
Tracking patient engagement is a key step to enhancing health and reducing costs.
Fam Pract Manag. 2016;23(6):21-24
Author disclosures: no relevant financial affiliations disclosed.
Active patient engagement is associated with improved patient outcomes.1 Health confidence is an easy-to-measure proxy for patient engagement that can lead to interventions that produce improved outcomes. The concept of health confidence and its implementation were introduced in a previous Family Practice Management article.2 You can measure health confidence by asking patients a single question, “How confident are you that you can control and manage most of your health problems?” Patients can respond using a numerical scale from 0 (not confident) to 10 (extremely confident). A score of 8 or more is considered ideal. Alternatively, patients could answer “very confident,” “somewhat confident,” “not very confident,” or “I don't have any health problems.”
Our group of five family physicians and four nurse practitioners and physician assistants decided to measure health confidence for one year, use it to guide interventions, and study the effects. This article describes what we learned.
Measuring health confidence
We identified 287 patients in our practice and recorded health confidence scores in structured data fields in our electronic health record (EHR). This allowed us to extract health confidence values recorded on certain encounter dates for patient populations we wanted to study.
Within the general patient pool, we identified a small cohort of 32 “at-risk” patients, which included individuals with high hospital utilization, poorly controlled chronic conditions, or some combination, who were willing to engage with the practice in focused care coordination. We measured the health confidence scores for this group even more regularly and systematically, and these patients received a range of interventions provided by a care coordinator. (See “Interventions for at-risk patients.”)
| Intervention | Intensity | Method |
|---|---|---|
| Assess health confidence | Low | Ask patient directly and record as structured data in electronic health record. (See visual aid and additional free health assessment resources at https://howsyourhealth.org.) |
| Define patient as belonging to “at-risk” population | Low | Identify patients with health confidence scores of less than 8. |
| Label chart of “at-risk” patients | Low | Flag patient record to identify at-risk patients as part of a cohort requiring enhanced services. |
| Perform medication reconciliation | Moderate | Perform medication reconciliation in person or by telephone regularly and after any hospital contacts. |
| Assess medication adherence | Moderate | Ask questions based on Morisky Medication Adherence Scale;1 record answers in structured data fields. |
| Perform enhanced previsit preparation | Moderate | Use a team approach involving nurses, care coordinators, medical assistants, etc.; ask about patient's goals for visit. |
| Engage office staff in focused, intensive outpatient care | Moderate | Create vision: What does improving health care look like? |
| Standardize panel management | Moderate | Develop flow maps detailing the care management steps to be performed during visits for patients with chronic diseases. |
| Use motivational interviewing | Moderate – High | Incorporate into patient interactions where appropriate. |
| Provide focused transitional care management | High | Contact all patients within 48 hours of discharge from emergency department or inpatient care. |
| Provide in-office care coordinator visit | High | Schedule for 15 minutes prior to office visit with provider. |
| Provide intensive chronic disease management | High | For example, implement asthma action plans, PHQ-9, and patient education, and refer to mental health resources as needed. |
One such intervention, motivational interviewing, became “usual care” for all of our patients after our clinicians and staff received formal, multi-session training to develop these skills. (To learn more, see “Using Motivational Interviewing to Promote Healthy Weight,” FPM, September/October 2016.)
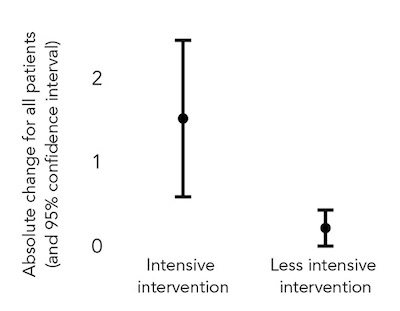
We measured changes in health confidence over a period of three to 12 months for two cohorts: the at-risk patients who received “intensive intervention” and the general group of 287 patients, most of whom received “less intensive intervention.”
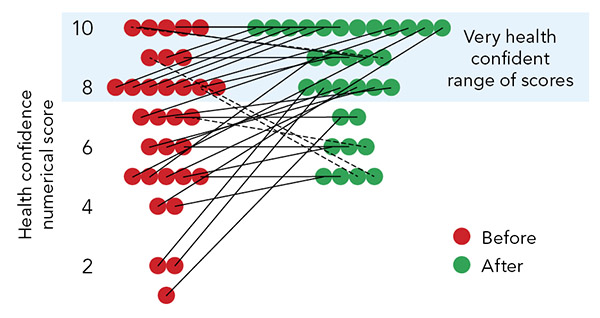
Among the 32 at-risk patients, only three recorded a decline in health confidence during the measurement period. (See “Change in health confidence among at-risk patients.”) Moreover, when comparing the change in health confidence among these at-risk patients with that of the overall 287 patients, most of whom received the less intensive intervention, the at-risk patients experienced a larger and statistically significant improvement in self-reported health confidence. (See “Change in health confidence by intensity of intervention.”)
CHANGE IN HEALTH CONFIDENCE AMONG AT-RISK PATIENTS
Health confidence scores among “at-risk” patients increased following a series of interventions. Scores of 8 and above are considered ideal.
CHANGE IN HEALTH CONFIDENCE BY INTENSITY OF INTERVENTION
Patients receiving a larger range of interventions aimed at improving their health confidence reported a higher increase in their confidence scores than patients who did not receive those interventions.
Benefits of higher health confidence
Several factors affect a patient's health confidence, including health status, socioeconomic stressors or supports, and the quality and usefulness of the health care provided. We did not provide all interventions to all patients in the at-risk group. Rather, we selected specific interventions based on the patient's circumstances at the time. This allowed the practice to direct scarce resources toward patients with the most potential to benefit from the interventions. The goal was to progressively increase patients' confidence in personal health care management, leading to improved health status and less use of hospital care.
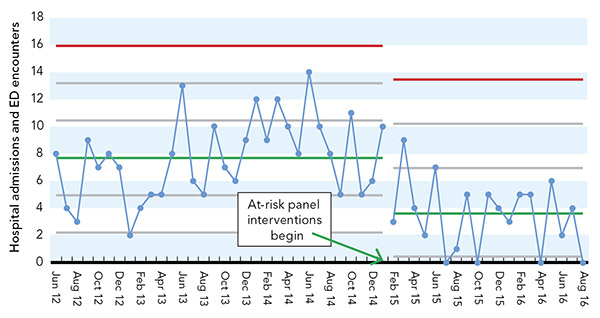
We found that improved health confidence led to lower use of hospital care. Our practice uses run and control charts to monitor performance over time in metrics important to the practice and to patient care. (See “Run and control charts.”) One chart showed an abrupt, statistically significant, and sustained decline in the number of hospital admissions or emergency department visits among our at-risk patients immediately after we deployed intensive interventions and discussions of health confidence among this population. (See “Change in use of hospital services.”)
RUN AND CONTROL CHARTS
White River Family Practice uses control charts as part of its Statistical Process Control (SPC) methodology to quality improvement efforts. We use inexpensive commercially available software to create graphs that differentiate significant change from common variation within the data. SPC tools are easily learned and are invaluable to providers wishing to move beyond simple “report card data displays” to understand whether process change has contributed to sustained improvement.
To learn more, try these resources:
Wheeler DJ. Understanding Variation: The Key to Managing Chaos. Knoxville, TN: SPC Press; 2000.
Carey RG. Improving Healthcare With Control Charts: Basic and Advanced SPC Methods and Case Studies. Milwaukee, WI: ASQ Quality Press; 2003.
CHANGE IN USE OF HOSPITAL SERVICES
Use of hospital services among patients belonging to the “at-risk” cohort showed a statistically significant decline following the start of health confidence interventions. The green center lines identify mean utilization before and after interventions began, and the red lines identify the upper control limit.
Our practice also found that simply asking patients how confident they were about self-management could change the dynamic of the office visit and improve the visit agenda. For example, one provider said that he used a patient's reported health confidence to adapt the content of the visit, the frequency of follow-up, and the type of follow-up (medical assistant telephone follow-up, engagement of the care coordinator, etc.). If time and setting permit, a physician could also use the patient's reported health confidence to develop a meaningful care plan (e.g., “What would it take to make you more confident?”).
We acknowledge that the study group was limited and that the statistically significant, sustained decline in hospital encounters we observed among this patient population may have been moderated by regression to the mean, the tendency of observations of a measure to approach the average over time. However, the results are suggestive. While further study involving a greater number of patients is necessary, others have observed a correlation between low health confidence and high emergency room use in larger patient populations.3
Adding health confidence assessment to your practice
The first, simplest, and least expensive step toward adding discussions of health confidence to your practice is to make it a vital sign that you routinely ask patients about and record in a structured field within your practice's EHR. This enables you to stratify populations in which low confidence translates to an increased risk for potentially avoidable high-cost care.
Next, designate one or more staff to act as care coordinators. These individuals need some clinical experience or training because, among their many duties, they need to ensure complete and accurate medication reconciliation, which is essential for addressing issues that arise when discussing health confidence. Medication reconciliation must be considered at every encounter with an at-risk patient population.
Third, develop motivational interviewing skills, which facilitate discussions with patients about important health issues beyond their immediate medical problems.
Last, track how patients' use of hospital services relates to their health confidence. Avoiding unnecessary high-cost hospital services is an obvious value to insurers. Our group has been able to use this data to advocate for higher payment.
Health confidence reporting and measurement can provide a wealth of benefits to the practice and the patient. Collecting the patient's health confidence rating as a vital sign is simple, inexpensive, and provides information that is immediately actionable. Improved health confidence correlates with improved patient health and reduced use of hospital services – strong arguments for employing this measure as a foundational metric of health care delivery and provider reimbursement.
