
Fam Pract Manag. 2000;7(6):23-29
Part-time practice yields equal performance, improved satisfaction
As more and more physicians move into part-time and “9-to-5” practice arrangements, there has been some concern that decreased work hours may translate into inferior care. But a study published in the April 2000 Archives of Family Medicine suggests that physicians' work hours have little effect on patient care. Looking at patients' perceptions in 11 measures of primary care performance (access, continuity of care, comprehensiveness, clinical interaction, etc.), researchers found no statistically significant difference overall between physicians who worked “overtime” (more than 65 hours per week), full time (40 to 65 hours per week) or part-time (less than 40 hours per week).
Physicians who worked more than 65 hours per week scored significantly higher in the visit-based continuity of care category than physicians working fewer hours, “but this appears to carry a cost to those physicians in the area of personal and professional satisfaction,” wrote the authors. The “overtime” physicians were significantly less satisfied with the amount of time they had for family and personal life and with the amount of time they spent with each patient.
The survey did not attempt to measure the effects of decreased work hours on physicians' technical competence and general knowledge base.
Revised documentation guidelines at least a year away
The Health Care Financing Administration (HCFA) has nearly completed its review of the “new framework” evaluation and management (E/M) documentation guidelines proposed by the AMA last year, according to Part B News, but implementation of occur until sometime next year.
The newsletter reports that Paul Rudolph, MD, HCFA's medical officer at the Center for Health Plans and Providers, told attendees at a recent American Health Lawyers Association conference that HCFA has “not committed to a timeline” for implementing revised guidelines and that pilot testing the guidelines could take “at least six months.” Pilot tests probably won't begin until later this year, at the earliest. HCFA still must decide what it will pilot test, design the tests and identify a contractor to administer them, Rudolph said.
Until revised guidelines are implemented, physicians must continue using either the 1995 or 1997 version.
Evaluation and management (E/M) code utilization in family practice
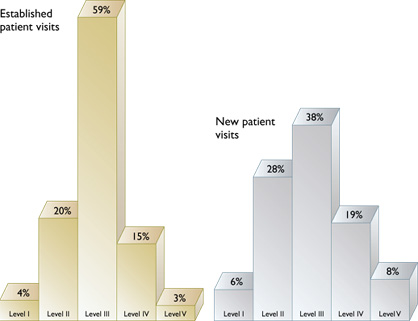
Source: 1998 Health Care Financing Administration data.
FDA begins review of over-the-counter drug policy
As part of the most sweeping effort since 1972 to examine its over-the-counter (OTC) drug policy, the Food and Drug Administration (FDA) will hold a hearing this month to discuss several OTC issues, including its role in switching products from prescription to OTC status.
The FDA has been asked that OTC status be granted to a number of drugs that now require a prescription, such as diuretics, antihypertensive agents, cholesterol-lowering drugs, antidiabetic drugs, asthma treatments and oral contraceptives.
Switching appropriate drugs to OTC sale can benefit the health care system “by providing consumers easy access to certain drugs that can be used safely for conditions that consumers can self-treat without the help of a health practitioner,” reports the FDA in the April 27 Federal Register.
While the OTC drug review has been hailed by drug companies, it could “backfire on the industry,” reports the April 28 USA Today. The insurance industry has asked the agency to be more aggressive in switching safe prescription drugs to over the counter, even when the manufacturers disagree.
Quote. Endquote.
“It goes from slow to slower. I've seen cemeteries that have more activity than this place.”
Senate Minority Leader Thomas Daschle, commenting in the May 6 Washington Post on Congress' failure to act on key legislation, including a patients' bill of rights and a prescription drug benefit for Medicare.
Lawsuit challenging resource-based practice expenses dismissed
Family physicians can expect higher Medicare payments through 2002 now that a U.S. District Court judge has dismissed a lawsuit that would have halted the Health Care Financing Administration's (HCFA's) new method of paying physicians for Medicare services.
Until 1999, the practice expense component of Medicare payments for physician services was based solely on historical charges, which undervalued most office services and overvalued hospital procedures. As a result of the Balanced Budget Act of 1997, HCFA is gradually decreasing the percentage of payment based on historical charges and is introducing payment based on resource-based practice expenses (RBPEs), which take into account the costs for clinical staff, equipment, supplies and overhead. Currently the ratio is 50:50, but by 2002, the practice expense component will be based entirely on resources.
The subspecialist groups initiating the lawsuit sought to freeze practice expense payments at the current ratio. According to the Practice Expense Fairness Coalition, which lobbied Congress against the lawsuit, “Halting implementation now would lock in unfair payment levels for thousands of physician services.”
Money buys happiness
It's been widely reported that although the United States spends more on health care than any other industrialized nation, Americans do not have the best health outcomes in the world. But we do get something for our money, according to a recent report from Johns Hopkins University, which found that Americans enjoy better access to care and better service than people in other countries.
Pill splitting
To stem the rising costs of prescription drugs, UnitedHealth Group is now requiring patients to purchase higher dosages of certain drugs and split the pills in half. Critics say the practice increases the risk of dosing errors, but the health plan argues that it is a simple way to save money.
Medicare on trial
Several states, associations and politicians have filed “friend-of-the-court” briefs in support of a suit filed against the Department of Health and Human Services by the Minnesota attorney general. The suit alleges that Medicare's payment formula violates Minnesota's Fifth Amendment right to equal protection under the law and its 10th Amendment right to sovereignty by permitting “wide disparities” in reimbursements, premiums and benefits.
Going broke
Nearly half of Americans who filed for bankruptcy last year did so at least in part because of their inability to pay medical bills, according to a forthcoming study of U.S. bankruptcy filings, cited in the April 25 Washington Post. The majority of filers had health coverage. Elderly people and households headed by women were hardest hit by medical costs.
Equal care?
How physicians manage their patients with acute myocardial infarction may depend on the patient's insurance, according to a report published in the March 27 Archives of Internal Medicine. After adjusting data for severity and baseline measures, researchers found that patients belonging to commercial health plans and Medicare received more health care resources than those covered by HMOs or Medic-aid or those without insurance.
Teen depression
While 30 percent of family physicians and pediatricians routinely ask their adolescent patients about depression, only 11 percent ask them about suicide, according to a nationwide study conducted at Saint Francis Hospital and Medical Center in Hartford, Conn. Less than half the physicians surveyed indicated they were comfortable identifying adolescent depression, even though three-quarters of them had been trained in assessing and treating depression.
Preventing dementia
Elderly people with fewer — or less satisfying — relationships have a greater risk of dementia than those with a strong social network, according to a study published in the April 15 Lancet. The three-year study of 1,203 elderly people found that poor social interaction increased the risk of dementia by 60 percent.
Complementary medicine
To lessen patient concerns regarding impending surgery, Blue Shield of California is offering its PPO members free audio tapes to help them employ guided imagery and “tap into their natural power to relax and heal.” According to Blue Shield, a committee of medical experts from the University of California at San Francisco and at Los Angeles found sufficient evidence that guided imagery can decrease surgical complications, postoperative pain and anxiety before and after surgery.
Press 1 for …
Health care providers in Michigan received an earful earlier this year when they called Blue Cross and Blue Shield's toll-free number for Medicare inquiries. Instead of getting answers to their Medicare questions, callers received an invitation from a phone sex hot line promising to fulfill their fantasies, according to the Detroit Free Press. After some providers complained, Blue Cross republished the guide that contained the incorrect phone number.