Knowing how your services are valued is key to understanding and improving your productivity.
Fam Pract Manag. 2023;30(2):4-8
Author disclosure: no relevant financial relationships.
Note: This article uses 2023 RVUs for illustrative purposes. For the latest RVUs, consult the CMS Physician Fee Schedule look-up tool.

Although the use of value-based payment models is growing,1 the most common payment method in physicians' employment contracts is still a base salary plus a production bonus based largely on relative value units (RVUs).2 RVUs reflect a physician's volume of work and level of effort in treating patients. The more RVUs a physician generates, the more income the practice (and the physician) should receive.
Knowing the RVUs assigned to different types of services allows physicians to understand how their productivity is measured. And knowing their RVUs per visit and per year allows physicians to understand how they compare to their peers. They can then assess whether they need to see more patients, work more efficiently, or change key processes such as billing and coding to better reflect the amount of work they are doing.
The four questions outlined in this article can help physicians get started in understanding and improving their RVUs.
KEY POINTS
Knowing the work RVUs assigned to different types of services can help you understand how your productivity is being measured.
Work RVUs vary depending on the work and effort required; for example, a 99212 has 0.70 work RVUs while a 99214 has 1.92 work RVUs.
To improve your total work RVUs per year, you may need to work more efficiently so you can see more patients, improve your coding practices to capture the full value of your work, or offer more high-value services, such as procedures or transitional care management.
1. WHAT ARE RVUS?
RVUs are part of the Resource-Based Relative Value Scale (RBRVS), which Medicare and other payers have used for decades to determine payment for physician services. RVUs are just one of three components that factor into the payment calculation.3 The other two components are geographic practice cost indices (GPCIs), which adjust RVUs to reflect regional differences in the cost of physician services, and a conversion factor (CF), which is the dollar amount by which total, geographically adjusted RVUs are multiplied to arrive at the payment amount for a given service. (See “How payment for a service is calculated.”)
Total RVUs are the sum of three types:
Work RVUs, which reflect the physician's work, including mental effort, decision making, technical skills, physical effort, stress related to patient risk, and amount of time spent,
Practice expense RVUs, which reflect the clinical and nonclinical labor costs and practice expenses,
Malpractice RVUs, which reflect the liability insurance costs.
The remainder of this article will focus on work RVUs because they are a key measure of physician productivity. Work RVUs for common services in primary care are listed at the end of this article. For example, a 99214 established patient evaluation and management (E/M) office visit has 1.92 work RVUs, a “Welcome to Medicare” visit has 2.6 work RVUs, and a 99223 initial hospital visit (admission) has 3.5 work RVUs.
HOW PAYMENT FOR A SERVICE IS CALCULATED
Relative value units (RVUs) are just one of three components that factor into physician payment under the Resource-Based Relative Value Scale:
Total RVUs, which is the sum of work RVUs, practice expense (PE) RVUs, and malpractice RVUs,
Geographic practice cost indices (GPCIs), which adjust RVUs to reflect regional differences in the cost of physician services,
A conversion factor (CF), which is the annually updated dollar amount by which total, geographically adjusted RVUs are multiplied to arrive at the payment amount for a given service.
Payments are calculated as follows:
[(Work RVUs x Work GPCI) + (PE RVUs x PE GPCI) + (Malpractice RVUs x Malpractice GPCI)] x CF = Payment amount
2. WHAT ARE YOUR WORK RVUS?
If you are an employed physician, you likely receive productivity reports from your employer, but you may not be in the habit of looking at them closely or you may not know what to do with the information. A helpful report should provide you with the following individualized data:
Work RVUs,
Annualized work RVUs (projected total if you continue to generate the same amount of work for the rest of the fiscal year),
Number of visits,
Annualized number of visits,
Types of visits you are seeing (such as preventive care visits, E/M visits, hospital visits, and Medicare wellness visits),
A breakdown of your E/M visits (i.e., what percentage are coded as level 1, 2, 3, 4, or 5).
If you are expected to meet a goal for work RVUs, you should receive your data on a regular and predictable basis — e.g., monthly, bimonthly, or quarterly — allowing you to analyze the data and make adjustments in scheduling, coding, or practice efficiency to meet the goal. Waiting until the end of the fiscal year to distribute a finalized report does not allow physicians enough time to make effective changes.
Data should be accurate, trustworthy, and presented to physicians in a user-friendly way. Practices should have a contact person who understands the information well and can answer physicians' questions or investigate discrepancies should they arise.
If your employer does not provide you with a productivity report, or does not provide it in a timely manner, ask for it. Most EHRs and practice management systems capture the required data and can generate customizable reports.
You can estimate your work RVUs on your own using the process described in the physician example.
HOW TO CALCULATE WORK RVUS PER VISIT AND PER YEAR: AN EXAMPLE
Dr. Smith is a family physician in a physician-owned outpatient practice. He sees an average of 10 patients per session, or 20 visits per day, and his average work RVUs are 1.69 per visit. Out of 260 total workdays per year, Dr. Smith has 40 days for vacation, continuing medical education, holidays, etc., leaving 220 workdays per year. That means he averages 4,400 visits and 7,436 work RVUs per year, which puts him well above the 50th percentile in national benchmarks but below the 90th percentile.
Here's the method used to estimate his work RVUs:
First, list the types of visits in an average session, assign work RVUs to each visit, and add the values to get the total work RVUs per session.
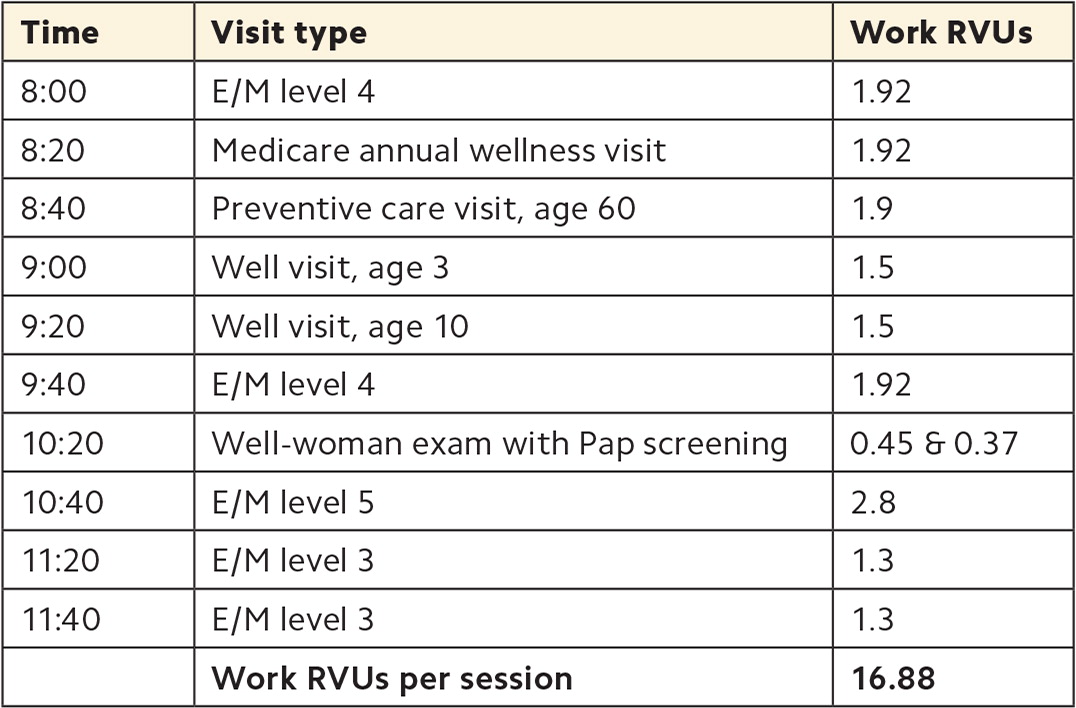
| Time | Visit type | Work RVUs |
|---|---|---|
| 8:00 | E/M level 4 | 1.92 |
| 8:20 | Medicare annual wellness visit | 1.92 |
| 8:40 | Preventive care visit, age 60 | 1.9 |
| 9:00 | Well visit, age 3 | 1.5 |
| 9:20 | Well visit, age 10 | 1.5 |
| 9:40 | E/M level 4 | 1.92 |
| 10:20 | Well-woman exam with Pap screening | 0.45 & 0.37 |
| 10:40 | E/M level 5 | 2.8 |
| 11:20 | E/M level 3 | 1.3 |
| 11:40 | E/M level 3 | 1.3 |
| Work RVUs per session | 16.88 |
Next, complete the following calculations:
Work RVUs per session ÷ Visits per session = Work RVUs per visit
16.88 ÷ 10 = 1.69
Workdays per year x Visits per day = Visits per year
220 x 20 = 4,400
Visits per year x Work RVUs per visit = Work RVUs per year
4,400 x 1.69 = 7,436
3. HOW DO YOUR WORK RVUS COMPARE TO BENCHMARKS
Practices should establish work RVU benchmarks at the beginning of the fiscal year and include them in productivity reports so physicians can see whether they are meeting work RVU goals. Practices may use internal data to set benchmarks, comparing you to your peers, or they may rely on national benchmarks from external sources. Benchmarks should be specialty-specific, but they may differ for inpatient versus outpatient practice, new versus established physicians, and physician-owned practices versus practices owned by hospital or health systems.
For example, according to data from the Medical Group Management Association, for family medicine physicians in physician-owned outpatient practices, the 50th percentile is 5,945 annual work RVUs and the 90th percentile is 9,063.4 Meanwhile, for those in hospital-owned or health-system-owned outpatient practice, the 50th percentile is 4,715 annual work RVUs and the 90th percentile is 7,451. One possible reason for the difference is that physician-owned practices may be more likely to reward productivity, while practices owned by a hospital or health system may be more likely to use straight salary compensation.
4. HOW CAN YOU INCREASE YOUR WORK RVUS?
If your work RVUs are below goal, there are several ways you may be able to increase them. Start by examining the following factors.
Visit volume. To assess whether low patient volume is contributing to low work RVUs, identify how many patients you see per day. A 2018 survey by the Physicians Foundation found an overall average of 20.2 patients per day across all specialties.5 According to data from the American Academy of Family Physicians, family physicians average 84 patient encounters per week — 63 in the office, 12 e-visits, seven in the hospital, and two in nursing homes or house calls.6 What ultimately matters is the benchmark your group is using. If your visit volume is too low, that does not necessarily mean that you need to work longer each day, but you may need to work more efficiently in order to see more patients. For example, you may need to delegate more tasks to your team, or you may need to address a high no-show rate.
Visit levels. Identify what percentage of your E/M visits are level 1 through 5, and compare this distribution to that of your peers. If your practice cannot provide this data, you can use national benchmarks derived from Centers for Medicare & Medicaid Services data (see this FPM worksheet, which has been updated with 2021 data). If you find that you are billing a higher percentage of lower-level visits than your peers, you will need to either see more patients to achieve the same overall work RVUs or investigate other issues. For example, it could be that your billing, coding, and documentation practices are inefficient, leading to under-coding or missed coding.
High-value visits. Identify which high-value visits you frequently provide, and which ones you should be providing. (See the list of work RVUs for different visit types on page 7.) For example, new patient visits have higher work RVUs than established patient visits, so if you've closed your panel to new patients, this could be affecting your work RVUs. Many procedures are also valued highly, so you may want to consider expanding your scope of practice by adding skin procedures, joint aspirations and injections, treadmill stress tests, etc. Transitional care management visits and Medicare annual wellness visits are also higher-value services. Consider whether you can provide these to patients who need them, and how your care team can assist with the workload.
Visit lengths. Track your visit lengths for various visit types to see whether you need to adjust your scheduling practices. Adjusting visit duration in your scheduling template can allow you to see more patients per day or per session to meet your work RVU goals. For example, a physician who has a goal of 30 work RVUs per day and averages 1.3 work RVUs per visit (the equivalent of an established-patient, level 3 office visit) would need to see 23 patients per day. In an eight-hour workday, that would allow for an average of 20-minute visits. Note that time-based billing became easier following the 2021 E/M coding changes and now includes the physician's total time spent on the day of the visit (not only face-to-face time but also pre-visit planning, coordination of care after the visit, and other physician activities).
WORK RVUS FOR COMMON VISIT TYPES
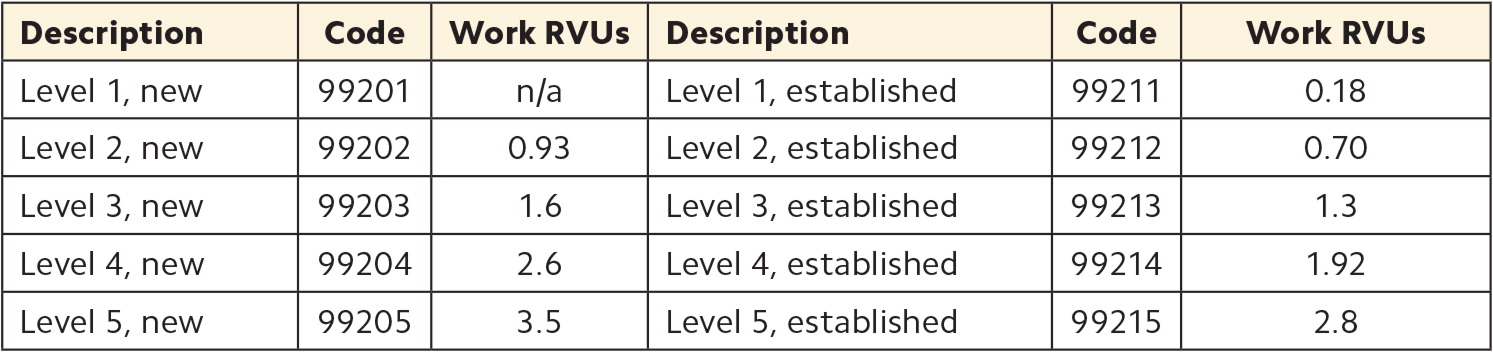
| Description | Code | Work RVUs | Description | Code | Work RVUs |
|---|---|---|---|---|---|
| Level 1, new | 99201 | n/a | Level 1, established | 99211 | 0.18 |
| Level 2, new | 99202 | 0.93 | Level 2, established | 99212 | 0.70 |
| Level 3, new | 99203 | 1.6 | Level 3, established | 99213 | 1.3 |
| Level 4, new | 99204 | 2.6 | Level 4, established | 99214 | 1.92 |
| Level 5, new | 99205 | 3.5 | Level 5, established | 99215 | 2.8 |
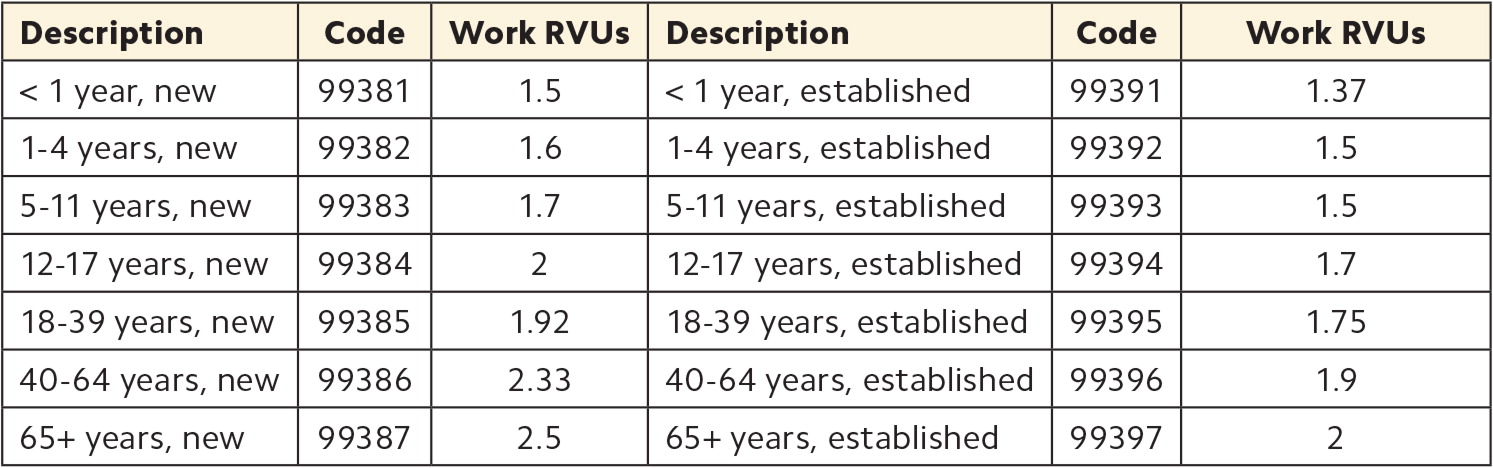
| Description | Code | Work RVUs | Description | Code | Work RVUs |
|---|---|---|---|---|---|
| < 1 year, new | 99381 | 1.5 | < 1 year, established | 99391 | 1.37 |
| 1–4 years, new | 99382 | 1.6 | 1–4 years, established | 99392 | 1.5 |
| 5–11 years, new | 99383 | 1.7 | 5–11 years, established | 99393 | 1.5 |
| 12–17 years, new | 99384 | 2 | 12–17 years, established | 99394 | 1.7 |
| 18–39 years, new | 99385 | 1.92 | 18–39 years, established | 99395 | 1.75 |
| 40–64 years, new | 99386 | 2.33 | 40–64 years, established | 99396 | 1.9 |
| 65+ years, new | 99387 | 2.5 | 65+ years, established | 99397 | 2 |
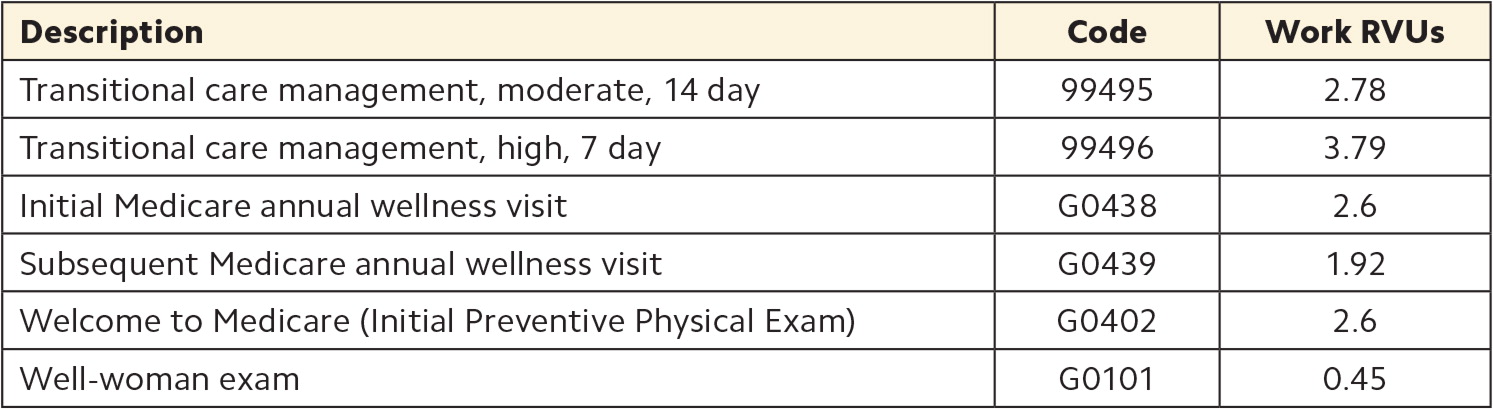
| Description | Code | Work RVUs |
|---|---|---|
| Transitional care management, moderate, 14 day | 99495 | 2.78 |
| Transitional care management, high, 7 day | 99496 | 3.79 |
| Initial Medicare annual wellness visit | G0438 | 2.6 |
| Subsequent Medicare annual wellness visit | G0439 | 1.92 |
| Welcome to Medicare (Initial Preventive Physical Exam) | G0402 | 2.6 |
| Well-woman exam | G0101 | 0.45 |
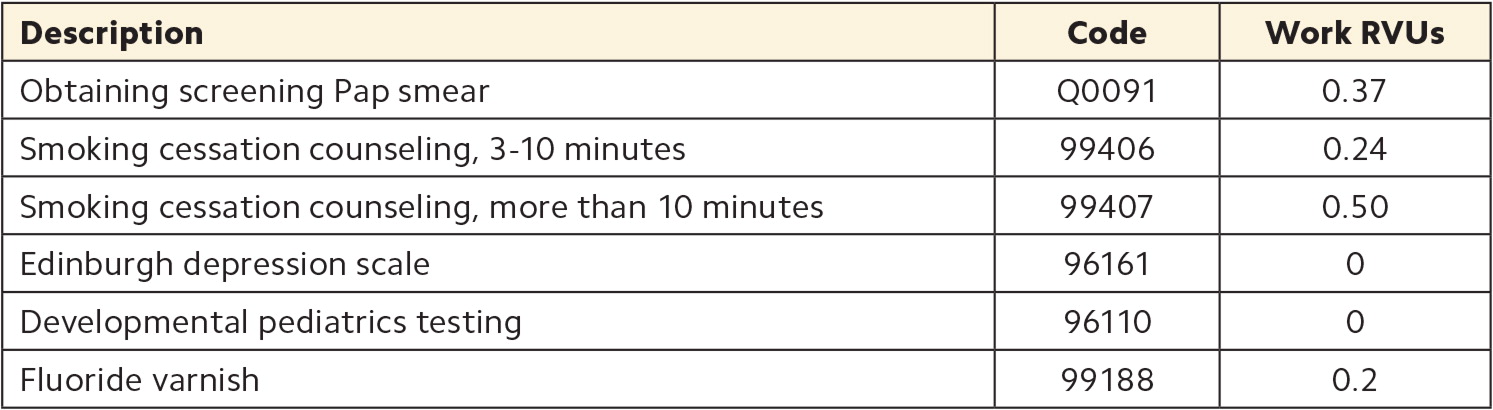
| Description | Code | Work RVUs |
|---|---|---|
| Obtaining screening Pap smear | Q0091 | 0.37 |
| Smoking cessation counseling, 3–10 minutes | 99406 | 0.24 |
| Smoking cessation counseling, more than 10 minutes | 99407 | 0.50 |
| Edinburgh depression scale | 96161 | 0 |
| Developmental pediatrics testing | 96110 | 0 |
| Fluoride varnish | 99188 | 0.2 |
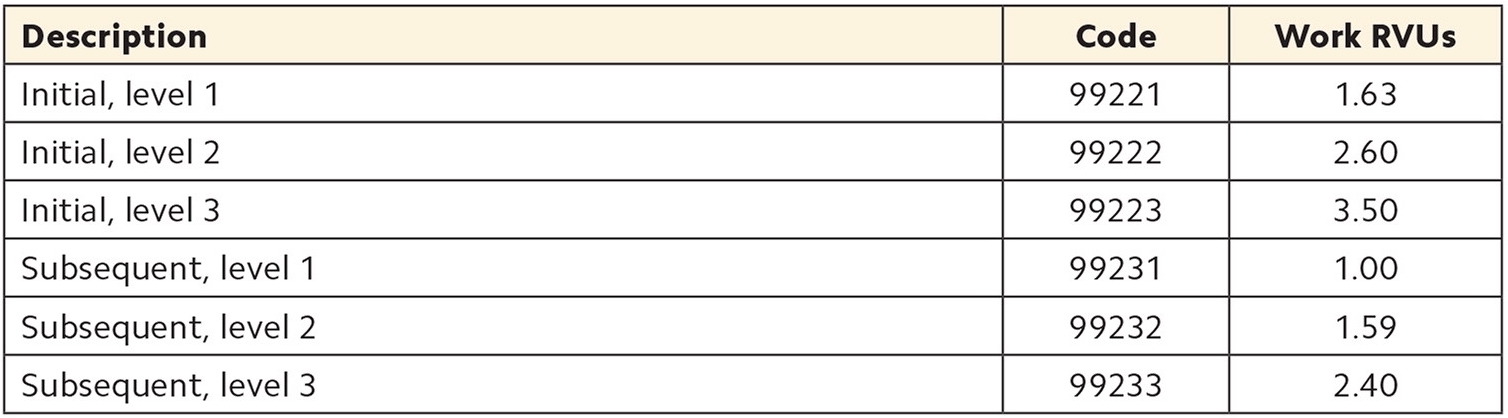
| Description | Code | Work RVUs |
|---|---|---|
| Initial, level 1 | 99221 | 1.63 |
| Initial, level 2 | 99222 | 2.60 |
| Initial, level 3 | 99223 | 3.50 |
| Subsequent, level 1 | 99231 | 1.00 |
| Subsequent, level 2 | 99232 | 1.59 |
| Subsequent, level 3 | 99233 | 2.40 |
FOCUSING ON WHAT YOU CAN CONTROL
Some aspects of physician productivity are beyond your control. For example, you can't really control whether your schedule is full every day or what level of care your patients need. However, it's still beneficial to understand the factors that are affecting your work RVUs so you can assess your performance and make the case for what you need, such as more clinical support staff or a second exam room. Improving productivity isn't just about working harder, but working smarter and identifying changes in practice operations and efficiency that will actually make a difference.