
Am Fam Physician. 2022;105(4):356-357
Author disclosure: No relevant financial relationships.
The COVID-19 pandemic has underscored the need for a more effective and equitable health care system in the United States. County-level variations in COVID-19 positivity rates, hospitalizations, and number of deaths demonstrate that community-level factors are essential to the pandemic response.1 Greater access to primary care has historically resulted in better health outcomes.2 Public health measures, such as masking and vaccination, and social assets, including access to housing for quarantine periods and transportation for treatment, are also important determinants of COVID-19 outcomes.
Our goal was to examine the cumulative effects of robust primary care, public health preparedness, and social assets on COVID-19 outcomes at the county level using a novel index called the Community Health Index (CHI). The CHI is an average score of public health preparedness, primary care physician supply rates, and the social deprivation index (a proxy for community-level factors such as housing and transportation). The National Health Security Preparedness Index was used to derive a public health preparedness score, the American Medical Association Physician Masterfile was used to provide the primary care physician supply rates, and the American Communities Survey was used to calculate a social deprivation index.3
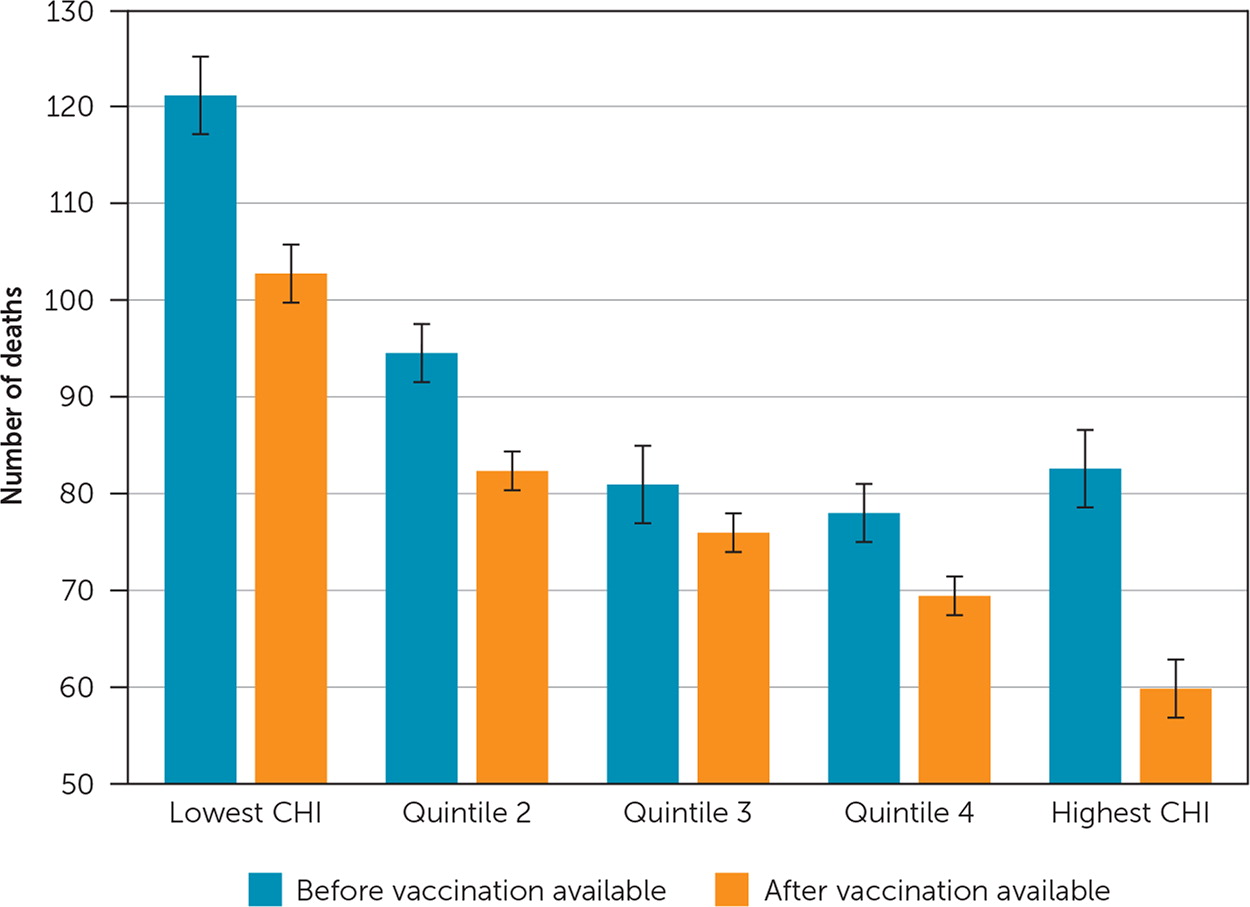
Each component of the CHI can have a score between 1 (lowest) and 10 (highest) for a total CHI score that ranges from 3 (lowest total score) to 30 (highest total score). In this analysis, counties were divided into quintiles based on their CHI, with Quintile 1 representing the lowest scoring counties (mean score = 8.6) and Quintile 5 representing the highest scoring counties (mean score = 26.7). These scores were then compared with county-level COVID-19 death rates before and after vaccination was available to all adults in the United States. Detailed methodology, including dates of data acquisition, is available elsewhere.4
Results demonstrate that before and after vaccination, COVID-19 deaths per 100,000 individuals were lower in counties with higher CHI scores. Specifically, counties in the top quintile had 42% lower death rates than counties in the lowest quintile. Furthermore, although deaths related to COVID-19 fell after vaccination availability regardless of CHI, the number of deaths fell most drastically for counties in the highest quintile (Figure 1).
These data demonstrate that the three components of the CHI (primary care, public health, social assets) had a cumulative effect on preventing deaths from COVID-19. Although this analysis does not account for the benefits of integrating these sectors, data emerging from states such as Maryland demonstrate improved COVID-19 outcomes in areas where public health and primary care are well-integrated.5 Strong public health, robust primary care, and social assets contributed to the COVID-19 response. Working in combination, these three resources have the potential to lead to exponentially better success in combatting future surges of COVID-19 or another health pandemic.
