
Am Fam Physician. 2022;105(4):369-376
Author disclosure: No relevant financial relationships.
Familiarity with common oral conditions allows clinicians to observe and treat patients in the primary care setting or refer to a dentist, oral surgeon, otolaryngologist, or other specialist. Recurrent aphthous stomatitis (canker sores) is the most common ulcerative condition of the oral cavity. Recurrent herpes simplex labialis and stomatitis also commonly cause oral ulcers. Corticosteroids, immunocompromise, antibiotics, and dentures can predispose patients to oral candidiasis. Benign migratory glossitis (geographic tongue) occurs in up to 3% of the population but generally lacks symptoms, although some people experience food sensitivity or a burning sensation. Hairy tongue is associated with a low fiber diet, tobacco and alcohol use, and poor oral hygiene in older male patients. Generally, hairy tongue is asymptomatic except for an unattractive appearance or halitosis. Tobacco and alcohol use can cause mucosal changes resulting in leukoplakia and erythroplakia. These can represent precancerous changes and increase the risk of squamous cell carcinoma. Mandibular and maxillary tori are common bony cortical outgrowths that require no treatment in the absence of repeat trauma from chewing or interference with dentures. Oral lichen planus occurs in up to 2% of individuals and can present as lacy reticulations or oral erosions and ulcerations. Traumatic buccal mucosal fibromas and labial mucoceles from biting can be excised.
Patients with oral disease may present to their family physician before a dentist. Some lesions are purely localized to the mouth, and others have systemic manifestations; familiarity with these entities is important for providing comprehensive primary care. This article describes the etiology, presentation, and management of commonly encountered oral conditions.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Aphthous stomatitis may be treated with topical or, less commonly, intralesional corticosteroids.2–4 | C | Good clinical studies are lacking; Cochrane reviews indicate insufficient evidence to support any specific therapy |
| Oral antiviral therapies started at the onset of symptoms can modestly decrease pain and healing time in recurrent herpes labialis.14–17 | A | Consistent findings from randomized controlled trials |
| Oral leukoplakia, erythroplakia, and erythroleukoplakia should be biopsied to identify oral epithelial dysplasia or malignancy.18–21 | C | Known rates of malignant transformation of these conditions |
| Symptomatic oral lichen planus can be treated with topical and systemic corticosteroids and calcineurin inhibitors.25–27,29 | B | Systematic reviews and meta-analyses |
Aphthous Stomatitis
Recurrent aphthous stomatitis, or canker sores, is the most common ulcerative condition of the oral cavity 1–3 (Figure 1). Prevalence in the general population has been reported at 20%, peaking between 10 and 20 years of age and decreasing after 50 years of age.1–4 A positive family history is found in 40% of patients suggesting a genetic predilection.2,4 The etiology is unknown.1,4
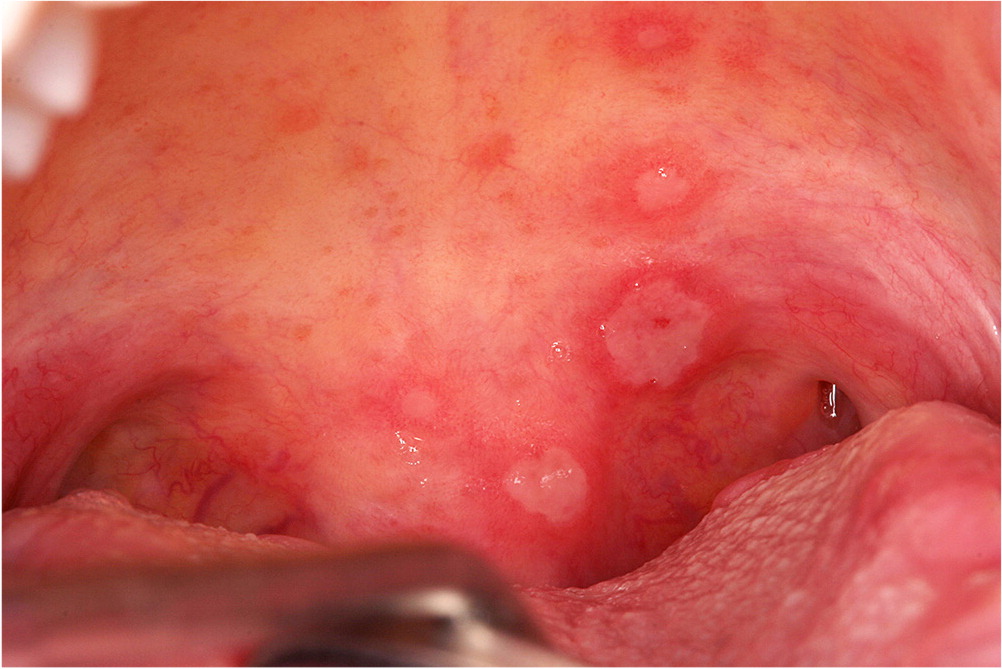
Minor aphthae comprise 75% to 85% of cases with lesions less than 1 cm in diameter that persist for seven to 14 days and heal without scarring. These present on mucosa that is not attached to a bony structure of the hard palate or gums.1,4 Major aphthae (e.g., Sutton disease) represent 5% to 10% of cases and are characterized by painful ulcers larger than 1 cm that may persist up to six weeks and often leave mucosal scarring. Major aphthae can occur at any oral site and in the oropharynx.1,2,4 Major aphthae are associated with HIV infection. The herpetiform type accounts for 5% to 10% of recurrent aphthous stomatitis; they occur in patches of up to 100 aphthae anywhere in the oral cavity, ranging in size from 0.1 to 0.3 cm. These heal within two weeks and appear similar to herpetic stomatitis.1,2
Treatment goals include reducing lesion frequency, pain, and size. Application of topical corticosteroid gels or rinses is the primary therapy; however, quality studies lack support for any specific treatment.2,4 Systemic corticosteroids or intralesional triamcinolone may be used for more severe presentations.1–3 Oral chlorhexidine (Peridex) rinse may decrease lesion severity and pain, but prolonged use stains the teeth.3 Patients should avoid foods that trigger ulcers. Sodium lauryl sulfate (a common ingredient in many types of toothpaste) may increase the irritation and pain from aphthous ulcers.1
Candidiasis
Approximately 30% to 60% of healthy individuals have oral Candida colonization, most commonly with C. albicans.5–7 Opportunistic infection can occur secondary to oral or inhaled corticosteroid use, immunocompromise, diabetes mellitus, malnourishment, antibiotics, and denture use.5–7 Oral candidiasis can present with white plaques that can be wiped off to reveal underlying erythematous mucosa (pseudomembranous candidiasis; Figure 2), generalized mucosal erythema (atrophic candidiasis), less commonly as hyperplastic nonwipeable plaques with a predilection for the lateral tongue and oral commissure (hyperplastic candidiasis), or depapillation and erythema of the dorsal tongue (median rhomboid glossitis).5–7 Patients may report oral burning, a metallic taste, or no symptoms.6

Denture stomatitis, a limited form of atrophic candidiasis, may be associated with dental prosthesis use attributed to restriction of salivary contact with its antimicrobial benefits. Removing oral appliances overnight and soaking in 0.1% sodium hypochlorite or 4% chlorhexidine (to avoid metal tarnishing) addresses appliance colonization.5 Brushing dentures with toothpaste should be avoided because this can cause surface scratching. An important differential diagnosis for hyperplastic candidiasis is leukoplakia, and if lesions do not completely resolve with antifungal therapy, then a biopsy is indicated.6,7 Accumulation of saliva in skin folds at the external corners of the mouth with Candida and Staphylococcus aureus infection can cause angular cheilitis (i.e., perleche) with pain and fissuring.5–7
Geographic Tongue
Geographic tongue (i.e., benign migratory glossitis, erythema migrans) occurs in up to 3% of the population and presents with depapillated, erythematous areas with serpiginous white borders forming a map-like appearance that migrates over time8–10 (Figure 3). Benign migratory glossitis has a familial predisposition and may be associated with psoriasis but otherwise lacks an evident cause.8–10 Most patients are asymptomatic, but some experience lingual burning and food sensitivity, which can be treated with topical rinses with anesthetic, antihistamines, sucralfate (Carafate), or, in severe cases, corticosteroids or calcineurin inhibitors, although comparative studies are lacking.9–11

Hairy Tongue
Retention hyperkeratosis of the filiform papillae on the anterior two-thirds of the lingual dorsum causes a furry appearance with hair-like projections that can be colonized with bacteria and take on dark pigmentation (i.e., black hairy tongue; Figure 4). This condition occurs in 0.5% to 11% of the population, commonly in older individuals, and has a 3:1 predilection for males.12,13 Associated factors include tobacco use, alcohol use, poor oral hygiene, a low fiber diet, hyposalivation, mouth-breathing, and immunosuppression.8,12,13 Hairy tongue can cause halitosis and concerns with visual appearance, but otherwise generally lacks symptoms. Hairy tongue responds well to increasing dietary fiber and brushing the lingual dorsum (with standard toothpaste or 1.5% hydrogen peroxide) or scraping the tongue.8,12,13

Herpetic Stomatitis
Herpes simplex viruses 1 and 2 (HSV-1, HSV-2) cause herpes labialis (cold sores; Figure 5A) and herpetic gingivostomatitis. HSV-1 has a 60% to 95% worldwide prevalence in adults and is normally acquired by adolescence.14,15 HSV-1 has classically been identified as the cause of oral lesions, whereas HSV-2 was associated with genital lesions; however, more data indicate substantial overlap.16 The initial (primary) infection with oral HSV can be markedly symptomatic with numerous vesicles throughout the mouth and may be accompanied by fever, malaise, lymphadenopathy, and pain that can interfere with speech and eating.16
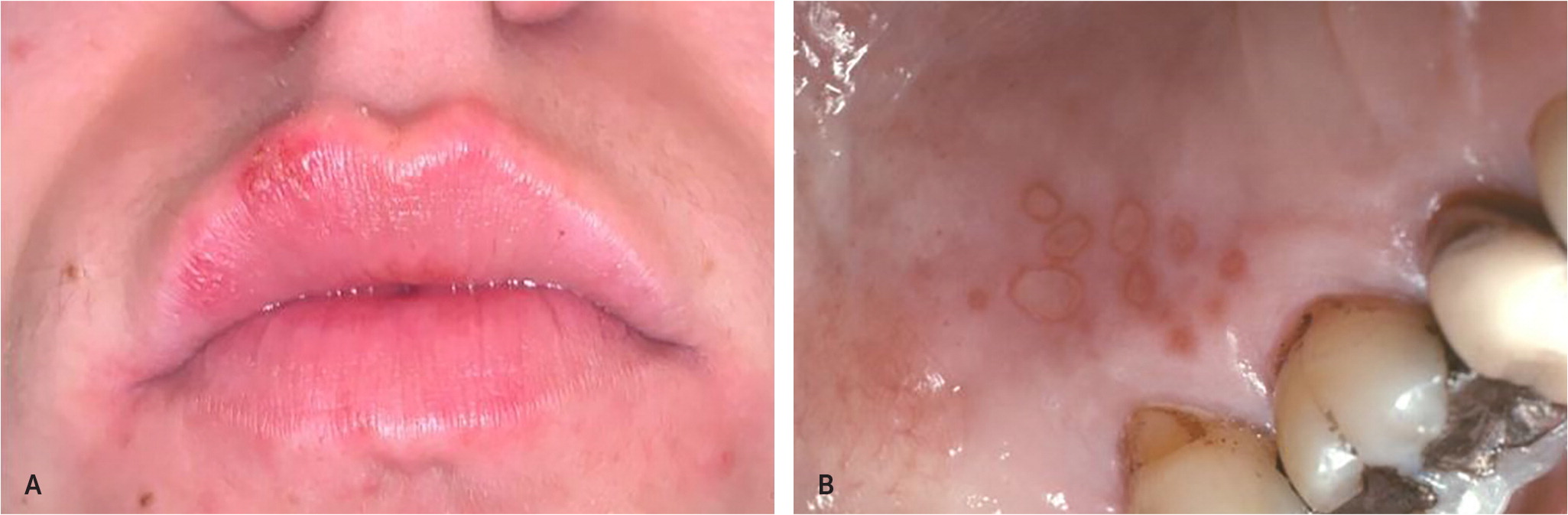
After initial exposure, HSV is dormant in the trigeminal ganglia and can cause episodic, recurrent outbreaks; stress, fatigue, illness, sunlight, and menses can reactivate HSV.16,17 The most common site of herpetic recurrence is the lips, but HSV may also occur at adjacent nasal structures. Up to 40% of infected individuals may develop recurrent herpes labialis.16 A prodrome of itching, burning, pain, or tingling precedes recurrence in 60% of patients. Blistering follows within 24 hours, becoming crusted, painful ulcerations that may bleed.14,17 Topical 5% acyclovir cream or topical penciclovir 1% cream (Denavir) applied every two hours at prodrome onset and used for five days decreases pain.16 Over-the-counter 10% docosanol cream (Abreva) has a similar benefit.14 Oral antivirals decrease pain and duration but must be started within 24 hours of onset. For initial infection, acyclovir in a dosage of 200 mg five times per day for 10 days is one option; valacyclovir (Valtrex), 1 g two times per day for 10 days, is an easier dosage regimen for patients. Recurrent herpes labialis is treated with valacyclovir, 2 g at prodrome and then 2 g 12 hours later.16 Most individuals have two or fewer flareups of recurrent herpes labialis per year, but 5% to 10% experience six or more and may benefit from prophylactic valacyclovir, 500 mg two times per day.15–17 Studies involving exposure to experimental ultraviolet light suggest that wearing sunscreen may prevent outbreaks; however, more research is needed for actual sun exposure.17 The relatively uncommon recurrent intraoral herpes occurs on mucosa of the hard palate, lacks a prodrome, and may be asymptomatic16 (Figure 5B).
Leukoplakia and Erythroplakia
Oral leukoplakia is an asymptomatic and often well-demarcated white plaque that cannot be wiped away or characterized clinically or pathologically as any other disease18 (Figures 6A, 6B, and 6C). Leukoplakia occurs in 1% to 4% of individuals and is most commonly found in older men between 40 and 70 years of age.18,19 Individuals who smoke have a sixfold greater incidence; alcohol use is also an independent risk factor.18 Erythroplakia is much less common and manifests as a smooth or pebbly, well-defined red patch, whereas erythroleukoplakia has red and white components (Figure 6D). Leukoplakia has a variably reported incidence of oral epithelial dysplasia, carcinoma in situ, and squamous cell carcinoma of 10% to 46%, which varies based on the clinical definition. In contrast, almost all cases of erythroplakia show dysplasia, with 90% exhibiting severe dysplasia, carcinoma in situ, or invasive squamous cell carcinoma.18,19
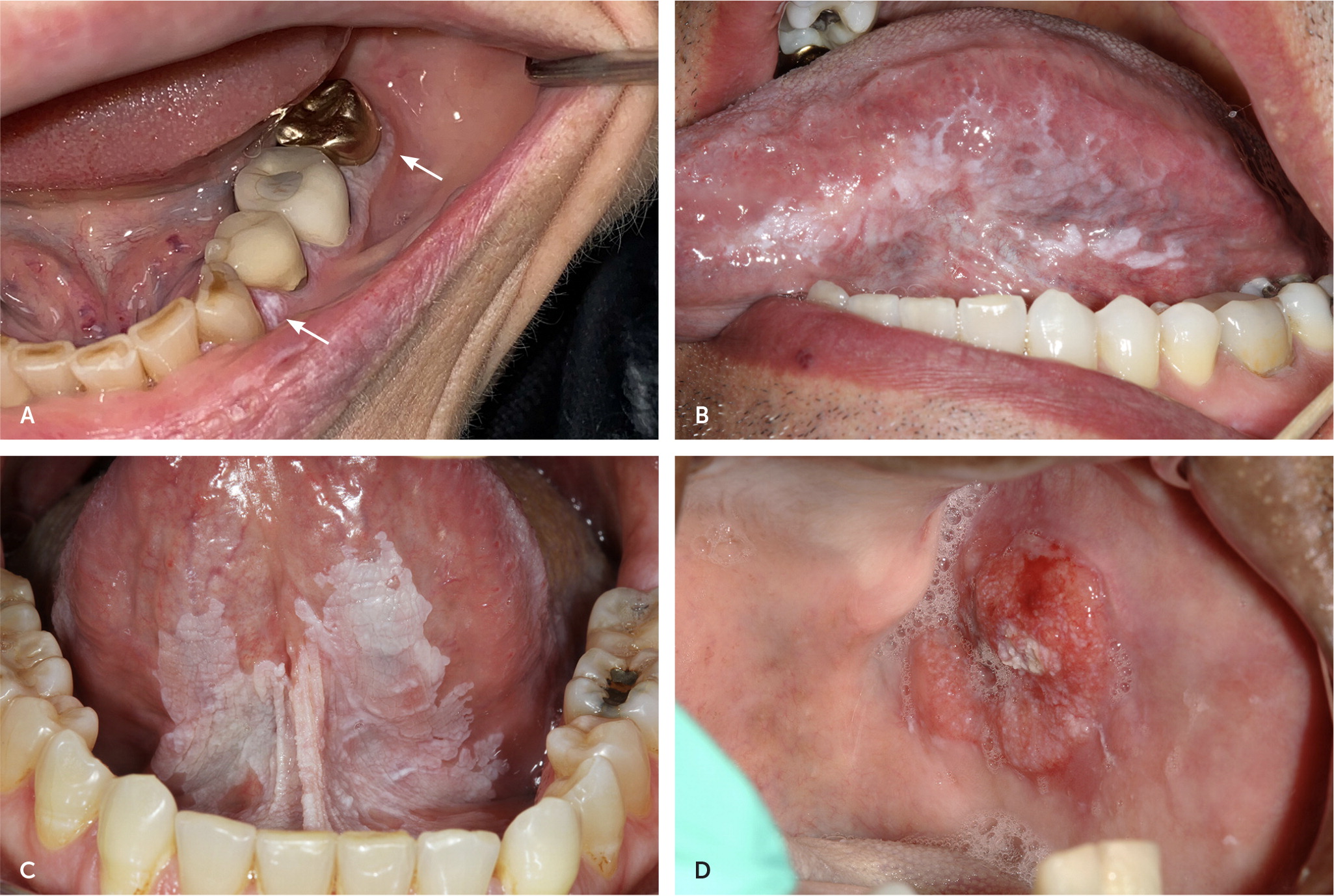
A biopsy should be performed to identify premalignant or malignant change, with excision for significant dysplasia or carcinoma; however, it is reasonable to defer biopsy for two weeks to determine if the lesions resolve spontaneously.18–21 In the absence of oral epithelial dysplasia, evaluation at least twice annually has been suggested because of the potential for malignant transformation.21
Maxillary and Mandibular Tori
Torus palatinus (Figure 7A) and torus mandibularis (Figure 7B) develop, respectively, as cortical outgrowths from the midline palate and inner surface of the mandible and occur in up to 10% to 30% of individuals.22,23 They have a hereditary component, present around puberty, and grow during adulthood.22,23 Tori rarely cause symptoms except when interfering with a comfortable fit of an oral appliance or recurrent ulceration caused by mastication trauma from hard foods. Indications for removal are chronic trauma, difficulty fitting dentures, or harvesting bone graft material for dental surgery.24
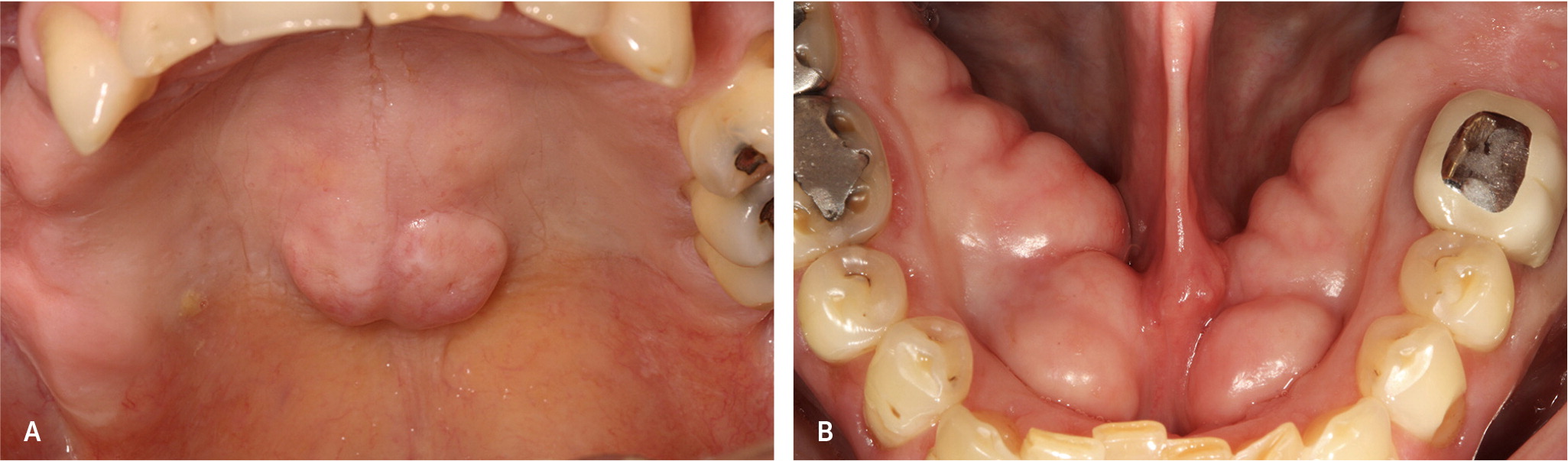
Mucocele
Mucoceles often result from trauma, usually biting, that leads to mucus extravasation into the adjacent connective tissues. They appear most commonly on the lower lip mucosa as smooth, blue-pink masses22,23 (Figure 8). Their typical location adjacent to the teeth often results in a cycle of biting, rupture, and recurrence. Small mucoceles usually resolve spontaneously. For recurrent or persistent lesions, treatment involves excision of the mass and its associated minor salivary gland.22

Oral Lichen Planus
Oral lichen planus is found in up to 2% of individuals and affects mucosa throughout the oral cavity 25–27 (Figure 9). Persons infected with hepatitis C virus have up to a sixfold higher incidence of lichen planus; oral lichen planus may be the initial manifestation.25 Approximately one-half of individuals with cutaneous lichen planus also have intraoral lesions.28 Reticular (the most common), erythematous, and erosive types have been described. A T-cell immune response has been postulated, but the exact etiology is uncertain.27 Women have a 2:1 predilection compared with men; the typical age of onset is 30 to 60 years.27 The classic reticular pattern presents with Wickham striae: symmetric, white, lacy patterns on the buccal mucosa that usually lack symptoms.25,27 Erythematous and erosive varieties can cause pain and burning.25 Oral lichen planus is less likely to resolve compared with cutaneous lichen planus, and patients experience relapses and remissions.27,29 Localized oral lichenoid reactions may occur due to hypersensitivity reactions to dental materials or other allergens.27

Asymptomatic disease requires no treatment. Topical corticosteroids are the primary treatment. Severe presentations may require therapy with systemic prednisone.29 Localized lesions may be managed with topical fluocinonide or clobetasol (Temovate) gel or oral steroid rinses; oral dexamethasone rinses may be used for more widespread lesions.25,27,29 Steroid-sparing options include topical calcineurin inhibitors tacrolimus (Protopic) and hydroxychloroquine (Plaquenil).29 The potential for malignant transformation of oral lichen planus is uncertain, with a range of 0% to 12.5% cited in the literature.25–27,29
Traumatic Fibroma
Fibroma is the most common oral soft tissue growth, which is thought to occur secondary to local trauma or irritation (Figure 10). Fibroma presents as a broad-based, smooth nodule or papule that usually is similar in color to the adjacent normal mucosa.22 Fibromas have a predilection for the buccal mucosa, intraoral lower lip, and tongue. The associated chronic repair process produces a dense collagenous lesion, sometimes with hyperkeratosis or ulceration of the overlying surface caused by continued trauma. Treatment consists of excisional biopsy, and there is no risk of malignant transformation.22

This article updates previous articles on this topic by Gonsalves, et al.,30 and Gonsalves, et al.31
Data Sources: A PubMed search was completed in Clinical Queries using the key terms oral medicine, oral disease, mucosal disease, leukoplakia, erythroplakia, erythroleukoplakia, pemphigus, pemphigoid, oral lichen planus, aphthous stomatitis, herpetic stomatitis, herpes labialis, oral candidiasis, thrush, geographic tongue, benign migratory glossitis, mandibular tori, maxillary tori, oral pyogenic granuloma, oral mucocele, oral mucus retention cyst, hairy tongue, and oral traumatic fibroma. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Cochrane Database of Systematic Reviews and the Agency for Healthcare Research and Quality. Search dates: October 2020 to February 2021, and November 2021.
The authors thank the Medical Library Staff at CoxHealth Medical Center for assistance with the references.
