
In six steps, you can make your referrals more efficient and please patients in the process.
Fam Pract Manag. 2011;18(6):9-14
Dr. Jarve is a practicing primary care physician and a champion for workflow improvement at Spectrum Health Medical Group in Grand Rapids, Mich. David Dool is a senior process engineer with Spectrum Health Medical Group. Author disclosure: no relevant financial affiliations disclosed. Acknowledgments: We would like to thank Kim Hamilton and Kristine Solomon, who were instrumental in implementing this referral process. We would also like to acknowledge John Byrnes, MD, and the instructors in the “Spectrum Health – Health Care Performance Improvement” course for giving us the tools to make this transformation possible. Editorial assistance in the preparation of this article was provided by Beyond Words, Inc. Although Beyond Words supplied paid professional editing services, this does not indicate its endorsement of, agreement with or responsibility for the content of the article. The services of Beyond Words were paid for by Spectrum Health.
Patient satisfaction and high-quality care depend on effective coordination of care not just within a primary care physician's office but also between primary and specialty care physicians. This requires that an efficient, timely referral process be in place, as well as a closed-loop tracking system for referral completion, correspondence and patient feedback.
This article describes a successful referral process that has been used in the primary care practice of a major Midwest regional health care system. Although our new process was put into place following a formal gap analysis and quality improvement (QI) process, the tools described can be used by other primary care physicians – leading to increased patient satisfaction and more efficient office practices – without having to go through a QI process.
Steps on the way to better referrals
Based on our experience, we have identified six steps in improving the referral process in a primary care office.
Step 1: Improve internal office communication. In any primary care office, effective communication between the physician and the referral coordinator is essential to initiate the referral process. Typically, the referral coordinator is a medical office secretary responsible for scheduling a patient's appointment with a specialist, informing the patient about the details of the appointment and providing documentation to the specialist's office. The method of communication between the physician and the referral coordinator is, at its best, a standardized, comprehensive form filled out by the physician, whether on paper or electronically. Often, however, it is just a note written on a piece of paper. With such a beginning, the chances of an efficient, timely referral process are significantly reduced.
The first step in bridging this internal communication gap is developing a patient referral form. It needs to be simple for the physician to complete but must include all the information the referral coordinator will need to properly schedule an appointment for the patient. In a paper-based practice, pre-printed patient information labels are often included in the patient's chart; these can easily be attached to the top of the referral form.
Referral form
In addition, the patient referral form should include at least the following:
Date,
Referring physician's name,
Diagnosis,
Urgency of referral (stat, urgent or routine),
What service is being requested (consult only, testing only, follow-up, or consult and treat),
Which specialist the patient is being referred to.
The primary care physician is often reviewing the patient's chart when filling out the referral form. This is a prime opportunity to specify the information or documents that need to be included when communicating with the specialist (e.g., lab results, X-rays or visit notes). Finally, it is helpful if the referral form contains a section for the referral coordinator to add some notes regarding preferred times and dates for the patient's appointment and the results of follow-up communications with the patient.
Although this example refers to a paper-based system, the same information could easily be incorporated into a macro for pulling the information into a referral order in an electronic health record (EHR) system. In this scenario, the patient information would already be electronically attached to the order and a label would not be required.
Step 2: Engage the patient in scheduling. At checkout, either the patient will present a completed paper referral form or the referral coordinator will access an electronic version. The referral coordinator then has an opportunity to actively engage the patient in the coordination of his or her care. Depending on the type of appointment, the coordinator may be able to phone the specialist's office and obtain an appointment before the patient leaves. When a patient interacts directly with the referral coordinator in arranging the date and time, the likelihood of compliance is increased.
Even if the appointment cannot be scheduled immediately, the referral coordinator can ask the patient for date and time preferences. This extra effort to provide immediate service to patients circumvents the numerous phone calls and voice messages typically required to communicate appointment information or reschedule when dates and times don't work.
Whether the appointment is scheduled immediately or not, the coordinator can give the patient maps and directions to the specialist's office at this time.
Step 3: Facilitate the appointment. After the patient has an appointment scheduled – and sometimes even before a specialist's office will schedule an appointment – the proper information must flow between the primary care physician and the specialist. Specialists' offices often provide their own forms to referring physicians' offices, identifying the information they need in order to complete their part of the patient's care. These forms, along with the recommended documents indicated by the primary care physician on the patient referral form, guide the referral coordinator in this next step of the process.
Optimizing this flow of information reduces unnecessary calls, faxes and e-mail messages between cooperating offices. More important for patients, it can eliminate delays and duplication of laboratory tests, radiology imaging and procedures. For example, specialists may need or the primary care physician may want to send specific lab results. When these are not sent promptly as a part of normal procedures, the specialist may mistakenly assume that the tests have not been done, triggering a duplicate test. This repetition of testing leads to overutilization of resources, increases costs, wastes the patient's time and can increase the risk of morbidity.
Step 4: Track referral results. Once the referral has been scheduled and the proper information transferred, the patient's chart goes back in the chart rack or the encounter is closed in the EHR. Many primary care offices see this as the end of the referral process, but actually it is only the end of the first stage.
After the patient sees the specialist, results should be returned to the primary care office, typically in the form of a consult letter that is routed to the primary care physician. Unfortunately, if the patient fails to keep the appointment or the results of the visit are not sent to the primary care office, there is usually no obvious signal to the primary care staff that continuity of care has been broken. This failure is often not discovered until the patient returns to the primary care office for a follow-up visit or calls to find out his or her results. This inadvertently transfers the follow-up burden to the patient. In the worst case, a seriously ill patient might never contact either practice, assuming that “no news is good news.”
If a practice is not using an EHR, or if the EHR does not have the ability to track important steps in the referral process, a simple spreadsheet like the one shown below can be used to do the tracking. With this method, the referral coordinator enters pertinent data into the spreadsheet when he or she receives a patient referral form from the primary care physician. Each spreadsheet record should include at least the following data:
Patient name,
Physician or clinic referred to,
Diagnosis,
Date of referral request.
REFERRAL TRACKING SPREADSHEET
A spreadsheet like the one shown below can help track referral requests from initial receipt by the referral coordinator through response from the referral specialist.
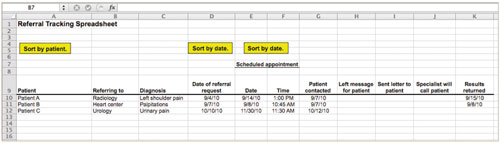
Developed by Spectrum Health. Copyright © 2011 Spectrum Health. Used with permission. Physicians may adapt for use in their own practices. All other rights reserved. Any user of this form or any adaptation thereof releases Spectrum Health from any and all liability.
Once the date and time of the appointment are known, they should also be entered in the spreadsheet, along with the date and method of patient contact. Finally, there should be a column for the date the results from the specialist were received at the primary care office.
This spreadsheet essentially becomes the work queue for the referral coordinator. For example, by scanning and sorting the columns, it is easy to visualize which referral appointments have yet to be confirmed. (There can be a time lag before an appointment is scheduled, particularly when requests must be faxed to a specialist's office.)
Other delays and breakdowns in communication also become obvious and can be dealt with. For instance, a second delay frequently occurs during the process of communicating with the patient. Even when every effort is made to speak to the patient directly by phone, the process often includes messages left on voicemail, e-mail messages or messages posted to the patient's online health record. Again, the spreadsheet makes it obvious when that communication loop has not been closed. If a practice's EHR system has the ability to pull reports about this information, then referring to these reports would achieve the same result.
Often, the longest delays occur during the wait for the actual appointment and during the post-appointment wait for results to be sent from the specialist. By sorting data by date of appointment, it is possible to determine what calls need to be made to ensure that the patient kept the appointment and that the return of results from the specialist is expedited.
Step 5: Analyze data for improvement opportunities. After referrals have been tracked like this for a number of months, the spreadsheet or a similar EHR report becomes a valuable historical database of information, especially about the relative timing of appointments with various specialists. Practices can use at least four specific pieces of information to streamline the referral process:
The time it takes to schedule or confirm an appointment with a given specialist;
The time between the day an appointment is set up and the day it takes place;
How often a patient misses an appointment;
The time between the appointment and the arrival of a post-appointment letter from the specialist regarding a given patient.
With these data in hand, it is possible to identify tendencies of different specialists and uncover process problems that can be improved. For instance, you might determine that it takes an average of six weeks for a patient to get an appointment with Dermatologist A but only two weeks to get an appointment with Dermatologist B. This allows you to work proactively – perhaps meeting with Dermatologist B to develop a closer working relationship or meeting with Dermatologist A to streamline the referral process. Either would result in increased patient satisfaction.
Step 6: Gather patient feedback. Better communication, new tools and the elimination of unnecessary phone calls are all important to the efficiency of the referral process. But what does this do for patients? Do they really know that their appointment was scheduled in a more timely manner? Do they realize that unnecessary tests were avoided? Do they recognize that continuity of care has been enhanced by proactively tracking the return of specialists' results?
Perhaps not. However, we can ask patients about things that matter to them, such as these:
Their ability to get an appointment when they wanted it;
Whether they were notified of the appointment in a timely manner;
How long they had to wait to see a specialist;
The suitability of the instructions they received;
Their overall experience with the specialist.
A patient satisfaction survey specifically developed to answer these kinds of questions can be implemented at any time as a benchmarking tool. It is especially valuable when a new referral process is being integrated into standard office practice. But it can also be used as a tool for gathering longer-term feedback about the continued effectiveness of the referral process.
By obtaining feedback from patients about their experiences with the referral process and the specialists they have seen, it is possible to identify areas where the process is still not adequately patient centered. It also accelerates the identification of possible patterns of patient dissatisfaction within a practice's referral base. This can lead to further improvement of the process. Over time, the increased efficiency and accuracy of the referral process can lead to increased quality of care and patient satisfaction.
Patient Satisfaction Survey: Referral Process - Coordination of Care
Regarding your referral to: __________________________________
We thank you in advance for completing this survey. We are striving to improve your experience when you are referred to a specialist, and your feedback and comments will help. Please fill out this survey and return it in the enclosed envelope after you have seen the specialist.
Instructions: Please rate the service you received by checking the box that best describes your experience.
| Very poor | Poor | Fair | Good | Very good | |
| Ability to get an appointment when you wanted (day of the week, time of day, etc.) | ☐ | ☐ | ☐ | ☐ | ☐ |
| Length of time until you were notified of your appointment. | ☐ | ☐ | ☐ | ☐ | ☐ |
| Length of time until you saw the specialist (appointment date). | ☐ | ☐ | ☐ | ☐ | ☐ |
| Instructions provided by our staff (directions, appointment time, special preparations, etc.) | ☐ | ☐ | ☐ | ☐ | ☐ |
| Overall rating of care received from specialist. | ☐ | ☐ | ☐ | ☐ | ☐ |
| Other comments: | |||||
| Your name (optional): | |||||
| Phone number (optional): |
Developed by Spectrum Health. Copyright © 2011 Spectrum Health. Used with permission. Physicians may adapt for use in their own practices. All other rights reserved. Any user of this form or any adaptation thereof releases Spectrum Health from any and all liability.
Is referral process improvement really worthwhile?
Two questions can be legitimately raised in relation to this six-step referral process. Is it too labor intensive to be worth the effort, and is it outdated in light of the implementation of EHR systems?
Any time a new workflow is introduced, it is easy to identify the additional work that will be generated. However, it is also important to understand the savings in labor that the new workflow can produce.
For example, by developing a standardized referral form, not only is communication between the primary care physician and the referral coordinator streamlined, but costly rework is avoided. This can be seen when incomplete information is provided to the specialist. At that point, a request for information is returned to the primary care office. This necessitates retrieving the patient's chart or going back into the EHR record, obtaining the relevant information and sending that information back to the specialist. This duplication of the original effort can easily waste 15 to 20 minutes of staff time. If the error isn't discovered until the patient has arrived at the specialist's office, it can delay care.
In another example of workflow savings, the tracking spreadsheet in this process requires approximately one minute of data entry per referral. The costs associated with this additional labor are quickly offset when the spreadsheet is effectively used as the referral coordinator's work queue. Rather than searching through a stack of charts or referral forms for pending appointment confirmations, the coordinator can quickly determine which responses are overdue. In addition, patients sometimes call their primary care office to confirm the date and time of their appointment with a specialist. The spreadsheet provides a quick way to answer the patient's inquiry immediately, without retrieving the chart and searching for the referral documentation.
Both of these scenarios are routine within a primary care office, and using a well-designed patient referral form along with a tracking spreadsheet or an EHR report can be invaluable in reducing the rework that is required.
Ideally, one would like to have a fully automated process for collecting and using these data. However, this is not possible unless a complete EHR system has been fully implemented – ideally one shared by the primary care office and the specialist's office. The process described is a good way to achieve effective referral tracking when a practice has not yet installed a complete and sophisticated EHR system. It allows for “good enough” tracking and communication, and the ability to see trends in one's practice, without the cost of a full EHR implementation. Using a process like this will promote better patient care and help practices move closer to a patient-centered medical home model of care.
