet (A1) | 39 | 41 |
| Well controlled with medication (A2) | 39 | 40 |
| Poorly controlled | Individualized | |
| Cholestasis of pregnancy | 36 | 39 |
| HIV infection (if viral load ≤ 1,000 copies per mL) | 39 | — |
| Fetal | ||
| Fetal growth restriction | ||
| Single gestation, no issues | 38 | 39 |
| Single gestation, other conditions | 34 | 38 |
| Twin gestation, no issues | 36 | 38 |
| Twin gestation, monochorionic or other condition | 32 | 35 |
| Oligohydramnios | 36 | 38 |
| Polyhydramnios | 39 | 41 |
| Alloimmunization | 37 | 39 |
| Multiple gestation | ||
| Dichorionic diamniotic | 38 | 39 |
| Monochorionic diamniotic | 34 | 38 |
| Monochorionic monoamniotic | 32 | 34 |
| Obstetric | ||
| History of stillbirth | Individualized | |
| Late term | 41 | 42 |
| Note: The placental disorders placenta previa, vasa previa, and invasive placental disorders were removed from this table because all typically require cesarean delivery. | ||
Induction of labor before 39 weeks' gestation increases neonatal morbidity and mortality and is not recommended without a medical indication.5,6 Several studies demonstrate that induction of labor at 41 weeks leads to similar outcomes as induction at 42 weeks. Pregnancies that exceed 42 weeks' gestation have increased neonatal morbidity, including convulsions, meconium aspiration, and need for intensive care.7
TIMING OF ELECTIVE INDUCTION
Until recently, elective inductions before 41 weeks' gestation have been controversial because of a lack of evidence. A large randomized trial showed that elective inductions at 39 weeks' gestation or later are associated with improved outcomes in first pregnancies.8 In this trial of low-risk nulliparous women, elective induction at 39 weeks to 39 weeks 4 days had similar neonatal mortality and morbidity as delivery at 40 weeks 5 days or later. Infants from the elective induction group had less need for respiratory support, with a number needed to treat (NNT) of 83 to prevent respiratory support in the first 72 hours of life.
There were also several other improved outcomes with elective induction. Elective induction reduced cesarean delivery (NNT = 28 to prevent one cesarean delivery) and reduced hypertensive pregnancy disorders (NNT = 17).8 The Society for Maternal-Fetal Medicine and the American College of Obstetricians and Gynecologists endorse offering elective induction of labor at 39 weeks' gestation to low-risk nulliparous pregnant individuals under circumstances that are consistent with this trial's study protocol.9,10
INDUCTION OF LABOR AFTER PRIOR CESAREAN DELIVERY
There are several reasons for choosing a trial of labor after a cesarean delivery (TOLAC) instead of a repeat cesarean delivery, including shorter hospital stay, shorter recovery time, and reduced pain after delivery. Careful counseling is required before TOLAC because of risks, including uterine rupture.11,12 A validated calculator is available to assist when deciding on TOLAC vs. a repeat cesarean delivery (https://mfmunetwork.bsc.gwu.edu/web/mfmunetwork/vaginal-birth-after-cesarean-calculator). This calculator was updated to remove the race and ethnicity component, which does not affect the validity.13
For individuals who have had one prior cesarean delivery, TOLAC may reduce rates of cesarean delivery.14–16 In 2019, the American Academy of Family Physicians reaffirmed clinical practice guidelines for management of TOLAC (https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/vaginal-birth-after-cesarean.html). Cervical ripening balloons and oxytocin (Pitocin) are appropriate agents for TOLAC, but prostaglandin use increases the risk of uterine rupture and should be avoided.1,17,18
Assessing Cervical Favorability
BISHOP SCORE
Introduced in 1964, the Bishop score (Table 219–21) is the most widely used method for determining cervical favorability. The Bishop score grades the dilation, effacement, position, and consistency of the cervix and the fetal station in the maternal pelvis, producing a score from 0 to 13. It is available as an online calculator at https://www.mdcalc.com/bishop-score-vaginal-delivery-induction-labor.
| Cervical examination findings | Score |
|---|---|
| Simplified score | |
| Dilation | |
| Closed | 0 |
| 1 to 2 cm | 1 |
| 3 to 4 cm | 2 |
| ≥ 5 cm | 3 |
| Effacement | |
| 0% to 30% | 0 |
| 40% to 50% | 1 |
| 60% to 70% | 2 |
| ≥ 80% | 3 |
| Fetal station | |
| −3 | 0 |
| −2 | 1 |
| −1, 0 | 2 |
| +1, +2 | 3 |
| For a full score add: | |
| Position | |
| Posterior | 0 |
| Middle | 1 |
| Anterior | 2 |
| Consistency | |
| Firm | 0 |
| Medium | 1 |
| Soft | 2 |
| Total: | ______ |
The cervix is considered unfavorable if the Bishop score is 5 or less. With a Bishop score greater than 8, the probability of a successful vaginal delivery with induction is the same as for spontaneous labor. A simplified Bishop score that uses only dilation, effacement, and position has the same accuracy as the full score for predicting successful induction. A simplified Bishop score greater than 5 predicts a successful vaginal delivery with induction.20–23
TRANSVAGINAL ULTRASONOGRAPHY
Cervical length assessment using transvaginal ultrasonography has been used to predict the need for cervical ripening. In two small randomized trials, using a cervical length greater than 28 mm as criteria for cervical ripening led to less prostaglandin use with similar vaginal delivery rates and time to delivery.24–26
Inducing Spontaneous Labor Before Admission
EXERCISE
Exercise may increase spontaneous labor at term. In a small randomized controlled trial, women with low-risk pregnancies at 38 weeks who exercised required less induction and fewer operative vaginal deliveries.27 Women in the exercise group walked for 30 minutes a day at a moderate rate three times a week. Exercise is a safe method of enhancing the onset of spontaneous labor.
BREAST STIMULATION
Breast massage and nipple stimulation can be used as a natural method of labor induction. Nipple stimulation causes release of oxytocin from the posterior pituitary gland, leading to uterine contractions and cervical ripening. In a small randomized controlled trial, bilateral breast massage for 15 to 20 minutes three times daily starting at 38 weeks' gestation increased the chance of vaginal delivery, with an NNT of 8.28
SEXUAL INTERCOURSE
Sexual intercourse theoretically encourages labor through the release of oxytocin from breast stimulation and cervical exposure to prostaglandins in semen. Yet a systematic review showed no increase in the rate of spontaneous labor after intercourse. There is no reason to restrict sexual intercourse in low-risk pregnancies.29
ACUPUNCTURE
Acupuncture does not increase vaginal delivery rates based on a Cochrane review.30
CASTOR OIL
Castor oil also does not appear to increase rates of spontaneous labor. A Cochrane review of three small trials showed no benefit from one dose of the cathartic agent.31
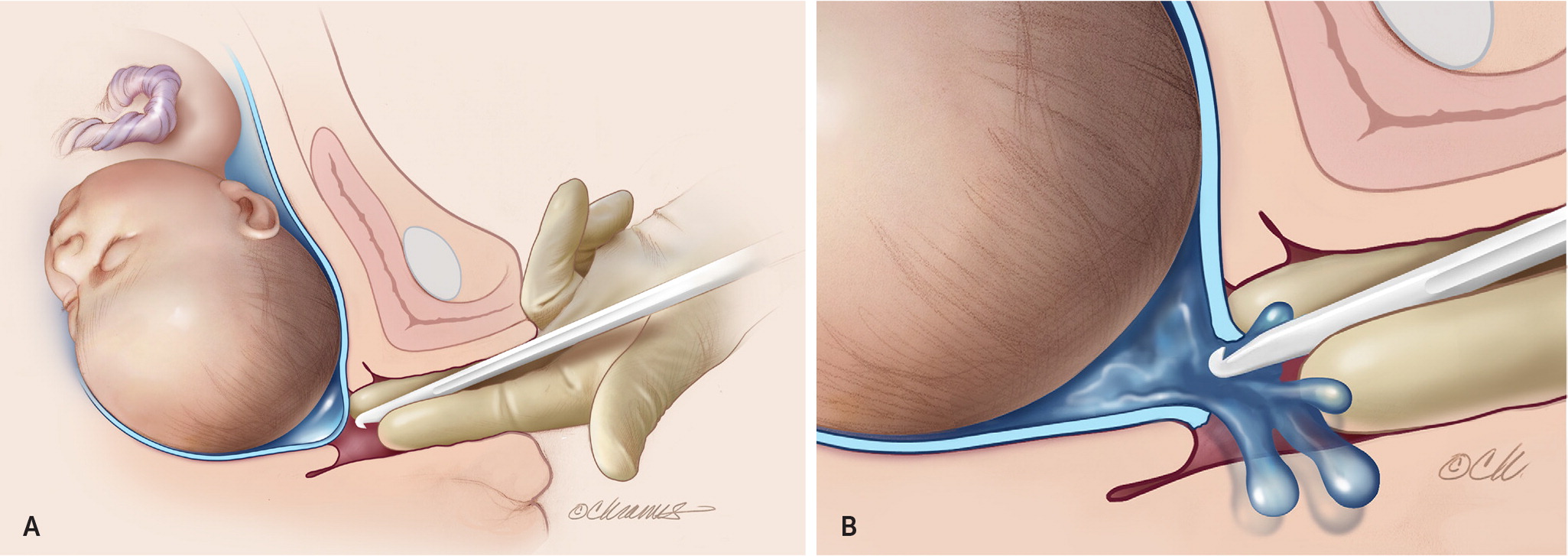
MEMBRANE SWEEPING
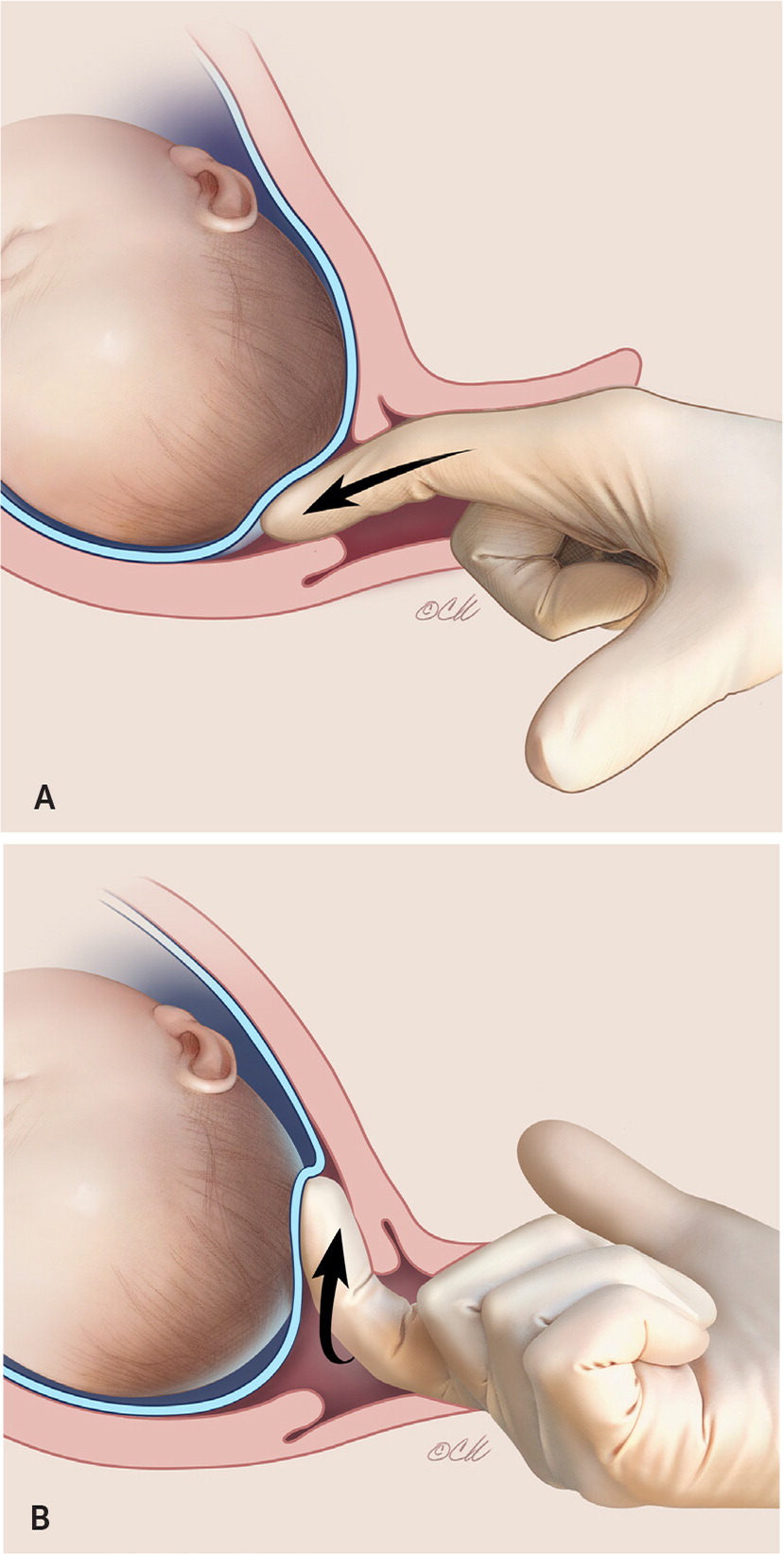
Stripping the amniotic membranes, also called membrane sweeping, is common in the outpatient setting. Membrane sweeping involves shifting the internal cervical os in relation to the amniotic membranes during a cervical examination, as described in Table 332 and illustrated in Figure 1. This promotes local release of prostaglandins, phospholipase A1, and cytokines, which ripen the cervix and induce uterine contractions. Membrane sweeping reduces the need for induction. In a Cochrane review of 40 studies, membrane sweeping increased spontaneous labor within 48 hours, with an NNT of 8.32
| Ensure good dating, and confirm pregnancy is term. |
| Inform the patient of risks, including discomfort, rupture of membranes, irregular contractions, and vaginal bleeding. |
| Confirm location of placenta with ultrasonography to rule out placenta previa. |
| Perform sterile vaginal examination, and place a finger through the internal os of the cervical canal. |
| With the finger inside the internal os, use a circular motion to disrupt the connection of the amniotic sac and endometrial lining (Figure 1). |
Membrane sweeping in carriers of group B streptococci appears to be safe. In one study, membrane sweeping led to similar neonatal outcomes in patients positive or negative for group B streptoccoci.33
Cervical Ripening
| Method | Dose | Adverse effects | Advantages | Disadvantages | Uses | Precautions |
|---|---|---|---|---|---|---|
| Balloon catheter: single balloon (Foley catheter) or double balloon | — | — | Can be considered for outpatient cervical ripening Cost-effective | Discomfort with insertion | Useful for minimally dilated cervix and if fetus is not tolerant of other cervical ripening methods Combination of Foley catheter and misoprostol was more effective than single-agent cervical ripening in a small randomized controlled trial34 | Mucopurulent cervicitis, rupture of membranes |
| Hygroscopic dilators: Dilapan-S rods, laminaria35,36 | Usually 3 to 5 for Dilapan-S and 1 to 2 for laminaria | Bleeding, infection | Can be considered for outpatient cervical ripening Tolerable, easy to use, cost-effective Fetal monitoring not needed during ripening process | — | Ripening for closed cervix | Presence of genital tract infection |
| Dinoprostone37,38 | 0.5-mg gel 10-mg vaginal insert | Nausea/upset stomach, vomiting, diarrhea, flushing, pyrexia | Insert easily removed to reverse effects | Increased time from placement to delivery Expensive ($450 per insert, estimated lowest GoodRx price [no generic available]) | Ripening for closed cervix | Presence of genital tract infection Uterine scar |
| Misoprostol (Cytotec, prostaglandin1 analogue)38–41 | 25 mcg intravaginally 50 mcg orally (sublingual or buccal) | Pyrexia, abdominal pain, shivering, nausea, diarrhea | Inexpensive (50 cents per 100-mcg tablet, estimated lowest GoodRx price for generic) | Uterine tachysystole more common Inability to reverse effects if there are abnormal changes | Ripening for closed cervix Use in combination with cervical ripening balloon increases likelihood of vaginal delivery within 24 hours34,35 | Uterine scar |
| Oxytocin (Pitocin) | 10 units in 1,000 mL of normal saline 1 to 2 mU per minute, titrated to establish contraction pattern Low-dose regimen: start at 0.5 to 2 mU per minute, and increase by 1 to 2 mU per minute every 15 to 40 minutes to a maximum of 32 mU per minute High-dose regimen: start at 6 mU per minute, and increase by 3 to 6 mU per minute every 15 to 40 minutes to a maximum of 40 mU per minute1,42,43 | Nausea, vomiting, water intoxication in high doses | Because of its short half-life, oxytocin can be titrated to desired effect and discontinued as needed if there are abnormal fetal heart rate changes Can be used for cervical ripening in trial of labor after cesarean delivery | Longer time from induction to vaginal delivery compared with other methods | Cervical ripening, especially in patients with prior cesarean delivery or uterine surgery Induction/augmentation after cervical ripening | — |
MECHANICAL METHODS
Mechanical modalities, including balloon catheters and osmotic dilators, physically dilate the cervix and cause secondary release of prostaglandins and oxytocin.
Cervical Balloon Catheters. Single-balloon Foley catheters have long been used for cervical ripening, whereas double-balloon catheters became available more recently. Both single- and double-balloon catheters are placed through the cervix to the intrauterine cavity. The catheters are most often placed digitally but can be inserted using a speculum and ringed forceps if the cervix is minimally dilated. After placement, the balloons are inflated to provide outward mechanical pressure on the cervix to promote dilatation. The catheters are removed after 12 hours if they do not fall out earlier. Table 5 describes cervical balloon catheter placement.44
| Catheters can be placed digitally during vaginal examination or by using a speculum to directly visualize the cervix. |
| Double-balloon catheters can be placed with or without the use of a stylet. |
| Insert the tip of the catheter into the cervical canal using gentle pressure. |
| The catheter must traverse the cervical canal to the uterine cavity. |
| Advance the catheter until the balloon(s) are in the cervical canal. |
| For a single-balloon Foley catheter, inflate the balloon with 30 mL of saline. Consider using a 500-mL saline bag to apply constant tension to the catheter, which speeds cervical dilation. |
| For a double-balloon catheter: Inflate the uterine balloon with 40 mL of saline. Once inflated, pull the catheter back until the uterine balloon contacts the internal os. The vaginal balloon should be visible or palpable outside the external os. Inflate with 20 mL of saline after removing the speculum, if used. Once the balloons are placed, inflate with saline to a maximum of 80 mL for each balloon. No traction is necessary for a double-balloon catheter. |
Outpatient cervical preparation using a transcervical Foley catheter placed in the clinic is sometimes performed in low-risk patients. In one randomized controlled trial of parous women, outpatient catheter placement did not shorten time from admission to delivery compared with inpatient catheter placement and oxytocin.45 But in another trial of only nulliparous women, outpatient catheter placement reduced the time from admission to delivery by four hours.46,47
Osmotic Dilators. Osmotic dilators are placed into the cervical canal and increase in diameter by absorbing fluids, gradually dilating the cervix. Two available dilators are Dilapan-S, a synthetic hygroscopic dilator, and laminaria, a natural product made from kelp (Laminaria japonica or Laminaria digitata). Both osmotic dilators are placed in the cervical canal for an extended time and then removed, allowing them to be used for outpatient and hospitalized patients. Dilapan-S dilators are typically removed after 12 hours, whereas laminaria is usually removed within 12 to 24 hours. The placement procedure is summarized in Table 6.48
| Cervical dilators can be placed in outpatient and hospital settings. |
| Perform continuous fetal monitoring for 20 minutes before insertion. |
| Use a sterile speculum to visualize the cervix. |
| Disinfect the cervix with an appropriate cleansing solution (e.g., iodine). |
| Use a tenaculum or ring forceps to stabilize and straighten the cervical canal. |
| Moisten the dilator with sterile saline. |
| Place the dilator rods into the endocervix using ring forceps, allowing the tails to fall into the vagina. |
| Continue to place dilators until the cervical canal is filled. |
| This usually requires 3 to 5 synthetic dilators and 1 to 2 laminaria dilators. |
| Note the number of dilators in the medical record. |
| Place a sterile gauze pad into the vagina to maintain the dilator position. |
| Remove synthetic dilators within 12 hours and laminaria dilators within 12 to 24 hours. |
A randomized controlled trial of patients with a term pregnancy and an unfavorable cervix found that the hygroscopic cervical dilator was similar to the Foley catheter for time to delivery and successful vaginal delivery. Patient satisfaction was higher for the dilator, which increased sleep, relaxation, and daily activities.36
PHARMACOLOGIC METHODS (PROSTAGLANDINS)
Synthetic prostaglandins are effective for cervical ripening. Two synthetic analogues are available—misoprostol (Cytotec), a prostaglandin E1 analogue, and dinoprostone, a prostaglandin E2 analogue. Prostaglandins increase contractions and can lead to tachysystole, defined as an average of five contractions or more in 10 minutes. After administering a prostaglandin, uterine activity and fetal heart rate should be monitored for 30 minutes to two hours.1 To avoid tachysystole, prostaglandins should not be used if more than three contractions occur in 10 minutes. In individuals with a prior cesarean delivery, prostaglandin use increases the risk of uterine rupture and is not recommended by the American College of Obstetricians and Gynecologists.18
Dinoprostone is available as a 0.5-mg gel and a 10-mg vaginal insert. Although both are effective, a small trial suggests that the vaginal insert is more likely to result in spontaneous labor.37
Misoprostol is used for cervical ripening and labor induction and can be administered vaginally, sublingually, or buccally. Misoprostol is available in unscored 100-mcg tablets, which are broken into quarters for administration in 25-mcg increments.1 Although 50 mcg given intravaginally is also an option, 25 mcg of intravaginal misoprostol results in a lower risk of tachysystole, fetal heart rate abnormalities, and need for neonatal intensive care, and is the usual starting dose.39
Induction with a Favorable Cervix
AMNIOTOMY
| Monitor the fetus throughout the procedure. |
| Perform a sterile vaginal examination to evaluate the cervix and fetal station. |
| The fetal head should be well applied to the cervix. |
| Insert the amniotomy hook through the cervical os by sliding it along the hand and fingers, with the hook toward the hand. |
| Rotate the hook to puncture the amniotic membranes. |
| Keep fingers inside the vagina while amniotic fluid drains to ensure no cord is present (Figure 2). |
| Note the color and consistency of the fluid after rupture (clear, bloody, meconium-stained, thin or thick). |
The effect of amniotomy on progression of labor is uncertain. Amniotomy performed before active labor does not increase spontaneous labor according to a Cochrane review.49 Yet a more recent systematic review showed a shorter interval from induction to delivery when amniotomy was performed before active labor.50
OXYTOCIN
Oxytocin is a natural hormone that can be given intravenously for induction and augmentation of labor and is commonly used as part of the active management of the third stage of labor to prevent postpartum hemorrhage. Oxytocin increases calcium release to contract the uterine muscle.51 Although oxytocin infusion may reduce oxytocin receptor sensitivity after delivery, the impacts of oxytocin use on postpartum hemorrhage and the active management of the third stage of labor are unclear. Oxytocin can cause tachysystole similar to prostaglandins, but contractions decrease rapidly after reducing the dose. The American College of Obstetricians and Gynecologists recommends continuous monitoring of uterine contractions and fetal heart rate when using oxytocin for induction or augmentation of labor.52
The success rate of oxytocin depends on many factors. When oxytocin is used, the likelihood of vaginal birth is higher with greater cervical dilation, lower body mass index, and higher parity. As gestational age increases, the effectiveness of oxytocin increases, likely due to increased uterine oxytocin sensitivity. Induction with oxytocin alone results in fewer vaginal deliveries within 24 hours than initial cervical ripening with prostaglandins followed by oxytocin.53
Two oxytocin dosing strategies are commonly used. The low-dose protocol starts at 0.5 to 2 mU per minute and increases by 1 to 2 mU per minute every 15 to 40 minutes, and the high-dose protocol starts at 6 mU per minute and increases by 3 to 6 mU per minute every 15 to 40 minutes.1 Although the higher-dose protocol has a higher rate of tachysystole, the lower-dose protocol may have a higher rate of postpartum hemorrhage.1,40 There is no difference between the high- and low-dose protocols in time to delivery, assisted deliveries, and cesarean delivery rate.40,41,53
Combining Induction Methods
This article updates previous articles on this topic by Tenore54 and Harman and Kim.55
Data Sources: Policy statements were reviewed from the American College of Obstetricians and Gynecologists. PubMed, Google Scholar, and the Cochrane database were searched using the key words labor induction, cervical ripening, Bishop score, Foley catheter for cervical ripening, mechanical methods of cervical ripening, misoprostol, oxytocin, prostaglandin E2, transcervical Foley balloon, preinduction cervical ripening, and outpatient cervical ripening. Search dates: September 18, 2020, to December 14, 2020.
The opinions and assertions contained herein are those of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department, the Army at large, the Uniformed Services University of the Health Sciences, or the Department of Defense.
