Your office staff can help normalize conversations with patients about critical care options.
Fam Pract Manag. 2022;29(3):10-14
Author disclosures: no relevant financial relationships.

The need for patients to document their critical care preferences through advance directives existed long before the COVID-19 pandemic. But the pandemic caused a sudden increase in procedures such as mechanical ventilation, often without family members present, which has driven home the importance of having these sometimes-difficult conversations with a trusted primary care clinician before patients are seriously ill.
Advance care planning (ACP) gives patients the information they need to create a legal document (sometimes called a “living will”) that outlines the care they want if they are unable to voice their wishes due to physical or cognitive disability. This includes naming a health care agent (HCA) authorized to make decisions on the patient's behalf, who can also be named in a separate medical/durable power of attorney document.
The most effective way to increase ACP completion in primary care settings is repeated face-to-face patient counseling by a health care professional.3 But it's not practical for physicians to do this alone in most practices.
However, there are a number of ways practices can leverage their EHRs and clinic staff to prep patients for ACP conversations and increase ACP completion rates. Our clinic created a team-based workflow and educational tools to encourage these conversations without adding clinician effort or cost.
Our workflow uses the EHR, the full clinic staff, and pre-visit waiting time to prime patients for ACP discussions, ensuring clinician time is used only for the complex, clinical aspects of ACP. Our educational tool helps patients understand how an HCA functions and what medical procedures should be discussed during ACP. Ideally, this results in patients completing a full set of advance directives, or at least legally identifying an HCA.
KEY POINTS
Developing a health care agent (HCA) patient education form can lead to more patients designating a trusted person to make health care decisions for them if they become incapacitated.
Engaging the whole care team in advance care planning (ACP) and HCA designation lightens the clinician's workload and enriches the jobs of other staff.
Making ACP/HCA forms a routine part of patient visits normalizes end-of-life care conversations and helps the clinic consistently document patient wishes.
IMPLEMENTING THE WORKFLOW
We recommend that clinics start by assessing their current ACP processes and resources. When our clinic did that, we found that our process usually depended on clinicians initiating the ACP discussion, often at a Medicare wellness visit, new patient visit, or annual physical, or when patients were in declining health or facing a terminal diagnosis. Clinicians said that ACP conversations felt forced and unnatural when the visit was about chronic disease or a minor acute issue such as a muscle strain. As a result, many patients were never approached about ACP or designating an HCA.
To overcome these barriers, we redesigned our workflow to reduce the clinicians' responsibility for beginning ACP conversations. Instead, staff now ask all patients to consider ACP/HCA documentation while they are waiting to meet with the clinician, and staff hand patients educational tools designed for this purpose. When every patient is asked about ACP/HCA documentation, it normalizes the conversation for patients and clinicians. Clinicians do not have to remember to add ACP documents to visits; they simply review the ACP paperwork already provided by staff and answer any questions the patient may have.
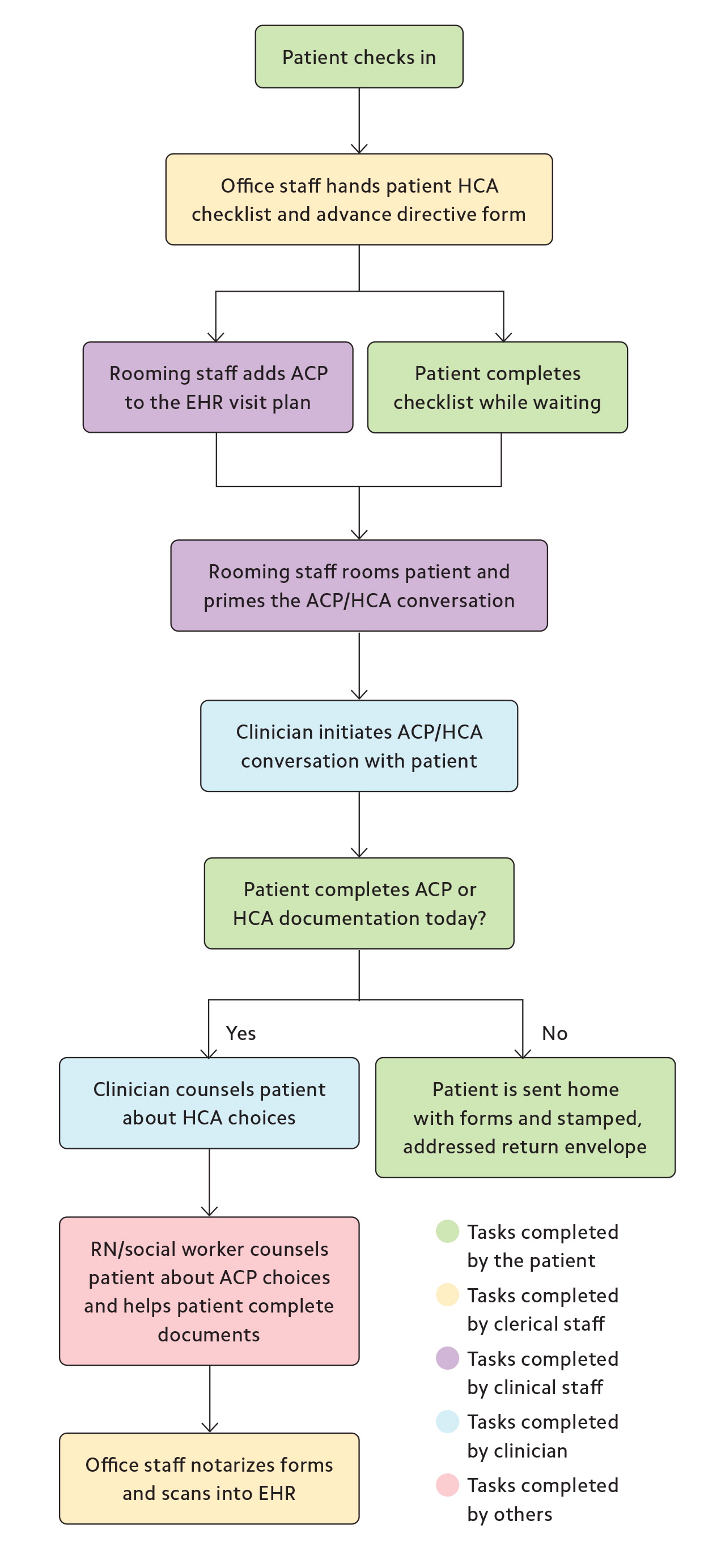
When patients want to spend more time considering their ACP choices after discussing options with a clinician, or when they need help completing the form, our clinicians make a warm handoff to clinic staff such as licensed social workers or registered nurses. This helps clinicians stay on schedule, while supporting patients at the pace they need individually. It's also enriching for staff. Providing patient education and guidance allows nurses and social workers to work at the top of their license.
Patients who are ready to complete a formal advance directive in the office can have it notarized onsite by our clinic business office staff. For those who need more time to think about the form or have discussions with their HCA, our clinic provides a pre-paid, addressed envelope to return the form. We have also designated a care coordinator to provide ACP/HCA support to patients over the phone.
Our process leverages technology in addition to the medical staff. Early on, we used our EHR to check the rate of ACP documentation for all of our patients age 65 or older and found it was only 53%. The clinic sent the remaining 47% of patients a letter with a short-form ACP explaining why this information was important to have on file and encouraging patients to reach out with questions and complete the paperwork.
We have also used the EHR to reduce clinician burden when it comes to documenting and billing for ACP. We added an ACP option to our problem list menu and developed several standardized dot-phrase EHR templates. These templates allow quicker documentation because clinicians can use a customized keyboard shortcut (e.g., “.ACP”) to create a pre-formed block of text and then fill in any blanks (see “Sample dot-phrase EHR templates”). Make sure your templates meet your state's legal requirements for advance directives.
Encounter notes support ACP billing, but adding data specifically to the EHR's ACP/HCA fields gives clinicians fast, reliable access to this information. For patients on Medicare, billing for ACP can occur multiple times annually, but the conversation must last at least 16 minutes. For Medicaid and commercially insured patients, ACP codes may or may not be covered based on contracts and state policies.4
SAMPLE DOT-PHRASE EHR TEMPLATES
.ACP
(Patient name) and I discussed their advance care plan preferences for ___ minutes, which include: [Y/N attempt resuscitation, (Do Not Resuscitate – DNR)], [Y/N intubate and ventilate, (Do Not Intubate – DNI)], [Y/N comfort care or life-sustaining care]. The patient's goals include: ___ ___ ___ ___ ___. I reminded patient to talk with their health care agent, (HCA name), about their care goals. Note reflects patient's free will and care goals as expressed to me.
.HCA
(Patient name) and I discussed advance care planning today. They named (HCA name) as their health care agent. Reminded them to discuss their care goals with (HCA name).
.ACPintro
(Patient name) and I discussed advance care planning today. They are not yet ready to name a health care agent or define their advance care goals. Sent them home with ACP/HCA planning materials.
DEVELOPING ACP/HCA TOOLS
Our new workflow required us to develop several ACP/HCA tools.
An HCA patient education form/checklist. This document includes a basic description of an HCA, four questions to prompt patients to think about who they prefer to be their HCA and what conversations they should have with that person, and a section to indicate what action they would like to take today (see “HCA patient education form”). We print this checklist on blue paper so it stands out from other forms. It can be added to the EHR as a pre-visit form (which is particularly useful for telehealth visits, when forms cannot be handed out prior to the visit). Having the pre-visit form in the EHR allows the clinician to review it during the visit and then pass it along to clinic staff to send the patient a paper form for the next steps (e.g., signing and notarizing).
| Selecting Your Health Care Agent | ||
|---|---|---|
| A health care agent is a person you name (usually a family member or friend) who will make medical decisions for you if you are not able to. Your health care agent will make decisions about your medical care, including your medications, tests, surgeries, and end-of-life care. You can complete the attached form to name your health care agent. | ||
| Do you know which person you would like to make medical decisions for you if you become unable to do so? | □ Yes | □ No |
| Have you told that person that you have chosen them? | □ Yes | □ No |
| Have you talked with that person about what is most important to you? | □ Yes | □ No |
| Have you told your doctor which person you have chosen to make these medical decisions? | □ Yes | □ No |
| □ I am interested in completing the health care agent form today or discussing this with my clinician. □ I already completed my health care agent or advance care plan. □ I am not interested at this time. □ Other: __________________________________________ | ||
A short-form advance directive. Our clinic started with a short-form advance directive from the Twin Cities Medical Society initiative Honoring Choices Minnesota5 and then supplemented it with a few items specific to our clinic. We suggest that you look for a similar form available for your state, because each state has different legal requirements, including what should be specified in the advance care plan (e.g., mechanical ventilation, feeding, and treatment interventions) as well as requirements for witnesses and notarizing.
ACP scripts. We provided scripts to front-desk staff to help them explain to patients what these forms are and why we ask all patients of a certain age to complete or review them. We also developed scripts that clinicians and staff can use when having ACP conversations with patients (see “ACP conversation prompts”). During training sessions about ACP requirements, clinicians and staff paired off to practice initiating ACP conversations.
ACP CONVERSATION PROMPTS
Introducing the concept of advance care planning:
“Have you ever completed a living will or advance directive?”
“Would you like to talk more about your wishes regarding your health care?”
“Have you ever thought about planning for future health care decisions?”
“Advance care planning is a process we encourage all adults to do throughout their lives. You can update your directives as you grow older or if your health changes.”
Providing education on advance directives or POLST:
“An advance directive is a way for you to write down who you would want to speak for you if you could not speak for yourself. It also allows you to include specific wishes for future health care decisions and express what is most important to you.”
“Physician Orders for Life-Sustaining Treatment (or POLST) is an extension of your advance directive. It transfers your current wishes for your health care into doctor's orders that follow you wherever you go. It is especially important for patients with serious illnesses.”
Discussing the selection of a health care agent:
“Have you ever thought about who you would want to speak for you for health care decisions if you were unable to speak for yourself?”
“Have you discussed your health care wishes with this person before?”
“Do you think this person would respect your wishes and preferences?”
Exploring patient's values, beliefs, and goals:
“Have you ever been involved in caring for a loved one who was very sick? What did you learn about your own wishes for your health care from that experience?”
“What does living well mean for you?”
“Are there any medical treatments that you feel you would not want?”
“If you lost the ability to recognize or interact with loved ones, how would you want to be cared for?”
“Do you have any religious or cultural beliefs that impact your wishes for your health care?”
Encouraging next steps:
“We are committed to helping you with advance care planning and have a variety of options for you to choose from (group class, staff with ACP expertise, consult/referral, hotline number, etc.). What would be most helpful to you at this time?”
Providing directions when a document is completed:
“Give a copy to your health care agent and other doctors/hospitals as appropriate.”
“Keep your POLST form on your refrigerator or with other important medical paperwork that can be easily located by paramedics.”
“Review and update your forms every 10 years, or when anything changes in your health, relationships, or wishes.”
HOW IT WORKED FOR US
During a pre-COVID-19 pilot of our new workflow, we were able to add HCA/ACP documentation for 56 patients (17%) to the EHR. Of the 335 patients we approached (all age 50 or older), 122 patients (36%) reported already having a documented HCA. Rather than excluding them, the team asked all patients to confirm their documentation and choices, because over time HCAs may change due to death, divorce, or other factors. Universal collection also makes the process easier for the front-desk staff. Every patient over age 50 gets the paperwork, so staff do not have to alter the process for each patient. While this may seem repetitive to patients who visit the clinic regularly, it helps normalize the ACP/HCA process.
Our clinicians reported using the EHR dot-phrase templates in 57% of visits that included ACP and the conversation scripts in 91% of visits. Clinicians said the forms were short and easy for patients to understand, the pilot program did not create much extra work, and the new workflow should continue as a regular clinic process. Clinic wait times and visit lengths did not grow, in part because patients had the option to take the paperwork home to complete later or schedule a future visit to talk about ACP exclusively (with the knowledge that this would incur an additional co-pay).
When COVID-19 moved many visits to virtual in 2020, we encountered some challenges. Online visits lack wait times during which staff can introduce the ACP documents to patients, and it is often not possible to hand off patients to other professionals in the same e-visit. Clinicians could still initiate ACP conversations with patients, but virtual visits made the documentation process more complex. We had to send patients the forms either by mail (along with the pre-paid, addressed return envelope) or through the patient portal. This also meant patients had to find their own notaries. When completed forms arrived through the mail, clinic staff had to scan copies into the EHR and add notes in the HCA field.
Still, we see a role for this ACP documentation process for a broad age range of patients, especially as clinics return to more in-person visits. We are planning to have staff add annual checks for ACP/HCA documentation and accuracy for all patients 18 and older, just as we do currently for address, phone, and other vital contact information.
The over-arching lesson we learned is that when we involve the whole care team in ACP, we can improve patient and employee satisfaction as well as quality of care.