This supplement is sponsored by the American Academy of Family Physicians.
Fam Pract Manag. 2022;29(5):17-22
The goals of the Triple Aim in health care of enhancing the patient experience, improving population health, and reducing costs are noble pursuits. However, those goals can only truly be realized when we focus on a fourth goal of improving the work life and well-being of the care team. These four goals are collectively called the Quadruple Aim of health care.1,2 This fourth additional and necessary goal reframes how we accomplish the Triple Aim and requires leadership from family physicians.
While family physicians are often leaders to our patients and colleagues, many have no formal leadership training.3,4,5 In fact, many learn in medical education the ethos that leading a health care team requires an unrestricted, personal sacrifice to patient care—even when our sacrifices result in burnout, suicide, early retirement, and reduced quality of care to those same patients.6,7
To break that ethos in family medicine and achieve the Quadruple Aim of health care, the specialty must train its physicians to be leaders in quality improvement and performance improvement (QI/PI) activities. These activities can have challenges, such as convincing staff and leadership that there is a need for improvement and the solution you’ve chosen is the correct one, lack of staff engagement, and adequate data collection and monitoring systems.8 Despite these concerns, QI/PI activities are essential to successful practice transformation and, ultimately, improved work life and well-being of the entire care team.
Leading Physician Well-being (LPW)
To improve physician well-being and develop the leaders of now and the future, the AAFP’s Leading Physician Well-being (LPW) certificate program was developed in 2020 as a yearlong discovery process for family physicians with three goals:
Leadership development,
Well-being advocacy on personal and system-levels,
Performance improvement skills to create positive changes in medicine.

Learn more about the AAFP’s LPW program on our website. To receive a notification when the next application process opens, please email lpw@aafp.org.
The certificate program of education includes more than 70 continuing medical education (CME) hours (including AAFP PI hours) and completion of projects pre-approved for American Board of Family Medicine (ABFM) Maintenance of Certification (MOC) PI points. More than 200 family physicians have participated in the AAFP’s LPW certificate program, which is entirely funded by a grant from the United Health Group.
This supplement examines the three goals of the LPW certification program (leadership development, advocacy for well-being, and performance improvements) and offers tips and tactics for each goal, as well as provides four steps (assess, strategize, accomplish, and celebrate) to help begin your journey to achieving the Quadruple Aim of health care.
The ABFM’s PI requirement for MOC has been enhanced, so simple office-based projects qualify for PI points. This ABFM Self-Directed Clinical Performance Improvement briefer and ABFM Self-Directed Clinical Pathway: Instructional Guide video provide overviews about satisfying PI requirements for continuing certification for physician practices of all types and sizes.
Achieving the Quadruple Aim Through…
…Leadership Development
Developing leadership skills among family physicians can help achieve the Quadruple Aim as you learn to lead by influencing others and implementing positive changes in your practice and community. When thinking about physician leadership development, the following tips are important to remember and can guide your efforts:
Physicians are leaders. Family physicians’ skills, patience, training, and abilities are similar attributes that make great leaders in other disciplines. Don’t undervalue your power, influence, and talent.
Leaders don’t always have the best ideas and shouldn’t do all the work themselves. Successful leaders learn that the best traits for success include motivating staff, partnering with other leaders, listening to feedback, and supporting their teams through their successes and failures.
Study leadership development trends and tools. There is an abundance of leadership training available. Ask the leaders you admire about the books, podcasts, YouTube channels, journals, conferences, TED Talks, and other resources they consume. Successful leaders are always learning. Study how and what they learn and model them.
Leaders learn by doing. It doesn’t matter how much you study if you’ve never led or strived to become a positive force for change. Not everyone’s personality lends itself to a bold and commanding leadership style. If you are a naturally quiet person, now is the time to lead quietly and learn skills of boldness. If you are a naturally bold person, consider what you can do to draw some of your more reserved colleagues into your work.9
…Advocacy for Well-being
Well-being is not just a buzzword. It is a practice and a way of life for many. And it is essential in order for you and your practice to achieve all four goals of the Quadruple Aim. When thinking about personal and system-level well-being, the following tips are important to remember and can guide your efforts:
You are not the problem. While there are many individual skills we can learn to support our well-being, the systems we work in strain our natural resilience. While working toward system-level changes, here are some individual skills or practices to bring balance to your experience as a physician:
– Take slow, deep breaths. A single, slow, and deep abdominal breath has been shown to help reset your sympathetic/parasympathetic system and prepare you for the encounter or challenge that awaits you.10
– Embrace your happy place. This is not just a cliché. The amygdala, your emotional processing center, is a terrible multi-tasker. Spending a moment recalling something amazing in your life can change your frame of reference for the task ahead.
– Gratitude works. Studies have shown that a few moments of daily reflection of gratitude can have a similar effect on your mood as taking a selective serotonin reuptake inhibitor (SSRI).11,12
– Practice what you preach. Regular exercise, attention to relationships, spiritual development, hobbies, leisure activities, spending time outdoors, and vacation time shouldn’t only be prescriptions for better psychological and physiological functioning for our stressed-out patients.13 It also applies to those who provide care.
Well-being is achieved one step at a time. Some physicians will experience a major life change that leads to their well-being. However, most physicians find that steady, incremental change is rather successful. Small efforts to improve individual and care team well-being and create a culture shift in your practice include spreading continual gratitude to one another, establishing strategies and protocols to make tasks less burdensome, developing a well-being task force, and incorporating physician well-being as a topic on board agendas and when selecting executive leaders.
Don’t go it alone. Physicians who prefer to go it alone can burn themselves out on any project, including well-being projects. There are plenty of AAFP and other resources to help physicians and their care teams positively impact their own well-being and the well-being of their workplaces, communities, and health systems. Seek these out and share them with staff and colleagues.
Healthy workplaces create healthy patients. If you aren’t already doing it, right now is the time to start discussing well-being issues with the decision makers in your health system and community. Many health care decision makers (e.g., physician leaders and non-physician leaders in areas from nursing and other specialties to human resources and executives) are looking to engage physician leaders practicing in clinics. They are interested in physician satisfaction and well-being for many reasons, including improving the bottom line. Physician satisfaction and well-being decrease the costs of physician recruitment and retention, improve the quality of care, lower the cost of care, and reduce staff turnover.14,15
The AAFP Physician Health First website contains information and resources to support physician well-being, including resources about creating a culture of well-being, increasing joy in practice, practicing self-care, and suicide prevention and emergency help.
…Performance Improvement (PI)
Health systems and medical practices often focus PI efforts around high-critical areas of care or administration, such as clinical outcomes, patient experiences and satisfaction, and organizational costs. These efforts can fall short of their desired outcomes as one-off projects if they’re not part of an ongoing strategic effort to improve the overall infrastructure or practice operations.16 When thinking about QI/PI, the following tips are important to remember and can guide your efforts:
QI/PI projects are not research. Physicians often think about QI/PI activities from a research mindset and avoid them. Instead, they should view them through a Plan-Do-Study-Act (PDSA) lens. A PDSA is a structured method to implement, test, and study a change effort.17 A well-planned PDSA project can take as short as a single day to complete and yield significant benefits for the care you and your staff provide.
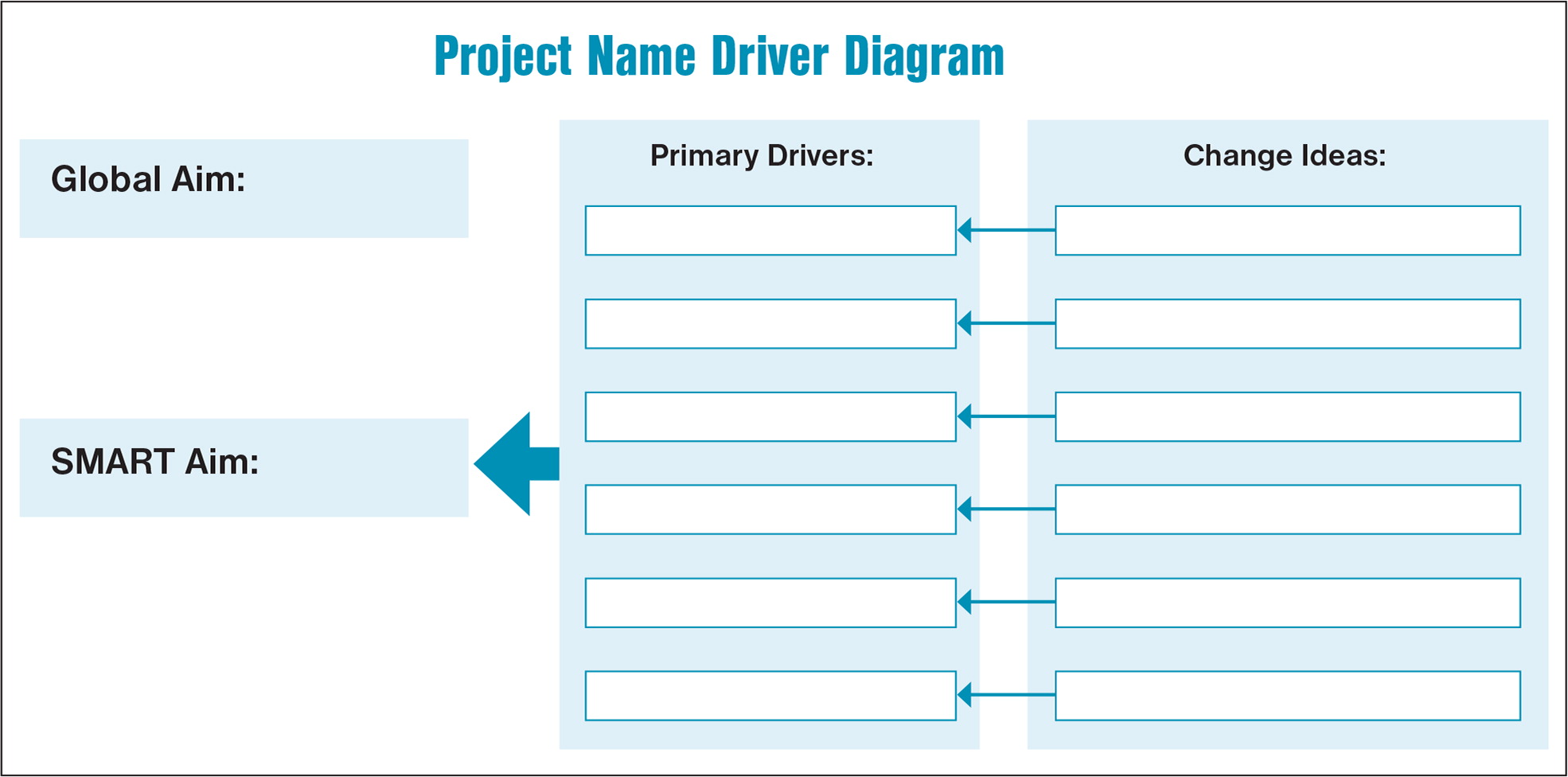
A major QI/PI project consists of a series of small projects that can lead to a single aim. An aim and driver diagram (see Project Name Driver Diagram below) can help you create a series of manageable steps to achieve your ultimate goal (called ‘Global Aim’ in the graphic below). One way to structure your aim or goal is to use the SMART pneumonic (Specific, Measurable, Achievable, Relevant, Time-bound).18
Get credit for your work. Many physicians are reluctant to start a QI/PI project because they envision the project can require significant time, effort, and resources. That is not always true, and you can even receive credit for smaller projects.
Example of a Single-day PDSA Project
Plan – A practice’s influenza vaccination rate is poor. Clinicians often forget to offer it at the beginning of a patient visit. For example, the practice only immunized five of 25 eligible patients in a single day. They ask themselves, “what if we post a note at check-in stations or in our electronic health record (EHR) reminding clinical staff about administering the influenza vaccine to all eligible patients?”
Do – Post a large sign on the wall next to the weigh-in station and/or a note in all eligible patients’ EHR records reminding staff to check the patient’s influenza immunization status and offer the vaccine to all eligible patients.
Study – Once this process is implemented, study the results. This practice found that after implementation, within one week, they had an all-time high for a single day of administering the influenza vaccine to 23 of 27 eligible patients. Patient and clinician feedback indicated that the sign on the wall (for patients and clinicians) and the EHR note (for clinicians) were needed reminders to offer and administer the shot.
Act – Leave the sign and EHR note as part of routine protocols for the practice and consider the same PDSA project for the COVID-19 and other routine vaccines.
Physicians striving to achieve the Quadruple Aim of health care should always be thinking about ways to positively impact their job satisfaction, workplace culture, care processes, well-being, local communities, and care systems. Many of us have limited opportunity and resources and may only be able to implement one or two of these changes at a particular time. For others in positions of influence, they could affect several changes simultaneously, building them into existing programs that positively impact physicians, staff, and patients. Wherever you are in the transformation process, the time is now to start making changes to achieve the Quadruple Aim in your practice, health system, and community. You might be asking, “where do I begin?” Well, with the first step, of course.
Steps Toward the Quadruple Aim
As the saying goes, the journey of a thousand miles begins with a single step. We’ve outlined some tips and tactics to work towards the goals of the LPW program as you strive to achieve the Quadruple Aim. Now, we’ll present four steps to take as you embark on your practice transformation journey: assess, strategize, accomplish, and celebrate.
Step 1: Assess
Carve out time for you and your team to conduct a simple needs assessment of your workplace. Begin by discussing some broad questions: What is our practice doing well? What areas can we improve upon? Next, ask yourself and your team the following specific questions:
Are we happy with our workplace culture? Which aspects should we eliminate, and which should we keep and improve upon?
Do we leave for work in the morning feeling exhausted or uninspired? Why or why not?
Does our workplace allow us to be the physician, nurse, office staff member, etc., we envision for ourselves? Think about the personal statement you wrote in medical school. Are you fulfilling that statement?
Are we doing our best for our patients who trust us with their care?
What other power structures or influencers can we leverage to help us impact positive change for our patients and community?
What are a few “easy wins” we can implement to help us all be more joyful in our work? Why haven’t we implemented these changes, and how can we accomplish them?
What is the greatest challenge I/we face every day?
Step 2: Strategize
Ask for ideas from all team members in your workplace—not just other physicians. An office manager, receptionist, medical assistant, nursing director, or other team members may be eager to help and have great ideas for change by viewing issues through a non-physician lens.
Openly communicate what you’d like to accomplish and why. This will build grassroots momentum, identify additional partners, help you see blind spots in your ideas, and give you time to think about your approach to change.
Leverage assistance from others when and where you need it. You may need financial assistance for some change ideas. Where will those finances come from? For other ideas, you may need the influence of upper-level management. Who in your organization will need to approve a change idea or use their influence to make change happen?
Step 3: Accomplish
Do something! Small interventions can often reap huge benefits in the well-being of you and your team. Don’t assume that only a massive, multi-faceted project can create meaningful change. You’re not going to solve all your issues with one project. Start simple and do a couple of small projects that give you a series of easy wins. Whether for good or bad, inertia is a powerful force. Building upon your successes will help refine your strategy, focus, leadership, and PI skills.
Step 4: Celebrate
Celebrate even your small victories and learn from failures. Remember, that’s what the PDSA cycle is all about—changing, reassessing that change, and repeating the process. Assess your quantitative and qualitative data to motivate, challenge, and stimulate further positive change for your team and culture. If a change project fails, that’s okay. Ask yourself why it didn’t work, learn from the experience, and move on to another idea. When something succeeds, celebrate and publicize that success…ALWAYS. Show gratitude to those who work alongside you. Use every win to lead you to the next thing you can positively impact.
These steps will facilitate success in practice transformations that will ultimately help your team achieve the Quadruple Aim of health care. Most importantly, your personal and professional well-being will improve as you transform your practice into one where you find joy and satisfaction in practicing medicine. The skills you attain along the way in this change journey will allow you to lean into your leadership abilities and be a role model to your patients, community, and the specialty of family medicine.
The AAFP Leading Physician Well-being Certificate Program is made possible through funding by the United Health Foundation.