
Before making the leap from private practice to employed practice, consider how the new arrangement will affect your productivity and your bottom line.
Fam Pract Manag. 2011;18(4):18-21
Donna Izor is a practice management consultant with West Pinnacle Consulting, LLC, in Waterbury, Vt. Author disclosure: no relevant financial affilia-tions disclosed.
This question – “Why did your productivity decrease when we hired you?” – is one that board members and hospital senior management frequently ask after bringing a successful private-practice physician into employment and reviewing the subsequent practice financials. Often, the numbers aren't what they expected, and they wonder what happened. Did they expect too much, or did the physician slow down after becoming an employee?
The newly employed physician often wonders the same thing. Although he feels busier than ever, he also feels less productive – and now, perhaps, disrespected by management.
Much has been written about the financial loss organizations experience per employed physician and the reasons for it. The Medical Group Management Association's Cost Survey for Primary Care Practices: 2010 Report Based on 2009 Data finds a median loss of $124,807 per full-time family physician. Clearly, becoming a financial loss to your employer is a real possibility. If you are considering the move from private practice to employed practice, you and your prospective employer can both benefit from a clear sense of what to expect. Here are some key issues to consider.
Expected clinical work hours
Many private-practice physicians schedule patient visits during set hours yet remain available at other times based on their patients' needs. In employed situations, the expected number of clinical work hours may be significantly lower. Know how many hours you actually spend to achieve your pre-employment productivity levels and how a change in clinical work hours might affect revenue for your practice.
Payer mix
It is not uncommon for physicians in private practice to limit the insurance plans they accept or the number of underinsured or uninsured patients they see. Once employed, the physician may see an influx of Medicaid and Medicare patients. Understanding the differences in payer mix will help you predict the effect that employment will have on your practice's bottom line. This will be especially important if your compensation will be based on revenue rather than a payer-neutral measure such as relative value units.
Loss of in-suite testing
You may currently be providing lab services within your office, or you may work with an outside lab but bill for the laboratory services. As an employed physician, you may be required to use the hospital laboratory, thus moving this revenue stream from your practice to the hospital. This may increase the overall revenue for the organization but decrease the revenue to the practice.
The answers to a few key questions will help you understand how this change could affect you:
Will patients be required to go to the hospital for laboratory services?
Will I be able to continue to offer phlebotomy?
Will these changes affect the number of staff who currently work in the practice?
Will the change in net revenue for the practice affect my expected income?
Changes in staffing
Bringing current office staff into a hospital-based salary and benefit structure can significantly add to the overall expenses of the practice. In addition, the organization may have staffing ratios that are greater or less than what you currently have in your practice.
Your staff's satisfaction can also affect your productivity, so handle the transition carefully. Don't underestimate how your staff will react once they know that you are contemplating employment. They may bring you their concerns about continued employment, seniority, changes to their salary and benefits, etc. Show empathy and be supportive, but don't make promises for the employer, which has policies and procedures that will need to be followed. When appropriate, encourage staff to meet with the hospital's human resources department to answer their questions directly and avoid miscommunication.
Changes in technology
At the July 13, 2010, announcement of the final rules for achieving meaningful use of electronic health records (EHRs), U.S. Health and Human Services Secretary Kathleen Sebelius stated, “When electronic health records are well-designed and implemented correctly, they can be a powerful force for reducing errors, lowering costs, raising quality of care and increasing doctor and patient satisfaction.” But an EHR can also disrupt productivity for an extended period during training and implementation. Be sure to review your prospective employer's EHR so you can assess how it may affect your time in the exam room and patient flow within the practice. Also, take into account the time you will need to set aside for training and acclimating yourself and your staff to the new system. If you do not have keyboarding or other necessary skills, arrange for this training in advance.
Regulatory review
When physicians sell their practices to hospitals or other large entities, they sometimes need to update the practice facility to comply with regulatory standards. For example, a practice may have to make physical changes related to the Americans with Disabilities Act or the Occupational Safety and Health Administration regulations. The cost of bringing a practice facility up to standards for regulatory review can be significant. Add to that the costs and time associated with training and making workflow changes to ensure compliance. While these expenses are unavoidable, you should at least know up front what will be required.
Practice operations
Anticipating the workflows of the practice will allow you to better understand how employment could affect your productivity. Here are some questions to consider:
Documentation. Does the organization require documentation on the same day of the visit? Is this how your practice currently handles documentation? What clinical guidelines does the organization use? Would documenting compliance with these guidelines decrease your number of visits per day?
Nursing staff. How do the employed practices use nursing staff? Are nurses dedicated to a provider or shared? Are they located near the physician or in a central area? Do they perform telephone triage? Who calls in prescriptions? How does this compare to your practice? Will it affect your efficiency?
Meetings. What standard meetings will you and your staff be required to attend? Are these held during patient care hours? Are covering staff provided to maintain patient flow? Are there other meetings the employer will expect you to attend?
Billing. Will billing be moved to the hospital system? Will your current billing staff be reassigned to that department? How will your patient collections and payment policies change? How will these new policies be communicated to your patients? Will certain patients now qualify for financial assistance through the hospital? All of these issues can affect your practice finances.
Overhead expenses
Some hospitals are choosing not to assign overhead expenses to the practices they purchase; others assign actual overhead costs; and still others assign a set percentage to all units of business. Depending on which method your employer uses, it could inflate – or deflate – your practice expenses. Take time to understand what overhead costs will be assigned to your practice and what current costs, if any, your employer will absorb.
Retirement planning
Some physicians see employment as a way to transition toward retirement. Naturally, this can affect their productivity levels. If you anticipate retiring in the next few years, discuss this with your employer. You'll want to consider the following questions: Is there a documented plan describing how your patients will be moved to other providers, and is it consistent with your intent? Is there an agreed-upon time line for your retirement? Do you expect to participate in the recruitment and training of a new physician? Is semiretirement an option?
EMPLOYED VS. PRIVATE PRACTICE
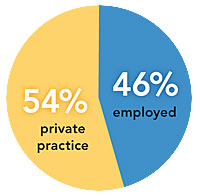
The percentage of U.S. physicians who own their own practices is declining. In 2004–2005, 54.4 percent of physicians reported full or part ownership of their practices.1 Today, that percentage is likely closer to 48 percent, assuming an annual decline of approximately 2 percent.2 With significant economic pressures on private practices, this decline is expected to continue.
Clarifying expectations
Physicians are attracted to employed practice for a number of reasons, including an approaching retirement, ongoing concerns over Medicare payment reform, the high costs of electronic health records and uncertainty about accountable care organizations. Whatever your reason, having clear expectations will help both you and your new employer have a successful transition.
