
To achieve further progress in the shift from volume to value, payment models must be consistent with certain guiding principles.
Fam Pract Manag. 2023;30(1):5-7
Author disclosures: no relevant financial relationships.
The call for the movement “from volume to value” in health care has resounded for many years, but progress toward a payment system that recognizes and rewards value — especially for primary care — has been slow.
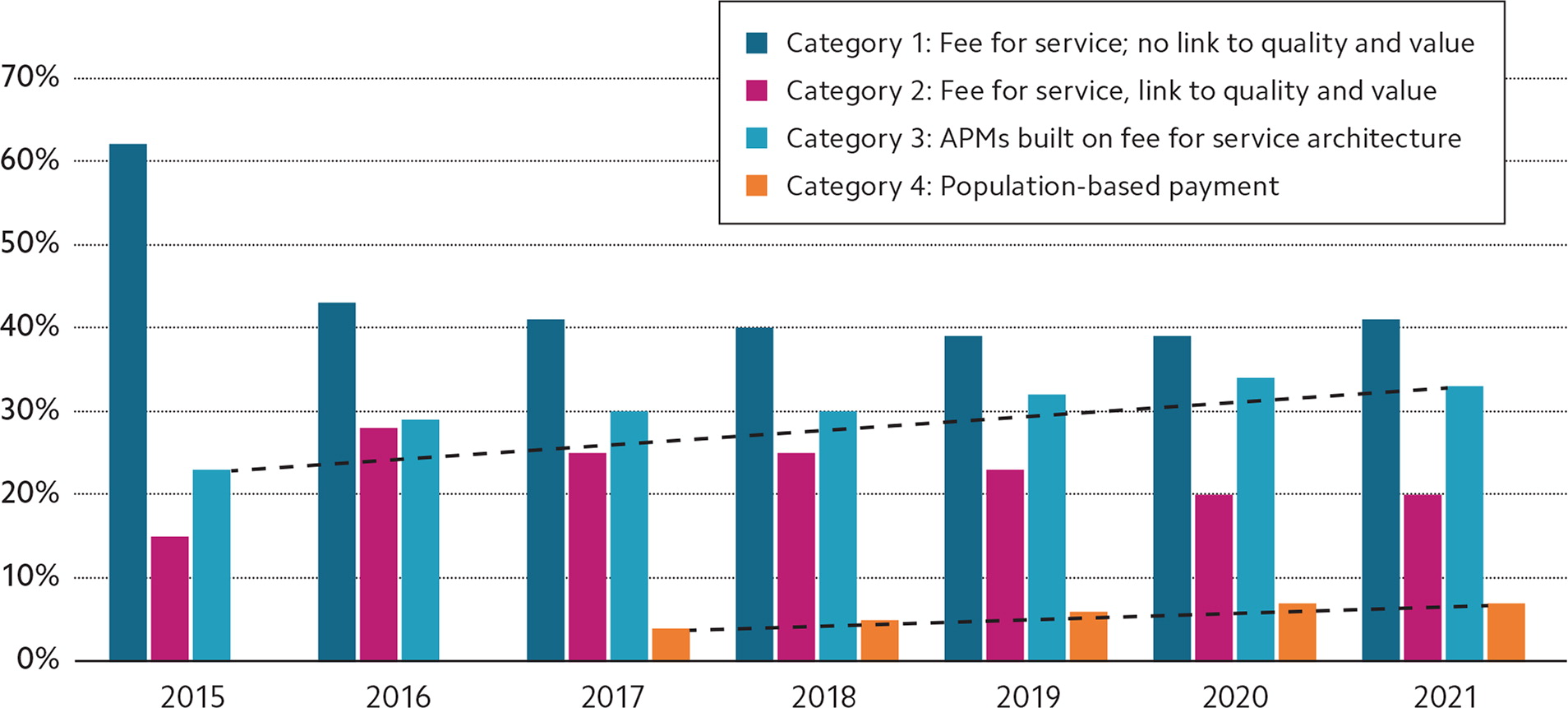
The Health Care Payment Learning and Action Network (HCPLAN) created a framework for assessing payment progress across commercial payers, Medicaid, and Medicare (traditional and Medicare Advantage). In its 2022 report based on 2021 data, 41% of payments were still in fee for service (FFS) with no link to quality, 20% of payments were in FFS with some link to quality, 33% of payments were in alternative payment models (APMs) built on FFS architecture, and just 7% of payments were made in the most advanced APMs that rely on shared savings or risk, bundled payments, and other population-based payments.1 For context, in 2015, 62% of payments were in FFS with no link to quality and 23% were in some type of APM. (See the graph below.)
We are making progress, but not nearly fast enough or at a scale large enough to meaningfully advance toward achieving the quadruple aim for health care — improving the work life of clinicians and staff — in addition to the original aims of improving the patient experience and health of populations while decreasing the cost of care.2 Further real progress from a primary care perspective will occur when APMs implement value-based payments consistent with certain principles.
WHY VALUE-BASED PAYMENT IS NEEDED
While FFS may continue to work as payment for very discrete services common in highly specialized care, it does not recognize the importance of teams or the broad range of services necessary to deliver comprehensive, continuous, whole-person primary care — much of which is not visit-based and not easily captured or paid under FFS. To adequately support primary care's unique role in caring for the whole person, payments need to shift away from the predominant reliance on FFS toward prospective payment sufficient to support a comprehensive array of primary care services delivered by physicians and care teams. One study estimated that more than 60% of a primary care practice's revenue needs to be prospective to sustainably support comprehensive, team-based primary care.3
A critical review of how evolving payment models influence primary care and its impact on the quadruple aim also identified prospective payment as the approach best suited for primary care because, when sufficiently funded, it supports a more comprehensive, team-based approach, including care the team provides outside of a “visit,” which is generally not readily captured and paid under FFS.4 The teams might also include a broad range of non-physician members such as social workers, community health workers, patient navigators, medical assistants, behavioral health specialists, pharmacists, nutritionists, and others. Capturing their work often requires significant coding knowledge and documentation to qualify for FFS payment, if it is eligible at all.
GUIDING PRINCIPLES
As value-based payment programs are designed and implemented, they must include key features to support the kind of advanced, comprehensive primary care that is the hallmark of family medicine. To that end, the AAFP has adopted Guiding Principles for Value-Based Payment from a primary care perspective.
The principles state that predictable, prospective payments should generate revenue streams that are sufficient to support comprehensive, patient-centered, high-value care delivered by teams. Performance evaluations should align across payers and focus on a limited number of meaningful measures that matter to patients. Benchmarks used to evaluate financial impact should recognize and reward year-over-year improvement as well as sustained high performance over time. And physicians and care teams should receive timely and actionable information to provide comprehensive care to their patients without incurring unnecessary administrative or financial burdens. (See the full list of principles below.)
These principles inform the AAFP's advocacy and stakeholder engagement efforts. Their application by those who are designing and implementing APMs built on value-based payment rather than a FFS architecture will help ensure primary care physicians receive the kind of value-based payment that will support them, their care teams, and their patients. It is up to all of us — those who provide primary care and those who advocate for those who do — to see that this happens.
AAFP GUIDING PRINCIPLES FOR VALUE-BASED PAYMENT
Family physicians deliver most of the primary care in the U.S. It is essential that they and other primary care physicians take a leadership role in the development of policies and practices that facilitate movement away from fee-for-service and toward new advanced primary care payment models along with other key stakeholders, such as purchasers, union trusts, and government (federal and state) agencies responsible for U.S. health care spending.
These principles are intended to be responsive and adaptable to the changing environment and settings in which family physicians work. We encourage others to use these principles with the understanding that they must be applied in ways that are:
- Responsive to community needs, preferences, and resources,
- Adaptable to different practice organizational models, structures of care, and physician specialties,
- Inclusive of individual patient preferences and socio-cultural backgrounds,
- Sensitive to differences in adoption of health information technology while encouraging its effective spread and connectivity.
Value-based payment is designed to support collaborative partnerships between patients and physicians that include the four key functions of primary care (first-contact access, comprehensiveness, coordination, and continuity), which are essential to meeting the goals of improved quality and reduced health care spending. As more AAFP members transition to providing value-based care, these principles are intended to guide the design and implementation of value-based payment models, which support a health care system grounded in strong primary care that improves health outcomes, contributes to eliminating inequities, and reduces future health care spending.
The success of these principles is highly dependent on alignment across payers. Value-based payment models are unlikely to work if only a small subset of a practice's patient population is included. Covering just a portion of patients with value-based payment while the balance remains in traditional fee-for-service does not provide the level of prospective payment needed to invest in building advanced functions of primary care required for excellent population management.
Principles:
Value-based payment (VBP) models should be aligned across payers and provide predictable, prospective revenue streams as a foundation to sufficiently support comprehensive, longitudinal, patient-centered, high-value care in addition to performance incentives that reward improvement as well as sustained performance against financial and quality benchmarks. Within practices and other health care organizations, individual physicians should share in the financial rewards that accrue from their performance.
Methodologies used to determine the patients for which physicians and care teams are held accountable must prioritize existing patient-physician relationships over less reliable claims or geographic methods while ensuring physicians and primary care teams have reliable, timely information about the patients for whom they are held accountable.
Risk-adjustment methodologies should incorporate clinical diagnoses, demographic factors, and other relevant information such as social determinants of health without exacerbating health care disparities or expanding the administrative burden on primary care practices. Social determinants of health should be identified as risk factors and used for risk adjustment of populations. Primary care physicians cannot be held accountable for providing resources to address social determinants of health that do not exist in the community.
Financial benchmarks in VBP models should incentivize high-quality, efficient, accountable care delivery by establishing targets that reward both improvement and sustained performance over time.
Performance measures should focus on processes and outcomes that matter most to patients and have the greatest impact on overall health and unnecessary spending. VBP measures, as well as the mechanisms of measurement, should be parsimonious and aligned across payers to reduce unnecessary administrative burden.
Clinically relevant and actionable patient information should be readily available in a timely, accurate, secure, and efficient manner that does not place unnecessary administrative or financial burdens on primary care practices.
