
Am Fam Physician. 2023;108(6):544-553
Author disclosure: No relevant financial relationships.
Childhood and adolescent sports participation is encouraged because of health and wellness benefits. However, the increasing number of young athletes means there is the potential for more sports-related overuse injuries. Most youth sports injuries occur at the bone’s relatively weaker growth centers: the epiphyses and apophyses. Little league shoulder and elbow are common overuse injuries in baseball and other single-arm dominant sports. Little league shoulder is a Salter-Harris fracture of the proximal humerus, and little league elbow is an apophysitis of the medial epicondyle. In both injuries, the athlete often reports decreased throwing velocity or accuracy. The physician should emphasize the Major League Baseball Pitch Smart guidelines when counseling on rehabilitation and prevention. Gymnast’s wrist is a distal radial epiphysis injury in which the patient reports chronic wrist pain. Gymnast’s wrist should be managed conservatively with immobilization. Spondylolysis is an important cause of overuse back pain in young athletes and can progress to spondylolisthesis. Patellofemoral pain syndrome presents with anterior knee pain, often made worse with running or descending stairs and improved with physical therapy. Osgood-Schlatter disease and Sinding-Larsen—Johansson disease are forms of knee apophysitis. Calcaneal apophysitis is a common cause of heel pain in young athletes and can be diagnosed clinically with the calcaneal squeeze test. Calcaneal apophysitis is treated conservatively, with good evidence for the use of heel cups and physical therapy.
In the United States, 40 million to 60 million children are involved in organized sports annually.1 Sports participation has many health and wellness benefits, but overuse injuries can occur in young athletes because of increased stress on the body without proper training. Organized sports are a contributor to these, often preventable, injuries.1–3 Children enter sports at a younger age, and the number of sports each child is involved in is increasing.1,2 This hypercompetitive culture has led some athletes to specialize in a specific sport for nine to 12 months out of a year. With early sports specialization, overuse injuries are becoming more common.2–4 Proper technique, resistance training, protective equipment, and avoiding early sports specialization are necessary for injury prevention in adolescents. This article focuses on overuse injuries (Table 1); however, assessing for nonmechanical musculoskeletal pain causes such as infection, rheumatologic causes, and malignancy is important. The history and physical examination can identify red-flag symptoms such as fever, weight loss, poor weight gain, night pain, or symmetric swelling. After the initial evaluation has excluded a non-mechanical cause of insidious onset pain, overuse injuries should be considered (Table 25–34).
| Recommendation | Sponsoring organization |
|---|---|
| Do not order advanced imaging studies (i.e., magnetic resonance imaging or computed tomography) for most musculoskeletal conditions in a child until all appropriate clinical, laboratory, and plain radiograph examinations have been completed. | American Academy of Pediatrics – Section on Orthopaedics and the Pediatric Orthopaedic Society of North America |
| Body part | Differential diagnoses | Key distinct feature |
|---|---|---|
| Shoulder | Acromioclavicular joint injury | Pain over the acromioclavicular joint, limited range of motion |
| Glenohumeral instability | Shoulder dislocation/subluxation, feeling of instability | |
| Little league shoulder | Common in throwing sports in children younger than 16 years who have decreased velocity and accuracy when throwing | |
| Rotator cuff tendinitis | Pain with overhead activities, weakness with external rotation | |
| SLAP lesion | Pain with overhead activities, painful popping or clicking, instability | |
| Elbow | Avascular necrosis of the capitellum | Pain and tenderness on the outside of the elbow, aggravated by gripping or throwing and common in children between 7 and 12 years of age |
| Little league elbow | Pain and tenderness on the inside of the elbow, aggravated by throwing | |
| Osteochondritis dissecans | Pain, swelling, and decreased range of motion, may feel like locking or catching | |
| Ulnar collateral ligament injury | Pain on the inside of the elbow, weakness with gripping and throwing, more commonly an acute injury | |
| Wrist | de Quervain disease | Pain and swelling at the base of the thumb, aggravated by gripping or twisting |
| Gymnast’s wrist | Pain and swelling on the inside of the wrist, aggravated by weight-bearing | |
| Intersection syndrome | Pain and swelling at the top of the forearm, aggravated by wrist and finger extension | |
| Scaphoid stress fracture | Pain in the anatomic snuffbox, aggravated by wrist extension and radial deviation | |
| Triangular fibrocartilage complex tear | Pain and clicking on the ulnar side of the wrist, aggravated by gripping | |
| Back | Herniated disc | Pain and numbness in the back and legs, may have muscle weakness |
| Lumbar facet joint syndrome | Pain and stiffness in the lower back, may radiate to the hips or thighs | |
| Scheuermann disease | Osteochondrosis of the vertebrae | |
| Spondylolisthesis | Forward slippage of one vertebra over another, may have back pain and stiffness | |
| Spondylolysis | Stress fracture in the pars interarticularis, often asymptomatic | |
| Knee | Meniscal injury | Pain and swelling in the knee, may have locking or catching sensation |
| Osgood-Schlatter disease | Pain and swelling below the kneecap, aggravated by activity | |
| Patellar tendinitis | Pain and tenderness below the kneecap, aggravated by jumping and running | |
| Patellofemoral pain syndrome | Pain around the kneecap, aggravated by activity and sitting for long periods | |
| Sinding-Larsen—Johansson disease | Pain and tenderness at the lower tip of the kneecap, aggravated by jumping and running | |
| Heel | Achilles tendinitis | Pain and swelling above the heel, worse with activity |
| Plantar fasciitis | Pain in the heel and arch, worse in the morning or after prolonged rest | |
| Sever disease | Pain and swelling in the heel, common in young athletes |
| Type of injury | History | Evaluation | Management | Average months to full recovery |
|---|---|---|---|---|
| Little league shoulder5–10 | Proximal shoulder pain Worse with throwing Decreased throwing velocity | Radiography may show widening of the proximal humeral physis Magnetic resonance imaging is usually unnecessary | 3 to 4 months of rest from throwing Biomechanics/physical therapy Major League Baseball Pitch Smart guidelines | 4 to 6 |
| Little league elbow10–13 | Medial elbow pain Worse with valgus stress and resisted flexion of the wrist | Clinical diagnosis Radiography may show physeal widening | 4 to 6 weeks of rest from throwing Biomechanics/physical therapy Return to throwing protocol Major League Baseball Pitch Smart guidelines | 3 to 4 |
| Gymnast’s wrist14–17 | Radial-sided wrist pain Worse with hyperextension, axially loading | Radiography may show a widening of the epiphyseal plate, positive ulnar variance | NSAIDs, immobilization, and physical therapy No upper extremity weight-bearing until pain-free | 3 to 4 |
| Spondylolysis and spondylolisthesis18–24 | Gradual onset of progressive low back pain Worsens with lumbar extension | Radiography, oblique view may show Scotty dog sign or slippage of one vertebra over another Magnetic resonance imaging can help in diagnosing acuity | Rest 2 to 6 months from aggravating activity Begin physical therapy and gradual return to play over 2 to 6 weeks Surgical referral for grade 3 or higher spondylolisthesis, neurologic deficits, or no improvement with conservative management | 3 to 10 |
| Patellofemoral pain syndrome25–27 | Anterior knee pain that is poorly localized around the patella Worsens with knee extension and after prolonged sitting | Clinical diagnosis Radiography for refractory cases or atypical presentations | Physical therapy for hip and knee biomechanics/strength Activity modification, ice, NSAIDs, patellar taping, and foot orthoses | 1 to 12 |
| Osgood-Schlatter and Sinding-Larsen— Johansson disease25–30 | Anteroinferior knee pain Tenderness over the tibial tubercle (Osgood-Schlatter) or patella-patellar tendon junction (Sinding-Larsen—Johansson) | Clinical diagnosis Radiography should be reserved for refractory cases | Activity modification, ice, NSAIDs, and patellar taping Physical therapy | 3 to 6 |
| Sever disease31–34 | Unilateral or bilateral heel pain Pain with one-legged heel test or calcaneal squeeze test | Clinical diagnosis Radiography should be reserved for refractory cases or pain lasting longer than 8 weeks | Rest from painful activities, NSAIDs Orthotics or heel cups Physical therapy | 1 to 2 |
Shoulder
Little league shoulder (i.e., proximal humeral epiphysiolysis) is an overuse injury that commonly occurs in young male pitchers between 11 and 16 years of age, with a peak incidence at 13 years of age. Little league shoulder also presents in tennis, swimming, gymnastics, and volleyball.5–7 Throwing a baseball is a complex activity that forces the proximal humerus to experience a large amount of rotational force. The shoulder begins in a position of maximal external rotation and abduction and then goes into a forced internal rotation and adduction.5,7,8
Patients typically report progressively worsening, diffuse, proximal shoulder pain with throwing that resolves with rest. Patients may also report a decrease in pitching velocity or accuracy. Patients often have tenderness to palpation over the lateral aspect of the proximal humerus and deficits in shoulder flexion, external rotation, and internal rotation due to pain.5,7,35
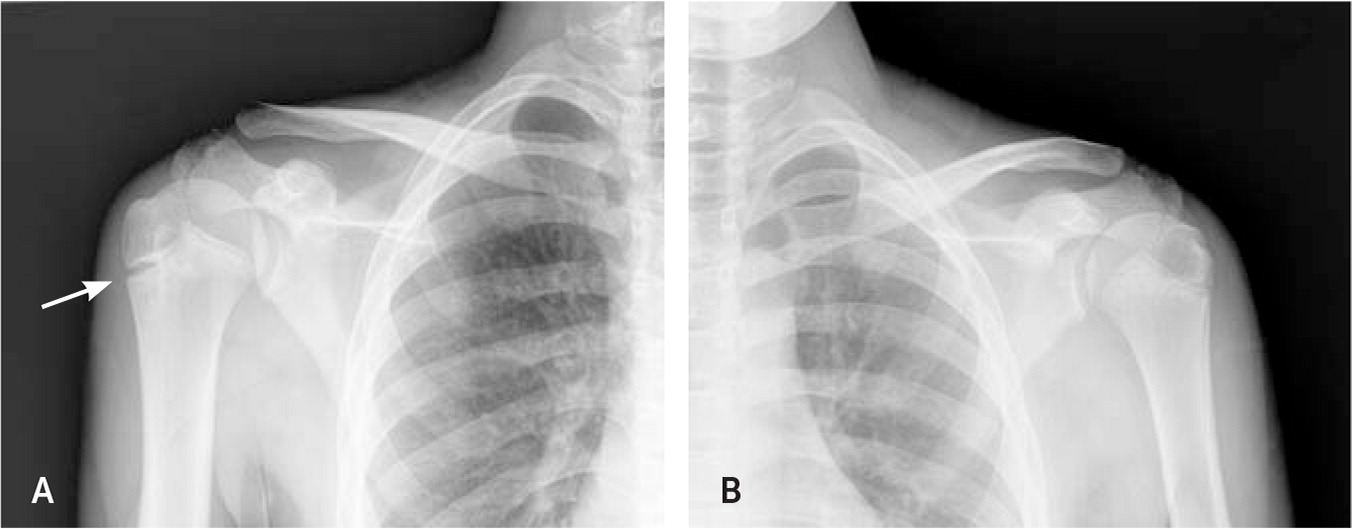
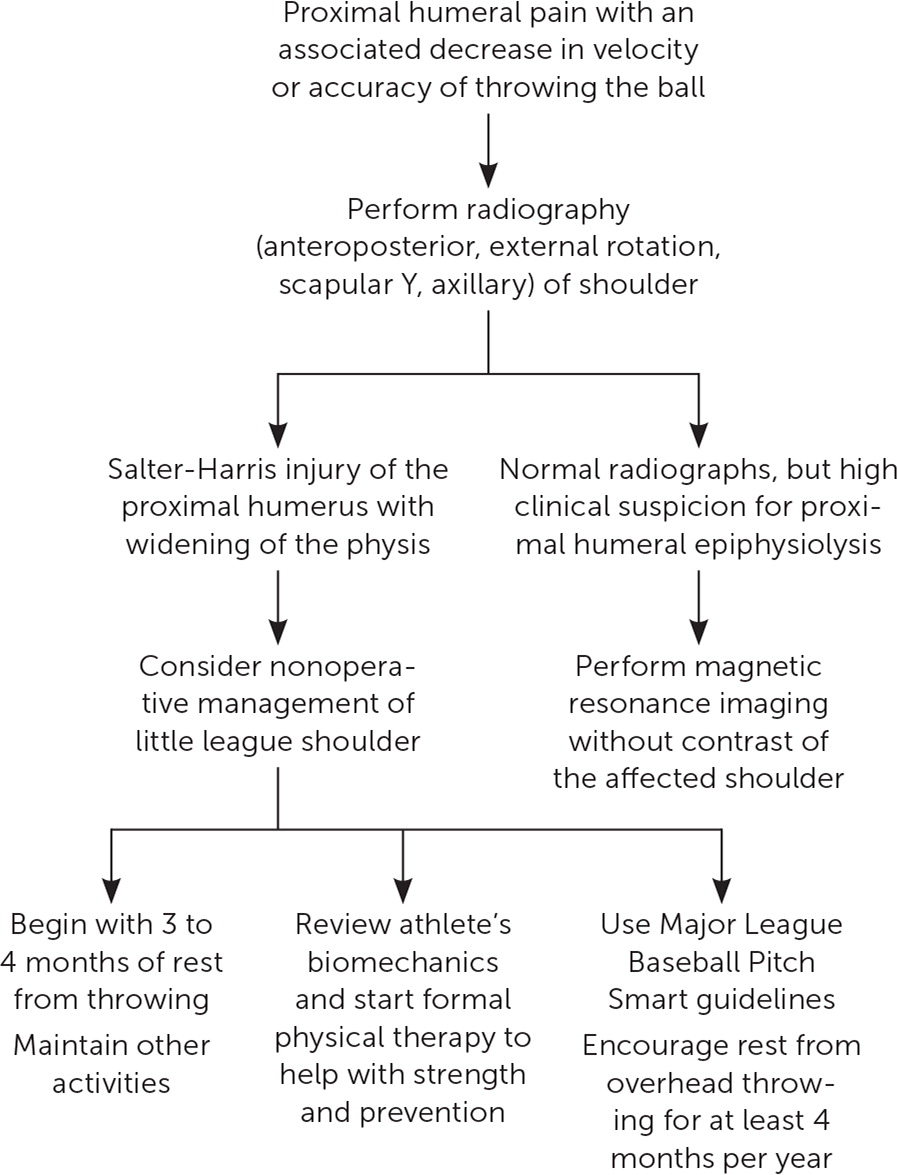
Initial imaging includes bilateral shoulder radiography that classically shows a widening of the proximal humeral physis consistent with a Salter-Harris fracture (the injury or fracture line extends through the growth plate or physis).5–7,35 Plain radiography should be performed using an anteroposterior view of the shoulder with the arm in external rotation (Figure 136). A scapular Y and axillary view should also be performed. Magnetic resonance imaging (MRI) is usually unnecessary but can be performed without contrast in a patient with negative radiographs and a high clinical suspicion. Imaging shows edema or a widening of the proximal humeral physis.5,6,37
Management of little league shoulder includes complete rest from throwing, physical therapy, and a gradual return to throwing protocol (allowing subthreshold activity below the levels that reproduce symptoms; Figure 2). The evidence suggests three to four months of rest from throwing while maintaining other activities before beginning a return to throwing protocol.5,7,9,35 Prevention is essential for young athletes and starts with assessing their biomechanics to ensure proper technique and that they generate power with their lower body instead of placing all the force on their upper extremities. Athletes should be involved with a strength program targeting core muscle groups, especially abdominals and quadriceps, and a stretching program to increase shoulder and thoracic mobility.7–9,35 Paying close attention to pitch counts and purposeful rest is important. The Major League Baseball Pitch Smart guidelines are a helpful tool organized by age group.10 In an athlete’s annual training cycle, rest from overhead throwing should be for at least four months, two months of which should be continuous. The tendency to overlook rest periods is a common argument against early sports specialization.6,7,9,35,37
Elbow
Little league elbow or medial epicondyle apophysitis is an overuse injury that occurs in adolescent baseball players between nine and 13 years of age.11,38 This is from the repetitive valgus load causing microtrauma to the medial elbow and is worse during the late cocking and early acceleration phases of throwing.11–13,38
These patients typically report medial elbow pain in their dominant arm and decreased velocity or accuracy when throwing. Patients may mention that they have recently increased the number of innings they have pitched or have joined a second team for more practice. On examination, the medial epicondyle is tender, and the pain is worse with valgus stress of the elbow and resisted wrist flexion.
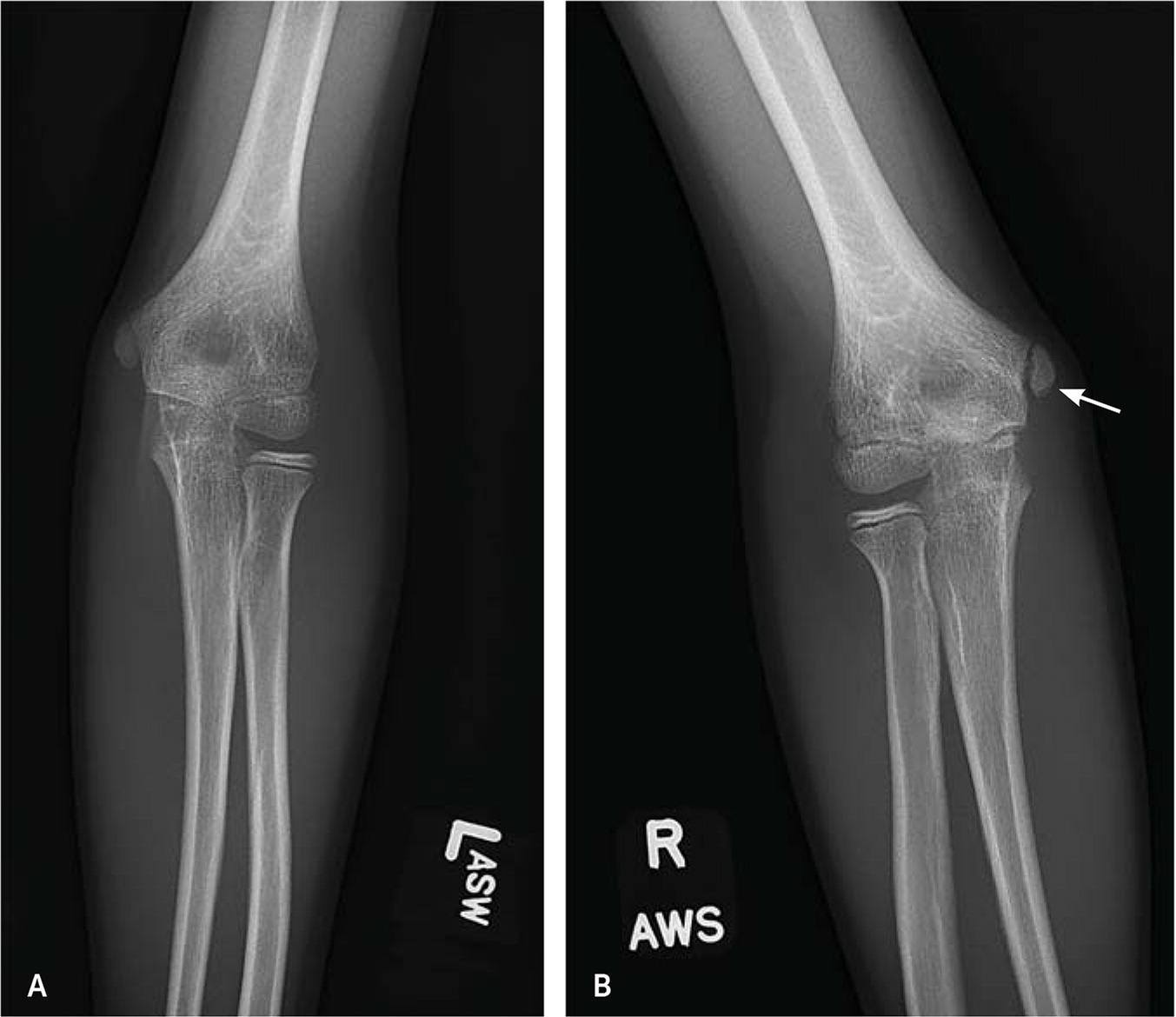
Treatment for little league elbow includes complete rest from throwing, physical therapy, and a gradual return to throwing protocol. The typical rest period is four to six weeks, and patients can usually return to competitive throwing after three months.11,12,38,39 Prevention is critical for the throwing athlete, and they should follow pitching guidelines, including four months of rest annually.10,38
Wrist
Gymnast’s wrist (i.e., distal radial epiphysitis) is an overuse injury that most commonly presents in females between eight and 15 years of age, with a peak incidence between nine and 13 years of age.14,15,40 Gymnast’s wrist is classically described in gymnasts, but can also present in divers, rock climbers, and weightlifters. In gymnastics, repetitive compressive and shearing forces are placed on the extended wrist, and the distal radius is at increased risk due to bearing about 80% of the axial load.14,16,17,40
These patients typically report chronic wrist pain on the radial side, made worse with wrist-loading movements, but may also have pain at rest, mild swelling, and a decreased range of motion. On examination, there is tenderness to palpation over the distal radial epiphyseal plate, pain with hyperextension and axial wrist loading, and reduced grip strength.14,15,40
The initial imaging of choice is plain radiography of the wrist (anteroposterior and lateral views). These views can show widening or haziness of the distal radial epiphyseal plate, cystic or sclerotic changes, palmar spurring of the metaphysis, and positive ulnar variance (distal articular surface of the ulna is more than 2.5 mm distal to the articular surface of radius).14,15,40 MRI is usually unnecessary but can be used for patients with negative radiographs and high clinical suspicion. MRI shows paraphyseal edema and irregular widening of the epiphyseal plate.15,41
Management of gymnast’s wrist primarily includes nonsteroidal anti-inflammatory drugs (NSAIDs), immobilization with activity restriction, and physical therapy. Patients should abstain from activity involving the affected wrist for four to six weeks and have the wrist immobilized in a short arm splint.14,15,40 Patients need to decrease upper extremity weight-bearing until the pain resolves, which could take up to three months. Physical therapy can improve the flexibility and strength deficits in the smaller, stabilizing muscles of the wrist and hand. Bracing can reduce forces through the radial physis by limiting wrist hyperextension, which may help reduce pain and prevent the injury from worsening.16,17,40
Back
Spondylolysis is an important cause of back pain in young athletes and is due to a fracture or defect in the pars interarticularis, typically occurring at the L5 vertebra, and can be unilateral or bilateral.18,19 Spondylolysis occurring bilaterally at the same vertebral level can progress to spondylolisthesis, the anterior or posterior translation (slippage) of one vertebra over the inferior adjacent vertebra.19 The classic presentation is low back pain that develops slowly over time and worsens with activity, especially hyperextension and spinal loading.19 The most common examination finding is pain with lumbar extension, hamstring tightness, and hyperlordosis.19,20
The stork test, or one-legged hyperextension test, has been used to help with diagnosis (Figure 4). Studies suggest that the stork test is not sensitive or specific and may not help differentiate spondylolysis from other causes of lower back pain.20,21,42 Although little evidence exists for physical examination maneuvers to diagnose spondylolysis, there is utility in palpating the spinous processes for a step-off deformity when assessing for spondylolisthesis because this indicates slippage19,22 (Figure 5). Anteroposterior, lateral, and oblique lumbar spine radiography should be performed. Oblique views are helpful to evaluate for a pars defect (Scotty dog sign). The lateral view allows for the assessment of vertebral alignment23,43 (Figure 644). If plain radiographs are negative but clinical suspicion is high, advanced imaging should be pursued with an MRI of the lumbar spine.23,24,43 MRI that preferentially sequences bone spares the patient from radiation exposure, detects early stages of spondylolysis, and has a sensitivity equivalent to computed tomography.23,24,43



When diagnosed and treated early, spondylolysis has an excellent prognosis with conservative management.45,46 One study demonstrated a greater than 90% healing rate with conservative management of early-stage defects.45 Rehabilitation for patients with spondylolysis and low-grade spondylolisthesis should include rest from painful activities, especially those that involve lumbar extension. A flexion-based physical therapy program should be initiated early in treatment, with the possibility of returning to play in six to eight weeks. Depending on injury severity (Table 319,47,48), recovery can last up to six months.19,43,45 The benefits of bracing are unclear.46,47 Referral to a spine surgeon is necessary if there is high-grade or progressive spondylolisthesis (grade 3 or higher), development of any neurologic deficits, or no improvement following conservative management for at least six months.19,22,46,47,49
| Grade | Criteria | Management |
|---|---|---|
| 1 | 1% to 25% of anterior slippage | Asymptomatic or mildly symptomatic can trial conservative management |
| 2 | 26% to 50% of anterior slippage | Asymptomatic or mildly symptomatic can trial conservative management |
| 3 | 51% to 75% of anterior slippage | If persistent symptoms or progression of slip-page, refer for surgical consultation |
| 4 | 76% to 100% of anterior slippage | Refer for surgical consultation |
| 5 | > 100% of anterior slippage | Refer for surgical consultation |
Knee
Patellofemoral pain syndrome is a common cause of knee pain in children. It is characterized by anterior or retropatellar knee pain that worsens with knee extension, such as running, and is made worse with climbing or descending stairs or doing a leg squat. A single-leg squat often shows the knee going into a valgus deformity due to imbalances. Patients often report pain that is worse when standing up from a seated position (i.e., theater sign). Patellofemoral pain is usually treated with physical therapy; surgical intervention is rarely needed.25–27 Exercise therapy should be tailored to the individual and include hip (targeting posterolateral hip musculature) and knee exercises (resisted squats or resisted knee extension) to improve strength, flexibility, endurance, and proprioception.
Apophysitis of the knee is a common cause of childhood knee pain due to repetitive traction from the patellar tendon. Apophysitis can occur at the tibial tubercle (Osgood-Schlatter disease) or the inferior patella (Sinding-Larsen—Johansson disease).50 These conditions typically present in athletes between 10 and 15 years of age with insidious onset of anterior knee pain exacerbated by activities such as running and jumping.25,50 Pain is localized, and on examination, patients will be tender over the tibial tubercle in Osgood-Schlatter disease, whereas patients with Sinding-Larsen—Johansson disease will be tender over the patella-patellar tendon junction.25,28,50 Swelling over the affected area may be present but is usually mild.28 Although imaging is not necessary for a diagnosis, lateral radiography is often performed and typically shows fragmentation or ossicles in Osgood-Schlatter disease, whereas patients with Sinding-Larsen—Johansson disease often have calcification and ossification at the patella-patellar tendon junction.25 Osgood-Schlatter disease and Sinding-Larsen—Johansson disease are treated similarly, and most patients note improvement after conservative management with activity modification, icing of the affected area, NSAIDs, and physical therapy.25,28 Surgery, typically involving ossicle excision, is rarely needed, and consideration should be reserved for patients with severe, debilitating pain following physeal closure.29,30
Heel
Calcaneal apophysitis (i.e., Sever disease) is one of the most common causes of heel pain in young athletes.31,32 This overuse injury, caused by repetitive forces at the calcaneal epiphyseal plate, typically presents insidiously with unilateral or bilateral heel pain in high-impact athletes between eight and 15 years of age.31,32 Diagnosis is made clinically with one-legged heel standing or the calcaneal squeeze test, both of which have greater than 95% sensitivity and specificity33,51 (Figure 7). Radiography is occasionally performed, but signs of inflammation, such as sclerosis and fragmentation at the calcaneal growth plate, have been found in up to one-half of athletes without pain, making radiography unreliable for diagnosis.33,34 Radiography should be reserved for atypical presentations, severe symptoms, or refractory cases that persist longer than eight weeks. Treatment is conservative and includes rest from painful activities, ice, NSAIDs, orthotics or heel cups, and physical therapy.31,33 The average time to full recovery is approximately 60 days; however, intermittent flare-ups are common until the apophysis fuses.31,32

This article updates a previous article on this topic by Cassas and Cassettari-Wayhs.36
Data Sources: A PubMed search was completed in Clinical Queries using the key terms little league shoulder, proximal humeral epiphysiolysis, medial epicondyle apophysitis, distal radial epiphysitis, little league elbow, gymnast wrist, spondylolysis, pediatric spondylolisthesis, calcaneal apophysitis, patellofemoral pain syndrome, Osgood Schlatter, Sinding Larsen Johansson, adolescent overuse injuries, childhood overuse injuries, and pediatric overuse injuries. The search included randomized controlled trials, clinical trials, case reports, diagnostic studies, systematic reviews, and meta-analyses. The search included publications between 2012 to 2022. Landmark articles were included outside of that range for completion. DynaMed, UpToDate, the Cochrane database, U.S. Preventive Services Task Force, and Google Scholar databases were also searched. Search dates: July to October 2022, and September 27, 2023.
