This supplement is sponsored by the American Academy of Family Physicians.
Fam Pract Manag. 2023;30(2):9-12
When the Centers for Medicare & Medicaid Services (CMS) implemented the Quality Payment Program (QPP) in 2017, it combined three existing programs: the Physician Quality Reporting System, the Value-based Payment Modifier Program, and the meaningful use program. In some ways, the QPP provided more flexibility than previous CMS programs. For example, rather than being prescriptive about which quality measures a physician had to report, CMS allowed physicians to select measures from the CMS quality measures inventory that they wished to report. However, the program still included many of the complex and burdensome reporting requirements of the past. As the QPP enters its seventh year, CMS is taking a new approach.
Beginning in 2023, eligible clinicians (ECs) will have a new option to report in the Merit-based Incentive Payment System (MIPS) track. This new option is called MIPS Value Pathways (MVPs). MVPs are intended to reduce burden, connect measures and activities across the four performance categories, capture the patient voice, and move toward higher-value care. CMS hopes MVPs will provide ECs with a more meaningful reporting option that can reduce barriers to alternative payment model (APM) participation.
MVPs are a reporting option that offers a subset of measures and improvement activities centered around a specialty, condition, or public health priority. In general, each MVP will include around 10 quality measures and 10 improvement activities. By providing a smaller set of connected measures and activities, CMS hopes to make it easier for ECs to identify and report measures that they find more meaningful and applicable in their practice.
Are MVPs mandatory?
No. MVPs are currently optional. However, CMS intends to eliminate traditional MIPS and make MVPs mandatory in the future.
Who can report MVPs?
Any eligible clinician can report an MVP. For the 2023, 2024, and 2025 MIPS performance years, MVP participants include individual clinicians, single specialty groups, multispecialty groups, and APM entities. CMS will also allow practices to form subgroups to report MVPs.
What is a subgroup?
A subgroup comprises a subset of clinicians within the same tax identification number (TIN). The traditional MIPS reporting options require all clinicians under a TIN to report the same measures and activities. This can make it particularly challenging for physicians in multispecialty practices to report measures that are meaningful to them. Subgroup reporting under MVPs provides an alternative by allowing practices to form subgroups of clinicians who can report the MVP that is most relevant to their specialty or the conditions they manage rather than reporting the same measures as every other clinician in the practice.
An EC is only allowed to participate in one subgroup per TIN. CMS has not established any requirements for the composition of subgroups, and subgroups are not limited to one specialty. For example, a practice with primary care physicians and cardiologists may choose to form two subgroups—one that includes the primary care physicians and one that includes the cardiologists. In this example, the subgroup for primary care physicians could include both family physicians and internists.
Is subgroup reporting mandatory?
No. Subgroup reporting is currently optional. However, beginning with the 2026 performance year, multispecialty practices will be required to form subgroups to report MVPs.
What are the reporting requirements for MVPs?
Eligible clinicians who elect to report an MVP are assessed on the same four performance categories as those who report via the traditional MIPS options: (1) quality; (2) improvement activities; (3) cost; and (4) promoting interoperability (Table 1). However, as an incentive to report MVPs, CMS has eased some of the reporting requirements.
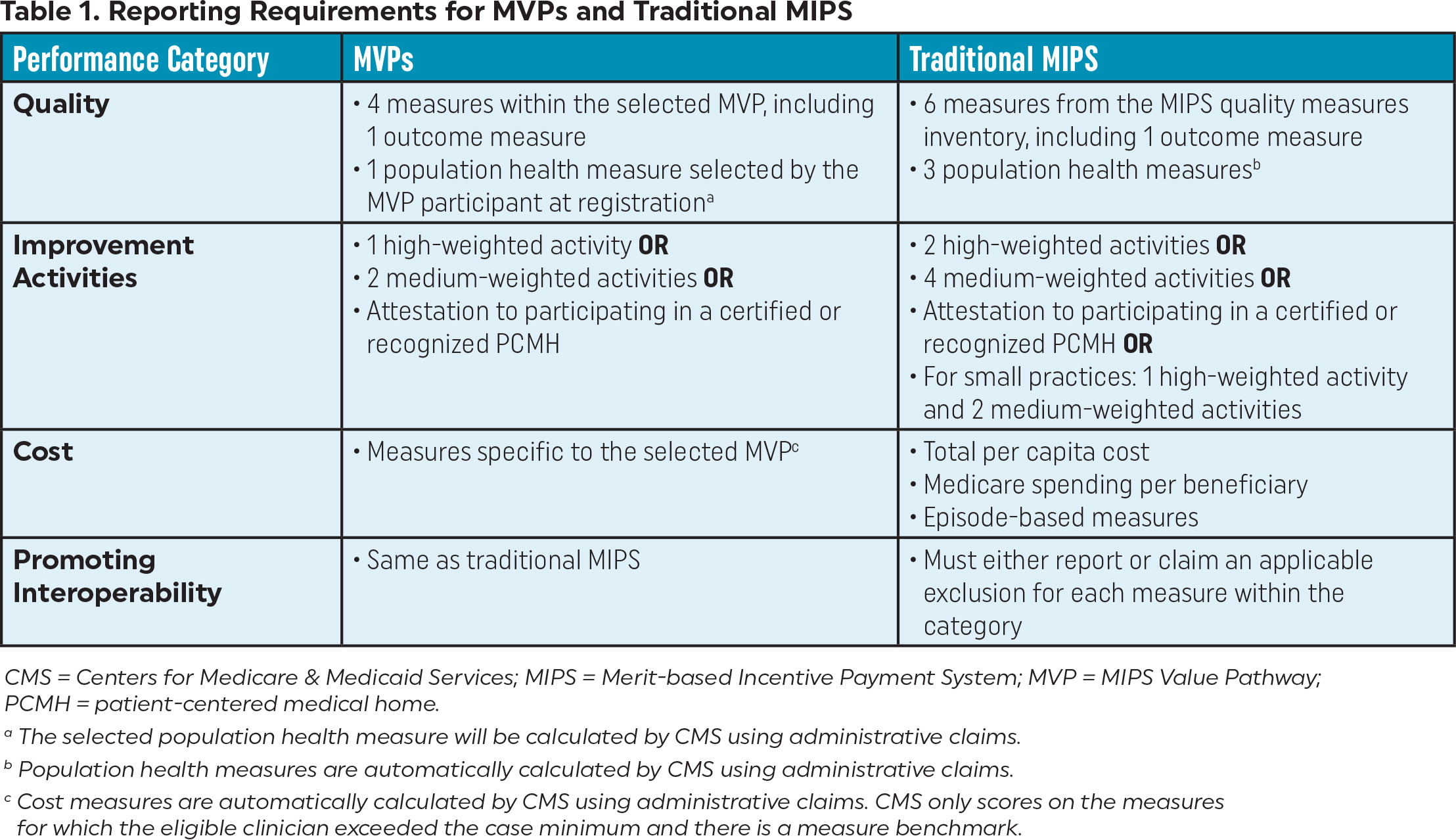
| Performance Category | MVPs | Traditional MIPS |
|---|---|---|
| Quality |
|
|
| Improvement Activities |
|
|
| Cost |
|
|
| Promoting Interoperability |
|
|
How do I report an MVP?
Eligible clinicians who want to report an MVP must register, and practices must register any subgroups that will report MVPs. Registration will open April 1 of the applicable performance year or on a later date specified by CMS. For the 2023 performance year, registration opens on April 3. Registration will close November 30 of the applicable performance year or on a later date specified by CMS.
After the registration window closes, MVP participants will not be able to make changes to their registration of the following:
Selection of one MVP
Selection of one population health measure
Selection of an outcomes-based administrative claims measure (if applicable)
For subgroups only:
– List of each TIN/National Provider Identifier (NPI) associated with the subgroup
– Name and description of the subgroup
What happens if I register to report an MVP but decide to report another way?
Neither MVP nor subgroup registration is binding. Eligible clinicians who register to report an MVP but change their mind can report via traditional MIPS instead. CMS will assign the highest final score that can be attributed to the EC from any reporting option and participation option.
How do I select an MVP?
Twelve MVPs are available for the 2023 performance year. They are listed on the QPP website. Eligible clinicians should consider whether the measures within an MVP are meaningful and applicable to them and the patients they serve. They should also compare the measures in the MVP to their contracts and payment arrangements with other payers so these can be aligned when possible.
Currently, the existing APM options are limited, but it still may be beneficial to compare MVPs to these options. This can give practices an idea of whether the MVP measures align with the types of measures included in APMs.
What MVPs are available for primary care?
For the 2023 performance year, two MVPs are focused on primary care: (1) Promoting Wellness and (2) Optimizing Chronic Disease Management. However, participants are free to report any MVP they wish.
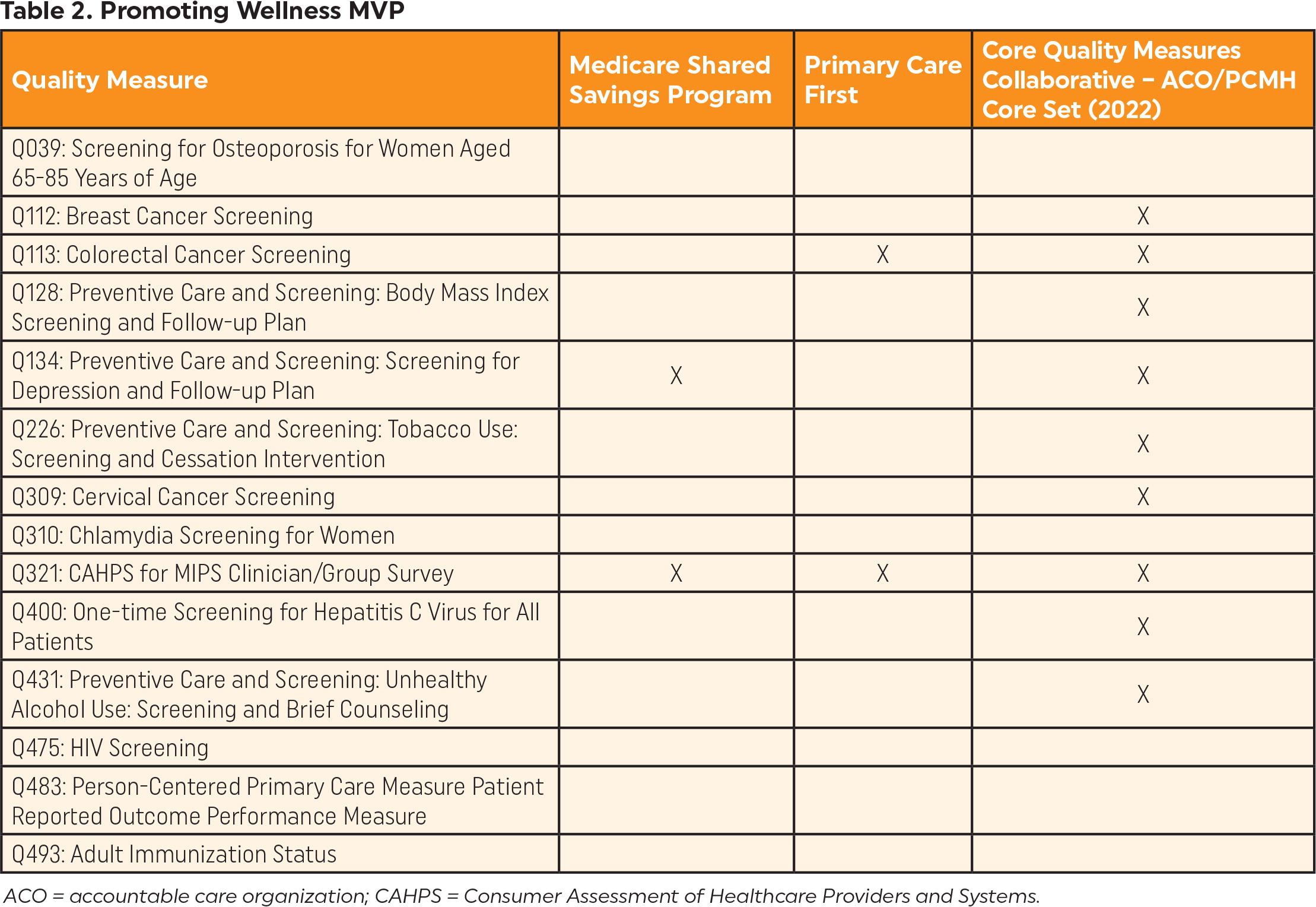
| Quality Measure | Medicare Shared Savings Program | Primary Care First | Core Quality Measures Collaborative – ACO/PCMH Core Set (2022) |
|---|---|---|---|
| Q039: Screening for Osteoporosis for Women Aged 65–85 Years of Age | |||
| Q112: Breast Cancer Screening | X | ||
| Q113: Colorectal Cancer Screening | X | X | |
| Q128: Preventive Care and Screening: Body Mass Index Screening and Follow-up Plan | X | ||
| Q134: Preventive Care and Screening: Screening for Depression and Follow-up Plan | X | X | |
| Q226: Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | X | ||
| Q309: Cervical Cancer Screening | X | ||
| Q310: Chlamydia Screening for Women | |||
| Q321: CAHPS for MIPS Clinician/Group Survey | X | X | X |
| Q400: One-time Screening for Hepatitis C Virus for All Patients | X | ||
| Q431: Preventive Care and Screening: Unhealthy Alcohol Use: Screening and Brief Counseling | X | ||
| Q475: HIV Screening | |||
| Q483: Person-Centered Primary Care Measure Patient Reported Outcome Performance Measure | |||
| Q493: Adult Immunization Status |
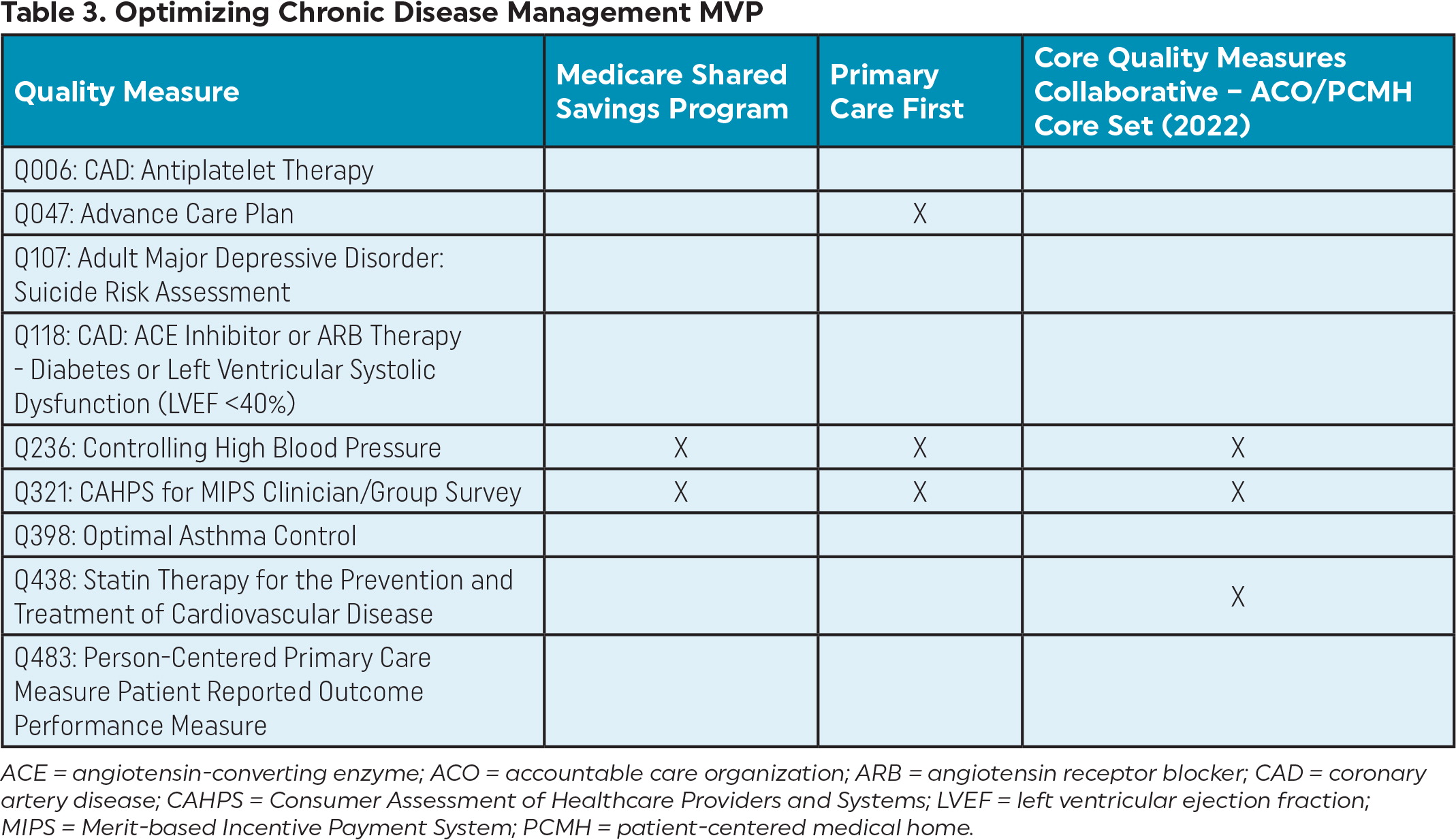
| Quality Measure | Medicare Shared Savings Program | Primary Care First | Core Quality Measures Collaborative – ACO/PCMH Core Set (2022) |
|---|---|---|---|
| Q006: CAD: Antiplatelet Therapy | |||
| Q047: Advance Care Plan | X | ||
| Q107: Adult Major Depressive Disorder: Suicide Risk Assessment | |||
| Q118: CAD: ACE Inhibitor or ARB Therapy - Diabetes or Left Ventricular Systolic Dysfunction (LVEF <40%) | |||
| Q236: Controlling High Blood Pressure | X | X | X |
| Q321: CAHPS for MIPS Clinician/Group Survey | X | X | X |
| Q398: Optimal Asthma Control | |||
| Q438: Statin Therapy for the Prevention and Treatment of Cardiovascular Disease | X | ||
| Q483: Person-Centered Primary Care Measure Patient Reported Outcome Performance Measure |
How are MVPs developed?
MVP candidates are developed by a variety of stakeholders, including clinicians, patients, and specialty societies. They can be submitted to CMS throughout the year on a rolling basis using the MVP Development Standardized Template on the QPP website. To ensure that an MVP meets patient and clinician needs, CMS strongly encourages submitters to work collaboratively with other stakeholders who may be impacted by it.
Once an MVP candidate is submitted, CMS will review the submission and contact stakeholders with questions, if necessary. CMS will identify potential MVPs in the Medicare Physician Fee Schedule (MPFS) proposed rule. MVPs approved for use within the program will be finalized in the MPFS final rule.
The public has several opportunities to provide feedback to CMS on proposed or finalized MVPs. Viable MVP candidates will be posted on the QPP website to solicit feedback for a 30-day period. Stakeholders will have an opportunity to comment on proposed MVPs through the rulemaking process. In addition, the public can recommend changes to previously finalized MVPs on a rolling basis via the QPP website.
For More Information
Information and practical resources on MVPs are available online from the American Academy of Family Physicians (AAFP).