
Am Fam Physician. 2023;108(6):554-561
Author disclosure: No relevant financial relationships.
Chronic kidney disease (CKD) affects approximately 15% of the U.S. population, and many people are unaware of their diagnosis. Screening may be considered for patients with cardiovascular disease, diabetes mellitus, hypertension, age 60 years and older, family history of kidney disease, previous acute kidney injury, or preeclampsia. Diagnosis and staging of CKD are based on estimated glomerular filtration rate (eGFR), excessive urinary albumin excretion, or evidence of kidney parenchymal damage lasting more than three months. eGFR should be determined using the CKD-EPI creatinine equation without the race variable. Risk calculators are available to estimate the risk of progression to end-stage renal disease. When possible, serum cystatin C should be measured to confirm eGFR in patients with CKD. Blood pressure should be maintained at less than 140/90 mm Hg, with a systolic blood pressure target of 120 mm Hg or less for patients tolerant of therapy, using an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker. Sodium-glucose cotransporter-2 inhibitors and metformin should be considered in patients with CKD and type 2 diabetes who have not reached their glycemic goal. Intravenous iodinated contrast media temporarily reduces eGFR and should be avoided in patients with advanced CKD. Interdisciplinary management of patients with CKD is important for reducing morbidity and mortality, and patients at high risk of progression to end-stage renal disease should be referred to a nephrologist.
Chronic kidney disease (CKD) affects about 15% of the U.S. population; however, 9 out of 10 people do not know they have impaired renal function.1 CKD is diagnosed in Black people three times as often as in White people.1,2 CKD is more common in women than men, but men are more likely to progress to end-stage renal disease (ESRD).1,2 CKD is more common in patients 60 years and older compared with younger patients, and more advanced disease is associated with an increased risk of cardiovascular disease and death.1,3
Definition and Staging
CKD is defined as an estimated glomerular filtration rate (eGFR) of less than 60 mL per minute per 1.73 m2 or markers of kidney damage, including functional or structural abnormalities such as albuminuria (albumin excretion rate of 30 mg or more daily or albumin/creatinine ratio of 30 mg per g or greater), abnormal urinalysis, and polycystic or dysplastic kidneys. CKD persists for more than three months.4 The Kidney Disease: Improving Global Outcomes (KDIGO) staging of CKD is based on the eGFR category and the level of persistent albuminuria (Table 1).5 High levels of proteinuria are associated with an increased risk of disease progression, even if the eGFR is normal. ESRD is defined as the need for renal replacement therapy or renal transplant. Risk calculators can help physicians identify patients with CKD at high risk of developing ESRD (https://www.mdcalc.com/kidney-failure-risk-calculator); however, it is unknown if these calculators improve the management of CKD.3
| eGFR categories | Range (mL per minute per 1.73 m2) | Persistent albuminuria categories | ||
|---|---|---|---|---|
| A1 | A2 | A3 | ||
| < 30 mg per g | 30 to 300 mg per g | > 300 mg per g | ||
| G1 (normal or high) | ≥ 90 | Low | Moderate | High |
| G2 (mildly decreased) | 60 to 89 | Low | Moderate | High |
| G3a (mildly to moderately decreased) | 45 to 59 | Moderate | High | Very high |
| G3b (moderately to severely decreased) | 30 to 44 | High | Very high | Very high |
| G4 (severely decreased) | 15 to 29 | Very high | Very high | Very high |
| G5 (kidney failure) | < 15 | Very high | Very high | Very high |
The National Kidney Foundation/American Society of Nephrology Task Force recommends that physicians use the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation without the race variable included to calculate eGFR (https://www.mdcalc.com/calc/3939/ckdepi-equations-glomerular-filtration-rate-gfr). This equation included diverse populations in its creation, is widely available, and performs well clinically.6 Serum cystatin C, which is produced at a constant rate and is independent of race, should be used to confirm eGFR in patients with CKD; combining it in an enhanced equation with CKD-EPI or creatinine is more accurate than either alone.6 Cystatin C levels may not be as accurate in acute kidney injury, inflammatory states, or thyroid dysfunction and may not be as widely available as the CKD-EPI creatinine equation.7
Albuminuria should be quantified by a urine albumin/creatinine ratio. The urine albumin/creatinine ratio is preferred to a urine protein/creatinine ratio due to more widespread standardization and improved accuracy at lower levels of albuminuria.5 Testing should be obtained from a first-morning sample or a 24-hour urine collection to improve accuracy.5,8 An elevated urine a lbumin/creatinine ratio on two or more samples over at least three months indicates CKD because a transient increase in albumin/creatinine ratio may represent acute causes such as urinary tract infection, acute kidney injury, and systemic infection.5,8
Screening and Indications
Most patients with CKD are asymptomatic. Symptoms are more common in advanced disease and may include fatigue, nausea, vomiting, anorexia, insomnia, and edema.3 KDIGO recommends screening patients with cardiovascular disease, diabetes mellitus, or hypertension and those at high risk (i.e., age 60 years and older, family history of kidney disease, previous acute kidney injury, or preeclampsia) for CKD based on eGFR and albumin/creatinine ratio.9 The U.S. Preventive Services Task Force is reviewing its CKD screening recommendation.10 No randomized controlled trials have shown improved outcomes with screening of asymptomatic individuals.3
Evaluation
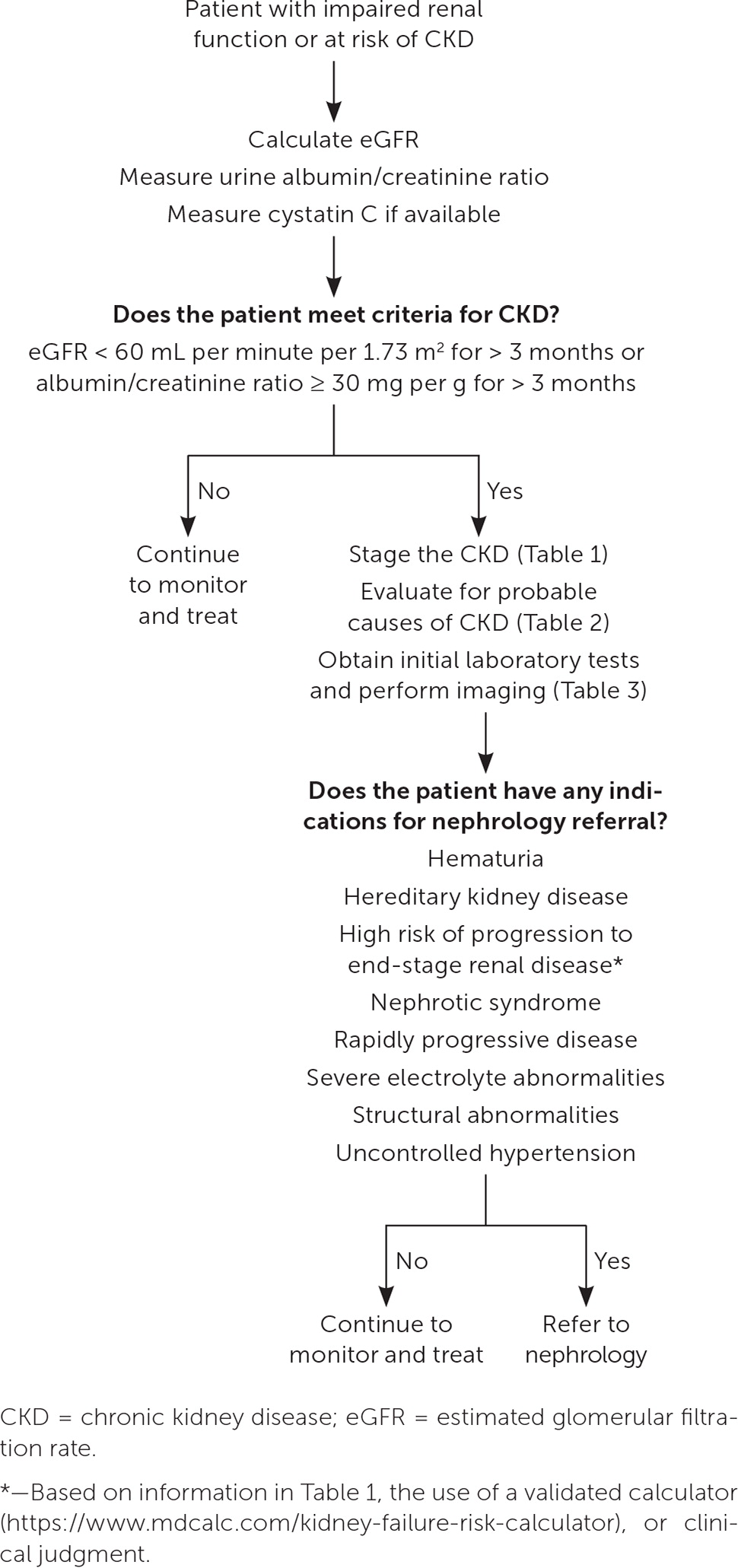
The most common causes of CKD are diabetes (38%) and hypertension (26%).11 Other causes can be divided into nephrotoxic medications; malignancy; and anatomic, autoimmune, genetic, infectious, metabolic, obstructive, and vascular processes (Table 23,5). More than one process may be present. A history and physical examination (including blood pressure and weight measurement) should be performed. The recommended initial laboratory and imaging tests for all patients with CKD are listed in Table 3.3,5 Testing for less common underlying conditions, such as autoimmune conditions or polycystic kidney disease, is based on the presumed diagnosis suggested by the history and physical examination. Indications for early referral to a nephrologist include hematuria, hereditary kidney disease, high risk of progression to ESRD, nephrotic syndrome, rapidly progressive disease, severe electrolyte abnormalities, structural abnormalities, or uncontrolled hypertension.3 Figure 1 provides steps for the initial diagnosis, staging, and management of CKD.3,5,12
| Category | Examples |
|---|---|
| Anatomic | Congenital anomalies of urinary tract |
| Reflux nephropathy | |
| Single kidney | |
| Autoimmune | Cryoglobulinemia |
| Poststreptococcal glomerulonephritis | |
| Systemic lupus erythematosus | |
| Genetic | Alport syndrome |
| Polycystic kidney disease | |
| Infectious | Hepatitis B virus |
| Hepatitis C virus | |
| HIV | |
| Malignancy | Multiple myeloma |
| Renal cell cancer | |
| Medications/drugs | Chemotherapy |
| Herbal supplements (anthraquinones, aristolochic acid) | |
| Immunotherapy | |
| Intravenous drug use (cocaine, heroin) | |
| Lithium | |
| Nonsteroidal anti-inflammatory drugs | |
| Metabolic | Diabetes mellitus* |
| Obstructive | Benign prostatic hyperplasia |
| Kidney stones | |
| Pelvic tumor | |
| Vascular | Heart failure |
| Hypertension* | |
| Peripheral artery disease |
| Test | Rationale |
|---|---|
| Albumin/creatinine ratio | Assess albuminuria; rules out transient causes and determines risk of progression |
| A1C | Screen for diabetes mellitus or assess current glycemic control |
| Lipid panel | Screen for coexisting dyslipidemia |
| Renal ultrasonography | Look for structural abnormalities |
| Serum electrolytes | Assess electrolyte abnormalities that may be due to chronic kidney disease |
| Urinalysis/urine microscopy | Assess for markers that suggest causes of chronic kidney disease (e.g., cellular casts, hematuria, pyuria, tubular concentrating defects) |
Management and Prevention
Many strategies that have been recommended to limit the progression of CKD are also recommended to prevent CKD in patients with multiple risk factors. Implementing lifestyle interventions, avoiding nephrotoxic substances, and managing comorbid health conditions demonstrate benefits.
Evidence-based lifestyle interventions for the prevention and treatment of CKD include a diet low in sodium (less than 2,000 to 2,300 mg per day), a structured moderate-intensity exercise program of at least 150 minutes per week, and smoking cessation.5,13–15 Dietary protein should be limited to 0.6 to 0.8 g per kg per day in patients with CKD stage 3 or 4 to reduce disease progression.13,15–17 Resistance exercise and adequate caloric and micronutrient intake are recommended to decrease the risk of sarcopenia.13,15–17 Plant-based diets have demonstrated benefits in the prevention and management of CKD because of reduced animal protein intake, increased consumption of anti-inflammatory phytonutrients, and their positive effect on controlling body weight, blood pressure, and blood glucose.18–21
Patients engaging in strenuous endurance exercise should ensure adequate hydration to avoid dehydration-related kidney injury and rhabdomyolysis.22 The use of nephrotoxic drugs should be limited or avoided where possible.23 Many medications require dosing adjustment in patients with CKD due to the potential for direct renal insult or a change in their magnitude of effect in patients who have reduced renal function.5,13 In addition to routine age-based vaccinations, a pneumococcal vaccination should be administered to patients between 19 and 64 years of age with ESRD and those on dialysis.24,25
HYPERTENSION
In 2021, KDIGO’s updated guideline on the management of hypertension in patients with CKD recommended that lifestyle and medication interventions target a systolic blood pressure of 120 mm Hg or less if tolerated.26 This recommendation is based on evidence from a high-quality randomized controlled trial showing that lowering systolic blood pressure below 120 mm Hg is associated with a reduction in cardiovascular events and all-cause mortality in patients who do not have diabetes but are at increased risk of cardiovascular events (e.g., known cardiovascular disease other than stroke, CKD with eGFR of 20 to 60 mL per minute per 1.73 m2 excluding polycystic kidney disease, 10-year cardiovascular disease risk of greater than 15% based on Framingham risk score, or age 75 years or older).26,27 The benefit of this more aggressive approach in patients with CKD stage 4 or 5, and in those with comorbid CKD and diabetes, is less certain when compared with the risk of adverse events such as acute kidney injury and electrolyte disturbance.26 This contrasts with the 2019 U.S. Department of Veterans Affairs/Department of Defense guidelines, which recommend a target blood pressure of less than 140/90 mm Hg.13 Patients with known cardiovascular disease and those at increased cardiovascular risk are most likely to benefit from more intensive management.26 Patients with hypertension, diabetes, CKD, and moderate to severe albuminuria (A2 to A3) should be treated with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker.5,13,26 Both classes are preferred in patients without diabetes who have CKD and microalbuminuria due to a demonstrated reduction in progression to ESRD, with a goal of reaching the highest-tolerated dose to maximize benefit.5,13,24,28
Finerenone (Kerendia), a nonsteroidal mineralocorticoid receptor antagonist that lowers the risk of disease progression and cardiovascular events when used in patients with CKD and type 2 diabetes, may be considered in patients with continued disease progression despite maximal medication therapy.29,30 Discontinuation of renin-angiotensin-aldosterone system blockades in patients with CKD stages 4 or 5 is not routinely recommended; however, there is little supporting evidence that discontinuation leads to worse outcomes.31–33 Other cardiovascular risk reduction strategies, such as the use of statins, should be used according to established guidelines.34 Adults 50 years and older with CKD who are not on dialysis and those between 18 and 49 years of age with CKD and risk factors qualify for statin therapy.34
DIABETES
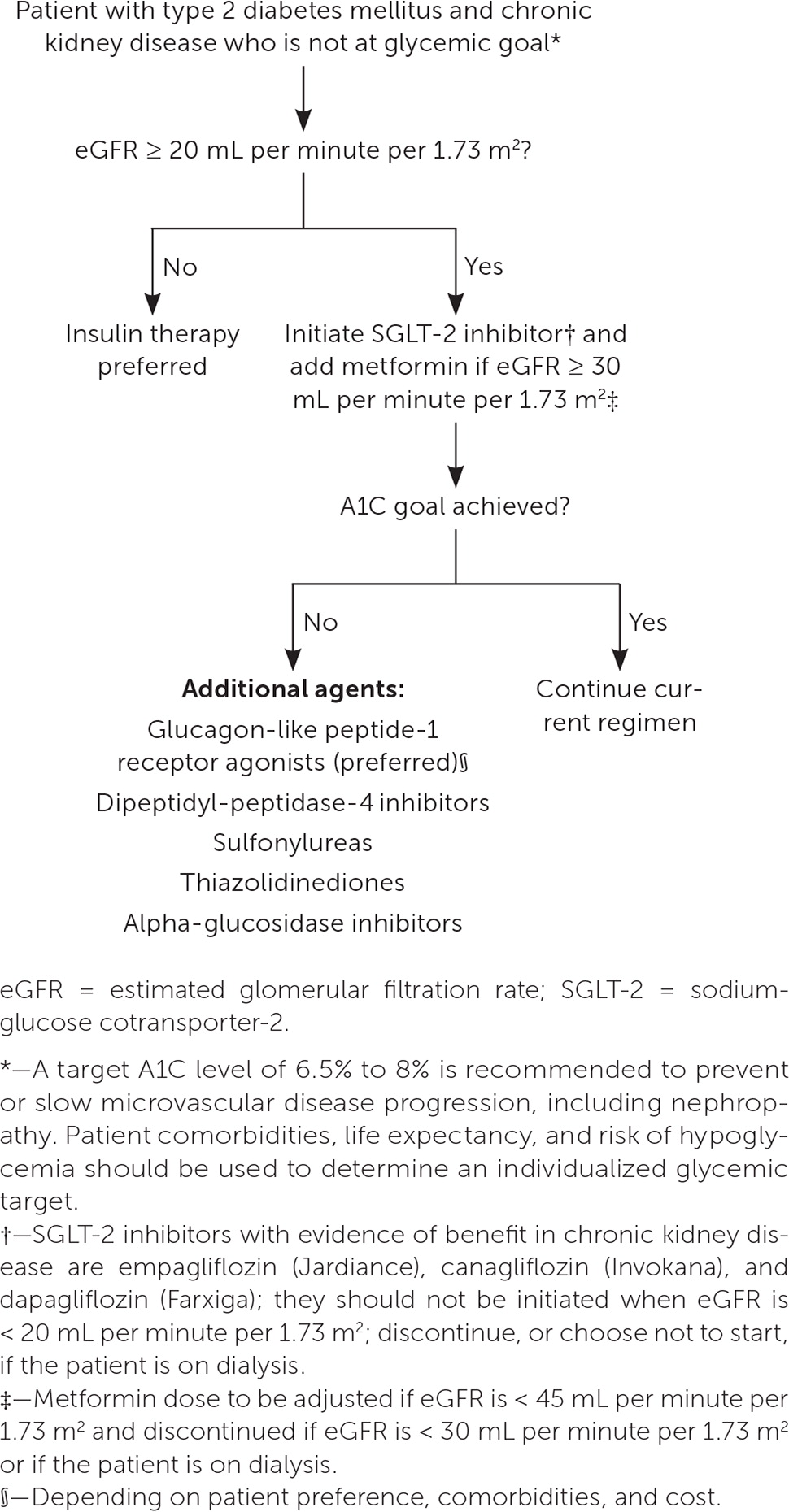
In patients with CKD and diabetes, a target A1C of 6.5% to 8% is recommended to prevent or slow microvascular disease progression, including nephropathy.5,13 Patient comorbidities, life expectancy, and risk of hypoglycemia should be used to determine an individualized glycemic target.5,35 Sodium-glucose cotransporter-2 (SGLT-2) inhibitors and metformin are recommended as first-line treatments in patients with CKD and type 2 diabetes who have not reached their glycemic goal. SGLT-2 inhibitors reduce renal disease progression and cardiovascular disease risk, independent of their effect on glycemic control, with risk reduction noted in patients with CKD who do not have diabetes.35–38 Due to the risk of diabetic ketoacidosis, SGLT-2 inhibitors are contraindicated in patients with type 1 diabetes.13 Metformin is recommended in CKD stages 1 to 3 with an eGFR of 30 mL per minute per 1.73 m2 or greater, but it is contraindicated in stages 4 and 5.33,35 Glucagon-like peptide-1 (GLP-1) receptor agonists also demonstrate protective effects against CKD progression, cardiovascular disease, and all-cause mortality.13,35,39 SGLT-2 inhibitors and GLP-1 receptor agonists share the additional benefit of a very low risk of hypoglycemia.5,38–40 Figure 2 outlines recommendations for glucose-lowering medications in patients with CKD and diabetes.35
ANEMIA
Serum hemoglobin should be measured at least once per year in patients with CKD stage 3 or greater because of the increased risk of anemia in CKD.13,41 Detailed information on screening for and monitoring complications of CKD is listed in Table 4.5,13,41,42 Table 5 offers testing and management recommendations for complications of CKD.3,5,13,41,42 Anemia may have several causes; therefore, a reticulocyte count and measurement of ferritin, transferrin saturation, folate, and vitamin B12 levels are indicated in patients with anemia to confirm the etiology.41 For patients requiring iron supplementation, deciding on the route of administration depends on the severity of iron deficiency, previous response to oral repletion, cost, and venous access.41 Administration of erythropoiesis-stimulating therapy requires careful consideration of the potential reduction in blood transfusion and anemia symptoms relative to the risk of complications such as stroke, loss of vascular access, and hypertension.41
| Complication | Recommended test | CKD stages 1 and 2 | CKD stage 3 | CKD stage 4 | CKD stage 5 |
|---|---|---|---|---|---|
| Anemia (screening) | Hemoglobin | As indicated | At least annually | At least twice per year | |
| Anemia (monitoring) | Hemoglobin | As indicated | At least every 3 months | ||
| Ferritin, folate, reticulocyte count, transferrin, vitamin B12 | Initially for diagnostic purposes, then as indicated | ||||
| Bone mineral disease | Serum calcium, phosphorus | Not indicated | Every 6 to 12 months | Every 3 to 6 months | Every 1 to 3 months |
| Dual energy x-ray absorptiometry | Not indicated | Once in patients with known bone mineral disease or risk of osteoporosis, then as indicated | |||
| Serum parathyroid hormone | Not indicated | Baseline, then as indicated | Every 6 to 12 months | Every 3 to 6 months | |
| Serum 25-hydroxy-vitamin D | Not indicated | At baseline, then as indicated | |||
| Cardiovascular disease | Lipid panel | At baseline, then as indicated | |||
| Hyperkalemia | Serum potassium | At baseline, then as indicated | |||
| Metabolic acidosis | Serum bicarbonate | At baseline, then as indicated | |||
| Complication | Relevant tests | Management recommendation |
|---|---|---|
| Anemia | Hematocrit Hemoglobin | Determine etiology of anemia by measuring ferritin, folate, reticulocyte count, transferrin, and vitamin B12 Consider iron supplementation if deficient or nephrology referral for erythropoiesis-stimulating therapies if hemoglobin < 10 g per dL (100 g per L) |
| Bone mineral disease | Dual energy x-ray absorptiometry Serum calcium Serum parathyroid hormone Serum phosphate Serum 25-hydroxyvitamin D | Consider phosphate-lowering therapies in patients with chronic kidney disease stage 5 or end-stage renal disease Consider vitamin D supplementation in cases of deficiency Treat osteoporosis as in the general population |
| Hyperkalemia | Serum potassium | Recommend low-potassium diet Consider potassium binders (sodium zirconium cyclosilicate [Lokelma], patiromer [Veltassa]) in patients with refractory hyperkalemia |
| Metabolic acidosis | Serum bicarbonate | Consider oral bicarbonate supplementation for refractory acidosis |
Erythropoiesis-stimulating medications should not be initiated in patients with CKD and a starting hemoglobin level of more than 10 g per dL (100 g per L); a target of no more than 11.5 g per dL (115 g per L) is recommended.13
BONE MINERAL DISORDERS
Beginning in CKD stage 3a, serum levels of calcium, phosphate, parathyroid hormone, and alkaline phosphatase should be obtained, with frequency determined by the CKD stage and previous results.42 25-Hydroxyvitamin D testing is recommended in patients with CKD stage 3 and greater, with treatment of insufficiency or deficiency.42 Bone mineral density testing with dual energy x-ray absorptiometry is recommended in patients with CKD stage 3 and greater and biochemical evidence of bone mineral disease, a history of fragility fracture, or an elevated risk of osteoporosis as defined by U.S. Preventive Services Task Force guidelines, provided that results would change management.42 Treatment of osteoporosis in patients with CKD is similar to that of the general population.42,43
Calcitriol, active vitamin D analogues, and calcimimetics should not be given to lower elevated parathyroid hormone levels in patients with CKD stages 3 or 4 due to unclear benefits to bone health and an increased risk of abnormalities in calcium and phosphorous levels.13,42 They may have a role in the treatment of secondary hyperparathyroidism in patients with CKD stage 5 or ESRD.42
USE OF CONTRAST MEDIA IN PATIENTS WITH CKD
Intravenous iodinated contrast media temporarily reduces eGFR and should be used selectively in patients with CKD. Preprocedure and postprocedure isotonic intravenous fluids should be used for nonurgent imaging studies to decrease the risk of worsened kidney function through improvement in renal perfusion and contrast dilution. Intravenous iodinated contrast media is not recommended in patients with diabetes and CKD stage 3a or in patients without diabetes and CKD stage 3b or greater.13 If contrast studies are considered in patients with CKD stages 4 or 5, a nephrologist should be consulted for management recommendations. No evidence suggests that holding angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, diuretics, or other medications for contrast studies decreases the risk of kidney injury.44 Evidence is insufficient to demonstrate a clear protective effect with preprocedural N-acetylcysteine use, and there are potential adverse effects on myocardial and coagulation function when given at higher intravenous doses.13,44 Renal replacement therapy should not be used routinely as prophylaxis against contrast-induced injury.13 Newer generation gadolinium-based contrast media can be safely used in patients with CKD.45
Indications for Referral
Early collaboration between family physicians and nephrologists allows for an interdisciplinary approach to patient education, detection, and management of complications, and planning for the progression of renal disease.
This article updates previous articles on this topic by Gaitonde, et al.46; Rivera, et al.47; and Baumgarten and Gehr.48
Data Sources: A PubMed search was completed in Clinical Queries using the key terms chronic kidney disease and management. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. The Cochrane database, DynaMedex, and Essential Evidence Plus were also searched. If studies used race or gender as patient categories, but did not define how these categories were assigned, they were not included in the final review. Studies that addressed concerns with including race in diagnosis and management are explicitly mentioned in the article. Search dates: January 4, 2023; May 12, 2023; and September 19, 2023.
