
These six lessons can help practices improve both the quality of care for refugees and physician satisfaction in caring for them.
Fam Pract Manag. 2022;29(4):15-18
Author disclosures: no relevant financial relationships.

Refugees are provided with resources such as case managers, social workers, financial support, and housing immediately upon arrival in the U.S., but these services are generally discontinued before the refugees become fully self-sufficient.3 Refugees also often have limited health literacy and English proficiency and acculturation issues, along with complex or multiple medical problems, including tropical and infectious diseases and mental health needs.1,3 U.S.-trained physicians are often not equipped to deal with these issues in a typical 15-minute office visit.1–3 The result is an underserved patient population that experiences significant health disparities and poses unique challenges to the delivery of primary care.1 The special care needs of refugee patients were outlined in a previous FPM article.3
In our clinic, more than 20% of patients are refugees, yet when we surveyed the physicians about how well they felt they addressed refugees' health care needs, they rated their care as only 5.5 on a 10-point scale (1 = terrible and 10 = excellent) compared with 7.3 for general patients in the clinic. In response, we created a refugee-specific clinic to better serve these patients and their complex needs in our practice. The refugee clinic is held two half-days per month, and we can see six patients per session, which is sufficient for our patient population. It operates within our family medicine residency's regular clinic facility and has been in operation for almost five years.
Here are six lessons we've learned about how to improve both the quality of care for refugees and physician satisfaction in caring for them by using the model of a refugee clinic.
KEY POINTS
Refugees' unique needs, including limited health literacy and complex or multiple medical problems, can be challenging to address in a typical 15-minute office visit.
Establishing a refugee clinic within an existing primary care clinic can help practices address the most complicated cases through longer visits.
In the authors' practice, after establishing an integrated refugee clinic, physicians' ratings of how well they felt they were treating refugees improved from an initial score of 5.5 to a score of 8 on a 10-point scale.
1. Assemble the right team. The refugee clinic team starts with a lead physician who has expertise in refugee care. We have two physicians who take turns serving in this role. They gained expertise in this area by working with refugee patients and completing continuing medical education related to the care of refugees. Any physician who has the passion and desire to take better care of refugees can fill this role, even in a small practice.
In addition to the lead physician, our team also includes the following:
- A dedicated nurse and a dedicated front-desk staff member (both staff members also work in the regular clinic but are always assigned to the refugee clinic on the days we hold it),
- Two residents,
- Two medical students,
- An attorney who is part of our medical-legal partnership4 and helps with housing issues, legal issues, and paperwork (such as N-648 forms, which exempt refugees with physical or mental/developmental disabilities from having to pass civics and English testing for citizenship naturalization),
- A social worker who does counseling and connects patients to community resources.
On occasion, we also include pharmacy and public health students and a case manager from the local refugee resettlement agency. The public health students work on translating educational materials and identifying local resources for our refugees. The pharmacy students help with medication reconciliation, education on medications, and automatic refills. We have patients bring all their medication bottles to every appointment, which has been tremendously helpful to the pharmacy students and us, as most patients are not sure what they are taking or why.
While this level of staffing may not be available in all practice settings, resources are available in many communities that could make them available to practices on an as-needed basis. For example, if you work in a health care system, dedicated nurses, front-desk staff, pharmacists, and psychologists may be available to participate in a monthly or biweekly refugee clinic. For independent practices, physicians can reach out to local refugee agencies and community partners to see if they have people who can work with the team during these special clinic sessions. We have found that consistency in the team is important and helps with the care of these patients with very complex needs.
2. Anticipate no-shows and appointment barriers. When we started the refugee clinic, we had a high no-show rate (about 50%). We decreased it to less than 25% by having the front-desk person call all refugee patients to confirm their appointments. During the call, patients are asked about barriers to getting to the appointment (e.g., Do you foresee any issues getting to your appointment? Do you have a ride?). If a barrier is identified, the front-desk person helps resolve it (e.g., calling Medicaid to help arrange a ride or calling the case manager). If barriers cannot be resolved, the appointment is rescheduled.
3. Do essential prep work to ease patient visits. Before we see patients in the refugee clinic, we start with a team huddle, reviewing each patient chart to identify gaps in care, including needed immunizations and preventive services. We also review the patient's initial intake form and the last clinical notes and labs. Based on this review, we develop a care plan for the patient's visit and assign tasks to different team members.
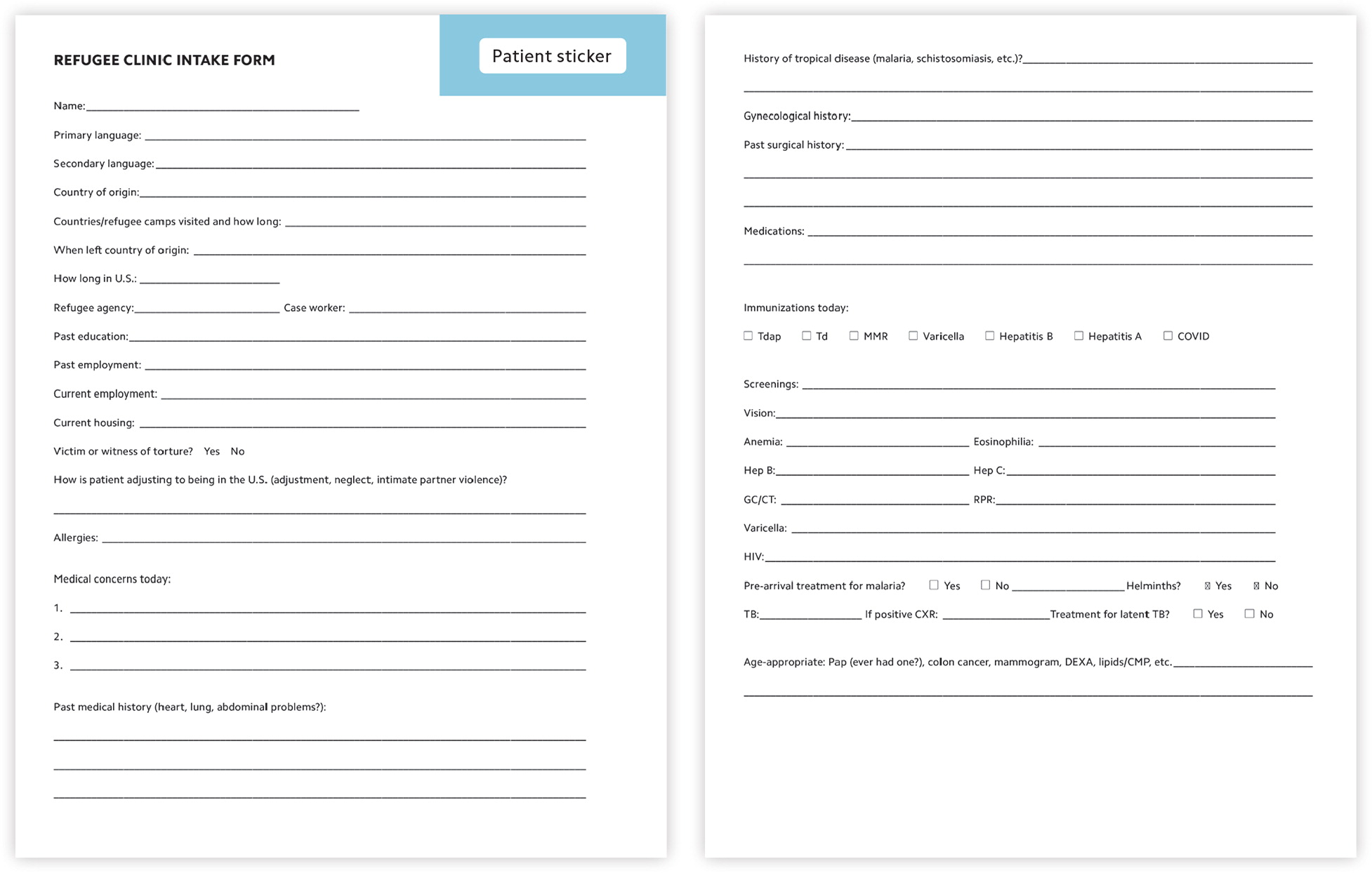
Each patient is scheduled for a one-hour appointment. At a patient's first visit, we complete a specialized intake form that has been adapted from several sources (see below). It is typically completed by the assigned medical student with guidance from the attending. In a practice without medical students, the dedicated nurse or social worker provided by the health system or local refugee organization could be trained to do this. We do the intake verbally so that the language of the form and patient literacy are not barriers to its completion. Our electronic health record (EHR) carries forward critical information from the intake form, but it could also be scanned into the EHR if needed.
4. Arrange for translation services. Since our patients speak a variety of languages, we often use interpreter services for translation during visits. We find that using phone interpreters, rather than video interpreters, works much better for patients, especially when discussing sensitive topics. Many of our patients seem more reserved with video interpretation but disclose information more freely when we use phone interpretation. We now use phone as our default method unless the patient prefers video.
5. Focus on the more complicated cases. Many of our refugee patients are seen in the general clinic, and only the most complicated cases are referred to the refugee clinic. Common issues we take care of in the refugee clinic are first-time Pap smears, new HIV-positive diagnoses, latent tuberculosis treatment, severe post-traumatic stress disorder, parasitic diseases, undifferentiated illnesses, medication reconciliation, and complicated paperwork completion (especially N-648 forms), as well as caring for those who have multiple complicated medical issues. The goal of the refugee clinic is to work on the most complex problems and then get these patients back to their regular physician in the general clinic. Since we operate in same facility as our regular clinic, we communicate with the patient's primary care physician through EHR messaging. Some patients with very complicated issues end up continuing care in the refugee clinic.
6. Track your time. Most of these visits can be billed using an E/M code plus a prolonged services code that reflects the additional work required. For prolonged services provided before and/or after direct patient care, CPT code 99358 can be billed for the first hour along with the E/M code, and code 99359 can be billed for each additional 30 minutes. For prolonged services involving direct patient contact, code 99417 (G2212 for Medicare) can be used for each 15 minutes of prolonged services beyond the usual E/M service. Report this code only with code 99205 or 99215 when time is used as the basis of code selection. Start and stop times must be documented in the note to justify these codes.
A MODEL CLINIC
Many clinic models address the initial care of refugees when they first arrive in the U.S., but few provide ongoing care for refugees with complicated issues within an established clinic. Unique features of our model include the specialized care team, the length of appointments, and seeing patients within their existing primary care clinic. We believe that this approach can serve as a model for any clinic that wants to better serve their refugee patients.
We surveyed our physicians after we established the refugee clinic, and their rating of how well they felt they were treating refugees improved from the initial score of 5.5 to a score of 8 on a 10-point scale.
Being able to provide comprehensive, individualized care tailored to the specific needs of our refugee patients has been beneficial for patients and rewarding for physicians. Furthermore, having integrated clinics that address the specific needs of refugees can go a long way to decreasing health disparities in this population by providing better and more comprehensive care and increasing communication between the physician and patient.
