
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2022;105(6):675-677
Author disclosure: No relevant financial relationships.
Key Points for Practice
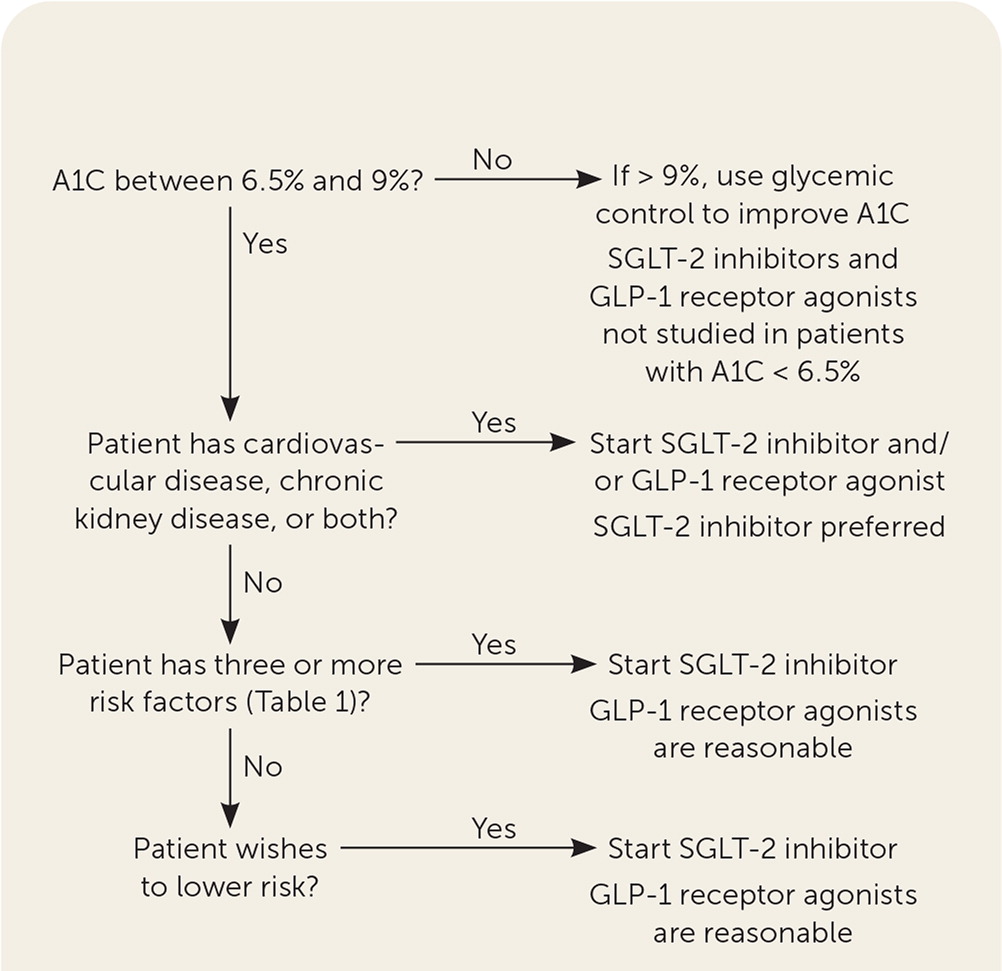
• To reduce overall mortality in patients with type 2 diabetes mellitus, the BMJ/MAGIC Group recommends prescribing SGLT-2 inhibitors in those with cardiovascular disease and/or chronic kidney disease or three or more risk factors for cardiovascular disease.
• GLP-1 receptor agonists are reasonable alternatives to SGLT-2 inhibitors in patients with similar risk profiles because this drug class also improves mortality, although to a lesser extent.
• Although SGLT-2 inhibitors and GLP-1 receptor agonists do not increase the risk of severe hypoglycemia, SGLT-2 inhibitors increase the risk of genital infections, and GLP-1 agonists have gastrointestinal adverse effects, especially at initiation and with high doses.
From the AFP Editors
Guideline Applicability
SGLT-2 Inhibitors
| Male sex |
| Asian, African, or Hispanic ethnicity |
| Age > 60 years |
| Family history of cardiovascular or kidney disease |
| A1C ≥ 6.5% |
| Current smoker |
| Uncontrolled hypertension (≤ 140/90 mm Hg) |
| Dyslipidemia (total cholesterol ≥ 200 mg per dL [5.18 mmol per L] or HDL cholesterol < 39 mg per dL [1.01 mmol per L]) |
In low-risk patients with less than three risk factors, SGLT-2 inhibitors still improve mortality, but absolute benefits are small. For patients who wish to reduce their cardiovascular and renal risk, SGLT-2 inhibitors are reasonable.
GLP-1 Receptor Agonists
GLP-1 receptor agonists improve mortality but to a lesser extent than SGLT-2 inhibitors. SGLT-2 inhibitors are superior to GLP-1 receptor agonists in improving cardiovascular and renal outcomes, except for nonfatal stroke.
The BMJ/MAGIC Group suggests GLP-1 receptor agonists as an alternative to SGLT-2 inhibitors for patients with type 2 diabetes, cardiovascular disease, and chronic kidney disease. In these very high-risk patients, GLP-1 receptor agonists reduce overall mortality, with an NNT of 42 (95% CI, 29 to 84) over five years.
GLP-1 receptor agonists reduce mortality in lower-risk patients, although absolute benefits are smaller. For patients with cardiovascular disease but not chronic kidney disease, GLP-1 receptor agonists reduce overall mortality, with an NNT of 59 (95% CI, 40 to 112) over five years. In patients with chronic kidney disease but not cardiovascular disease, the NNT is 77 (95% CI, 56 to 167) over five years.
Although GLP-1 receptor agonists improve mortality in low-risk patients, the absolute benefits are very small. For patients who wish to reduce their cardiovascular and renal risk, SGLT-2 inhibitors are preferred, but GLP-1 receptor agonists are reasonable.
Shared Decision-Making
Although SGLT-2 inhibitors are more effective than GLP-1 receptor agonists, benefits are similar. Prescribing choices should be based on patient preferences, medication adverse effects, and cost.
SGLT-2 inhibitors require monitoring for dizziness, hypotension, and renal dysfunction within three months of initiation and are contraindicated when glomerular filtration rate is reduced, usually to less than 30 mL per kg per 1.73 m2. Although SGLT-2 inhibitors increase the risk of genital infections, they do not appear to increase rates of Fournier gangrene or amputations. Tolerability to GLP-1 receptor agonists can be limited by gastrointestinal events, and starting at a low dose with slow titration is recommended. GLP-1 receptor agonists cannot be used in combination with dipeptidyl-peptidase 4 inhibitors. Most GLP-1 agonists (except semaglutide) are available only by injection and require storage below 86°F (30°C). [corrected]
SGLT-2 inhibitors and GLP-1 receptor agonists are associated with similar weight loss. Both can increase the risk of hypoglycemia if used in combination with glinides, insulin, or sulfonylureas but not as monotherapy. The cost of GLP-1 receptor agonists is about two to three times higher than SGLT-2 inhibitors. Cost was not considered in the recommendations.
Editor's Note: The NNTs and NNHs were calculated by the authors based on data in the systematic review.
This BMJ/MAGIC Group guideline is important because it proposes a new paradigm for diabetes therapy. Although we have long known that A1C targets are not effective, this guideline recommends focusing completely on cardiovascular and renal risk as long as A1C is less than 9%. The NNTs for SGLT-2 inhibitors to reduce mortality are truly impressive, although 1 in 7 patients will get an additional genital infection in five years. The systematic review did not show significant increases in Fournier gangrene or amputation despite early reports. GLP-1 receptor agonists are less beneficial and have common gastrointestinal effects, leading to a recommendation for slow dose tapering. Weight loss is similar between drug classes—nearly 2 kg (4 lb, 6 oz) with SGLT-2 inhibitors and 1.5 kg (3 lb, 5 oz) with GLP-1 receptor agonists.
The BMJ/MAGIC Group found that Asian, African, or Hispanic ethnicity was a risk factor for cardiovascular and renal outcomes and increased benefits of the medications, although race and ethnicity are social constructs that may not represent a genetic predisposition.
These recommendations and the systematic review add to the increasing evidence of the importance of these medications.—Michael J. Arnold, MD, Contributing Editor
The views expressed in this editorial are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Uniformed Services University of the Health Sciences, Department of Defense, Department of Veterans Affairs, or the U.S. government.
Guideline source: BMJ/MAGIC Group
Evidence rating system used? Yes
Systematic literature search described? Yes
Guideline developed by participants without relevant financial ties to industry? Yes
Recommendations based on patient-oriented outcomes? Yes
Published source: BMJ. May 11, 2021;373:n1091
Available at: https://www.bmj.com/content/373/bmj.n1091
