
Am Fam Physician. 2023;107(4):356-357
There are benefits to having a primary care physician or a usual source of care. Adults with a primary care physician have higher rates of preventive care, have improved communication with their care team, and receive more attention to social needs.1–3 Yet, not all individuals have equitable access to a primary care physician. The overall percentage of U.S. patients who reported having a usual source of care declined from 84% in 2000 to 74% in 2019, with wide variations across states, patient race, and insurance status.
The Primary Care Collaborative and the Robert Graham Center's 2022 Primary Care Evidence Report evaluated existing knowledge on the impact of having a usual source of care, examined data trends, and proposed policy strategies to ensure equitable access to primary care across the United States.4 A usual source of care can be defined at the clinician, clinic, or system level. Overall, 74% of the U.S. population reported having a usual source of care in 2019, with these patients more likely to be White, live in the Northeast, and have Medicare insurance. Iowa, Maine, Maryland, Michigan, Pennsylvania, and Vermont have higher percentages of residents who have a relationship with a primary care physician (about 80%), whereas Alaska, Mississippi, Montana, Nevada, North Dakota, Texas, and Wyoming have lower percentages (about 60%). The percentages are illustrated in Figure 1.
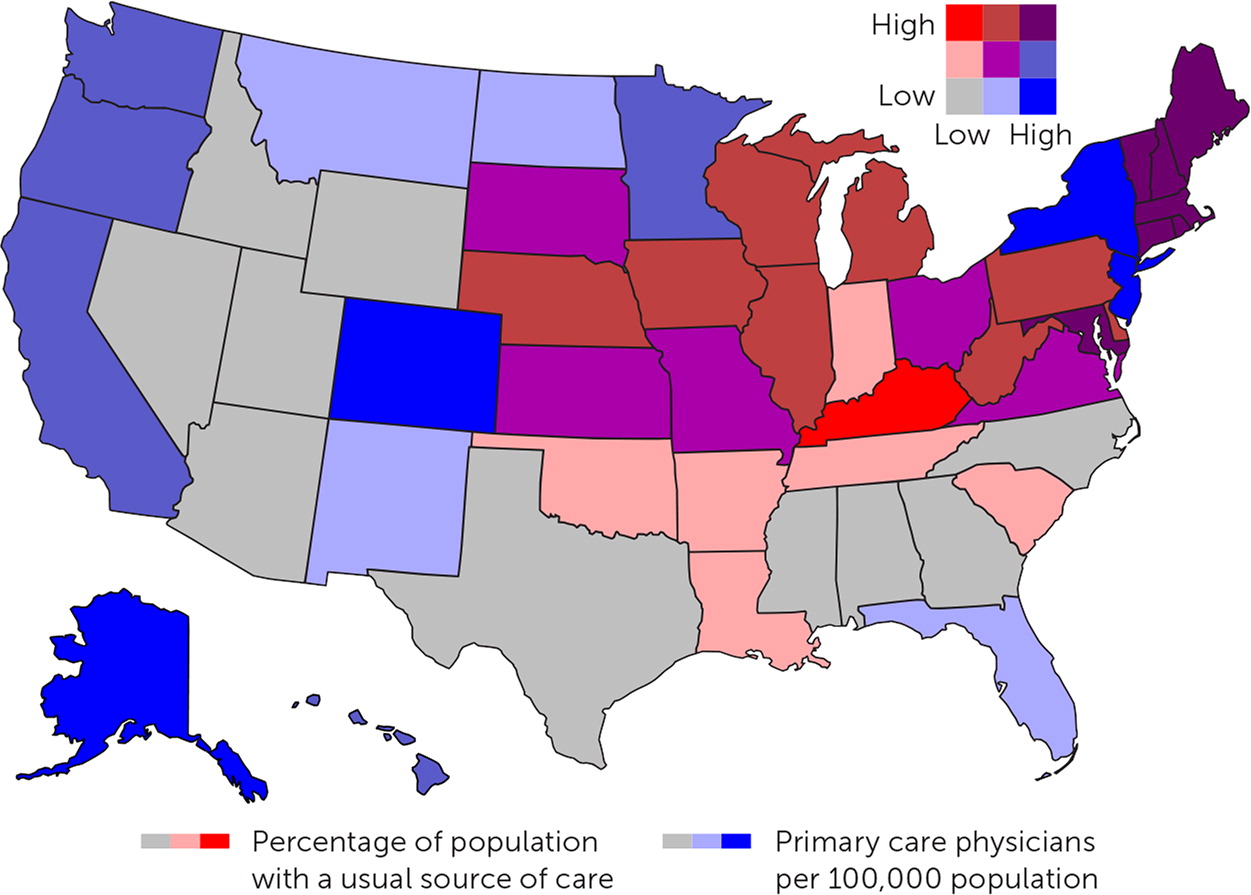
The reasons for a high or low reported rate of having a primary care physician may stem from clinician supply, payer mix, and whether the state expanded Medicaid under the Affordable Care Act. The District of Columbia has the highest primary care physician-to-population ratio but is average for the population percentage with a usual source of care. In comparison, New Hampshire experiences the inverse, with an average number of primary care physicians (80 per 100,000 people), and 84% of individuals report having a usual source of care. The number of primary care physicians in a state does not always directly correlate with access, and residents of rural regions are less likely than suburban or urban residents to identify a usual source of care.
Other factors that impact the odds of having a usual source of care include race (Black and Hispanic patients have a lower likelihood than non-Hispanic White patients) and insurance status (uninsured individuals are far less likely to have a usual source of care [odds ratio = 0.26]). Black and Hispanic patients reported using the emergency department more than White patients, and 20% of non-Hispanic Black individuals identified the emergency department as their usual source of care. These patients also reported better access to care compared with patients who use a primary care physician as their usual source of care. Given the 24-hour availability of the emergency department, this access is likely secondary to the structural differences in hours of operation and no appointment requirement.
The disparity in primary care relationships for Hispanic and Black communities exacerbates long-term health inequities. Historically, primary care has been the only discipline to improve health equity,5 but there is a long way to go to achieve equitable health outcomes. To improve access for medically underserved communities, barriers to a usual source of care must be addressed. Low Medicaid reimbursement may limit access to primary care physicians as practices limit the volume of Medicaid beneficiaries they see. Patients may be more likely to attend appointments if access is expanded (i.e., hours of availability and telemedicine options). High-deductible plans should exclude primary care physician visits from the deductible requirement to encourage patients to seek routine care. Finally, primary care physicians should reflect the neighborhoods they serve. Recruitment pathways for medical administrative positions, nurses, and physicians should actively seek out Hispanic, Black, and other ethnic minority individuals, and those from lower income backgrounds. Individuals of color should receive financial support to pursue training in health professions and to practice medicine in underserved communities.
