“M&M” conferences have traditionally been the means for addressing medical errors, but too often they have focused on assigning individual blame rather than identifying root causes within systems.
Fam Pract Manag. 2023;30(2):13-17
Author disclosures: no relevant financial relationships.

Medical errors are the third leading cause of mortality in the U.S., resulting in as many as 98,000 deaths annually.1,2 Yet open discussions and analyses of the causes of errors occur infrequently.3,4 Clinicians may avoid these discussions because they fear being perceived as less than competent or they have concerns about disciplinary action and litigation.5,6 However, unaddressed errors can cause clinicians to internalize feelings of anger, shame, and guilt, making them more likely to suffer from burnout.6–9 Collaborating to identify and fix the root causes of errors improves quality of care and prevents future errors.9 It also provides positive support and useful learning for all team members, particularly those closely involved in the error.6
Most errors are the result of bad systems, not bad people. Focusing on assigning blame to individuals does not prevent others in the organization from making the same error in the future. On the other hand, focusing on systems and processes makes errors less likely to begin with, resulting in more meaningful long-term changes.10
Morbidity and mortality (M&M) conferences have traditionally been the means of addressing medical errors,11 but they have too often focused on individuals rather than systems. In 2019, our department launched a quarterly M&M conference series designed to provide a supportive and nonjudgmental forum for in-depth, structured root cause analysis. The ultimate goal is to identify actionable steps focused on quality improvement and patient safety.12,13 With almost 300 physicians, 75 residents, and more than 250 advance practice providers spread across 62 sites and four residency programs in three states, we strive to highlight issues and solutions that are applicable to diverse practice settings. As a bonus, the conference series helps our family physicians meet maintenance of certification quality improvement requirements from the American Board of Family Medicine as well as requirements for root cause analysis training from the Accreditation Council for Graduate Medical Education and the Joint Commission.
This article explains our process, provides two case examples, and shares our lessons learned.
KEY POINTS
Most errors are the result of bad systems, not bad people; focusing on fixing systems and processes makes errors less likely to occur in the future.
Quarterly M&M conferences can provide a forum for in-depth, structured root cause analysis and identification of actionable steps focused on quality improvement and patient safety.
Keys to success are identifying a dedicated review board to select appropriate cases, involving content experts, creating a supportive and nonjudgmental environment, and encouraging participation and discussion.
ESTABLISHING A REVIEW BOARD
Our M&M review board is a dedicated group of individuals who select appropriate cases, review the cases to identify system-related errors, identify content experts to provide additional teaching during the conference, and follow up with practices to assist in implementing recommended changes. The eight-person review board has representation from staff physicians, advanced practice providers, and family medicine residents. Ad hoc members include representation from pharmacy, social work, and nursing. All members of the review board receive instruction on reviewing cases, including the key components involved in error analysis and root cause analysis.14 Each member receives a suggested reading list to familiarize themselves with case reviews and M&M conferences. Beyond that, no additional training is provided, although several members have been actively involved in our institution's quality committees.
Clinicians are encouraged to submit cases involving errors or adverse events to the M&M review board by contacting members directly via email or through their clinic medical director. Once members receive a case, they examine the details independently. During this initial review, they determine whether there are any opportunities for system- or process-wide changes and whether changes would be feasible within the department or institution. Members then vote on whether the case is appropriate for further review as a group and should be presented at a conference. If the case is deemed eligible, the board meets to review the case and includes input from the primary care clinician or referring clinician. Most cases are reviewed within one month of referral.
The M&M review board understands the sensitive nature of medical errors and maintains a collegial, no-finger-pointing environment. At the beginning of each review board meeting, members are reminded of the following ground rules and objectives:
Review how systems and human factors can result in undesired medical outcomes,
Identify system issues that might contribute to undesired medical outcomes,
Have constructive discussions focused on preventing medical errors with an emphasis on learning from mistakes and finding ways to continually improve systems and processes.
Members follow structured guidelines to review and analyze a case. First, they conduct an error analysis, which involves going through the main events chronologically that led to the adverse outcome. This is followed by a root cause analysis, which focuses on physical, human, and organizational/administrative factors that could have contributed to or facilitated the error.10,14 Physical causes may include deficiencies in materials or guidelines (e.g., medication or equipment shortages, malfunctioning equipment, unexpected EHR downtime, inadequate clinic examination rooms, lack of available hospital beds, or lack of institutional guidelines). Human causes may include staffing shortages, excessive workloads, inadequate training, or knowledge gaps. Organizational causes may include workflow problems (e.g., nursing, scheduling, or laboratory workflows), ineffective reminders or prompts (e.g., medication interaction or allergy prompts in the EHR), lack of system redundancies (e.g., hospital pharmacists double-checking medication interactions or allergies), and communication problems (e.g., hospital discharge summaries that lack clear instructions for patients and outpatient clinicians).
Throughout this process, members identify actions that were completed correctly as well as those in need of improvement. They also identify actionable system- and process-related improvements in the following domains: communication, coordination of care, escalation of care, workload, and error/problem recognition. Finally, they discuss how the adverse event could have affected the health care team involved in the case, with the hope of identifying opportunities to improve staff well-being, support the team, and manage emotions and biases.
CONDUCTING AN M&M CONFERENCE
During an M&M conference, a member of the review board acts as moderator, stating the goal of continuous process and quality improvement, introducing the case presenter, reviewing the ground rules and objectives listed previously, and reminding attendees to have a constructive discussion without blaming or finger-pointing. The moderator keeps the conference running on schedule, reserving sufficient time for audience interaction following the case presentation. The moderator is also responsible for maintaining a collegial tone throughout the conference. (See the “M&M conference timeline.”)
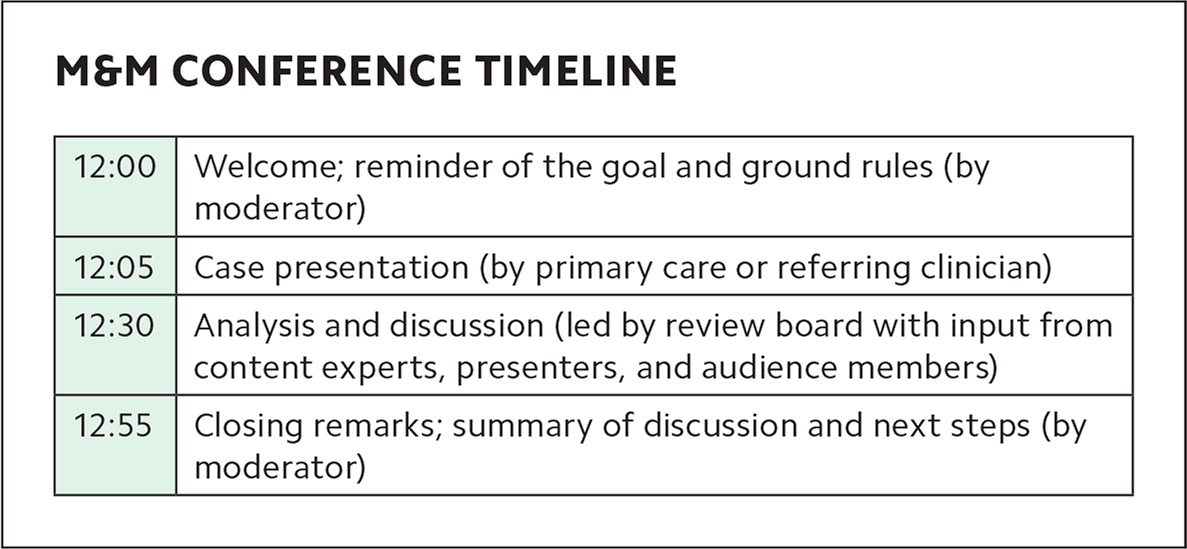
| 12:00 | Welcome; reminder of the goal and ground rules (by moderator) |
| 12:05 | Case presentation (by primary care or referring clinician) |
| 12:30 | Analysis and discussion (led by review board with input from content experts, presenters, and audience members) |
| 12:55 | Closing remarks; summary of discussion and next steps (by moderator) |
Following the moderator's opening remarks, the case presenter describes the actual events surrounding the medical error in neutral language. The presenter is typically someone close to the case, such as the primary care or referring clinician. For inexperienced presenters, M&M conferences can be intimidating.15 Members of the review board act as mentors for presenters who are unfamiliar with the format or inexperienced with group presentations, helping them organize and practice their presentation ahead of time if needed.
Following the case presentation, the moderator guides analysis, including root cause analysis, and leads the discussion of proposed system changes. At this point, audience interaction is encouraged. In addition, the invited content experts assist in answering questions and providing additional insight.
To encourage participation, our conferences are widely advertised within our department and livestreamed on our intranet platform to all locations. Prior to the COVID-19 pandemic, meeting rooms with audio-visual capabilities were set up in multiple locations for attendees. Since then, we have transitioned entirely to virtual meetings using Zoom. Attendees can submit written comments and questions through the group chat function, or they can submit anonymous comments and questions through a moderated platform (we use Slido).
A key deliverable from the conference is a list of proposed changes and recommendations based on input from all attendees. Members of the review board then present their final recommendations to primary care leaders, who are ultimately responsible for assessing feasibility, implementing changes, disseminating education, and ensuring compliance.
Following each conference, audience members are asked to complete an anonymous post-conference survey, which was adapted from a survey by Spielman et al.16
EXAMPLES OF CASE REVIEWS
Following are two examples of case reviews brought before the review board, including the recommendations and actions that resulted from the M&M conference process.
Case 1: This case involved an elderly female with a history of colon cancer and multiple co-morbidities. Shortly after her colon cancer diagnosis, the patient informed the outpatient team that she did not wish to have further interventions and preferred to take a comfort approach. Her wishes were documented in several outpatient encounter notes, but the patient did not have an advance directive in place and there was no formal discussion or documentation of advance care planning. Several months after diagnosis, the patient was admitted to the hospital for profound weakness; she was found to be in renal failure, anemic, and hyperkalemic. Her family could not be reached initially, so the patient underwent multiple transfusions and received care in the intensive care unit. When the family was finally contacted and goals of care were clarified, the patient was discharged to home hospice care. She passed away several days later.
In this case, members of the review board determined that the clinic lacked reminders and workflows to prompt clinicians to have advance care planning discussions with patients, especially those with life-limiting diagnoses. Additionally, clinicians could not easily determine whether a patient had an advance directive on file and, if so, how to find it. A palliative care specialist was invited to speak at the conference about how best to initiate discussions about goals of care, proper ways to document these discussions, and navigating the EHR system. Suggestions from attendees included making the presence or absence of advance care planning documentation more visible in the EHR, as well as including prompts to have such discussions. An additional recommendation was to add a “surprise” question to daily care team huddles: “Would you be surprised if any patient on today's schedule died in the next year?” If team members answer “no,” they should prioritize advance care planning with those patients and their families and ensure appropriate documentation in the patient record. A final recommendation was to update the discharge summary template to include 1) documentation of advance care planning discussions that take place during hospitalization and 2) recommendations for outpatient palliative care consultation, if appropriate.
The M&M review board ultimately brought these suggestions to primary care leadership, which led to updates in our EHR system. All patients with an advance directive on file now have a specific icon in their electronic record, and prompts have been built into the EHR to initiate advance care planning discussions with all patients 65 years and older.
Case 2: This case involved an adult female patient who underwent a screening colonoscopy and was found to have a polypoid mass in the proximal rectum, which was biopsied. Around the same time, the patient's primary care physician (who had ordered the screening) left the practice, and the patient was assigned to a new physician. During this transition period, multiple care team members handled the patient's test results. This coincided with a change in the EHR system, which made colonoscopy reports and pathology reports available separately. As a result, the patient was mistakenly informed to repeat the colonoscopy in three years due to the presence of “polyps” instead of being seen for immediate follow up. Eighteen months later, the patient developed rectal bleeding and was diagnosed with invasive adenocarcinoma of the rectum.
In this case, members of the review board and participants in the M&M conference put forth a new process to address communication problems related to colonoscopy and associated biopsy reports. First, the endoscopy nurses and physicians would huddle after every endoscopic procedure to optimize documentation by gastroenterology. The endoscopist would use a standardized documentation template to avoid communication errors in endoscopy reports and would communicate urgent results to the primary care clinician (if the ordering provider was not the primary care clinician or was unavailable). Lastly, the primary care clinician would contact the endoscopist directly if reports were unclear.
LESSONS LEARNED
Launching a quarterly M&M conference series has had some challenges but has been mostly rewarding as we strive to build a culture of learning, collaboration, and collegiality. We have been pleasantly surprised by the responses to our post-conference surveys. To date, 100% of respondents have reported that the conferences were moderately to extremely educational, 93% have reported feeling moderately to extremely engaged in the process, and 85% have reported that their ability to prevent or handle similar cases or complications in the future was either enhanced or greatly enhanced.
One early constraint was that we lacked a mechanism to allow for interactive participation from multiple geographically dispersed participants. The addition of live chat and anonymous commenting options has been helpful in this regard. We tried polling software to gain audience opinions in real time, but it was met with mixed reviews mainly due to unfamiliarity with the software. We hope to incorporate more live polling in future conferences.
Although we practice within a large organization, this model could be applied in smaller settings. If reviewing and presenting cases on a quarterly basis proves logistically challenging in smaller practices, reducing the frequency to 2–3 times per year would be a good start.
We believe the high level of interest, engagement, and support for this program has been due to several factors: 1) the systems- and process-focused analysis, 2) the participation of content experts, and 3) the group of dedicated case reviewers, all of which allow us to better identify areas of deficiency, enhance learning, and come up with actionable solutions to improve quality of care and optimize safety. But perhaps the key factor is providing a supportive environment focused on learning and systems improvement, rather than focusing on assigning blame.