
Fam Pract Manag. 2023;30(5):13-14
The publication of this supplement is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

Your priorities as American Academy of Family Physicians (AAFP) members are abundantly clear — improve primary care payment systems and reduce administrative burdens.1 These are non-negotiable changes that must occur. The urgent and consistent messages from AAFP members and the Academy are that we must course correct for the many years of harm created by an under-valued fee-for-service (FFS) payment system built around very narrowly defined, discrete services incompatible with primary care's comprehensive nature.
Furthering the problem with the current FFS system is payment is limited to narrowly defined services that significantly undervalue primary care and its many contributions to achieving the Quadruple Aim of health care: enhancing the patient experience, improving population health, reducing the per capita cost of care, and improving the work life of physicians and other health care providers.2 Successfully addressing these priorities requires solving many issues on many fronts and clearly communicating our message to key stakeholders again and again.
ECHOING THE MESSAGE
The AAFP is experienced and visible in advocating and fighting for impactful and meaningful change for family medicine at the federal level. The message in June from AAFP Executive Vice President and Chief Executive Officer Shawn Martin when he testified before the Senate Finance Committee strongly echoed the Academy's consistent message — improving payment and reducing the administrative burden on primary care is essential to advancing the health care system with the goals of improving the quality of care and reducing the cost of care.3
The AAFP's persistent advocacy in Washington, D.C., and its support of state chapter advocacy, is essential to influence public payers. However, as many of you are well aware, private payers are just as important to achieving more equitable payment and reducing the burdens you face. And you deal with a lot of private payers.
Based on the annual Practice Profile Survey completed by AAFP members, 74% of practices receive payment from 7–10 payers, with more than one-third of respondents reporting that they maintain more than 14 unique payer contracts.4 The level of complexity created by their differing approaches to coverage, payment, and reporting is untenable and unsustainable.
The AAFP's advocacy with private payers is essential to addressing your priorities and why we've created the Beyond the Beltway series. This is the first in the series, with these informational pieces appearing as regular features in FPM.
HEALTH CARE DECISION-MAKING IS COMPLEX AND BROADLY DISTRIBUTED
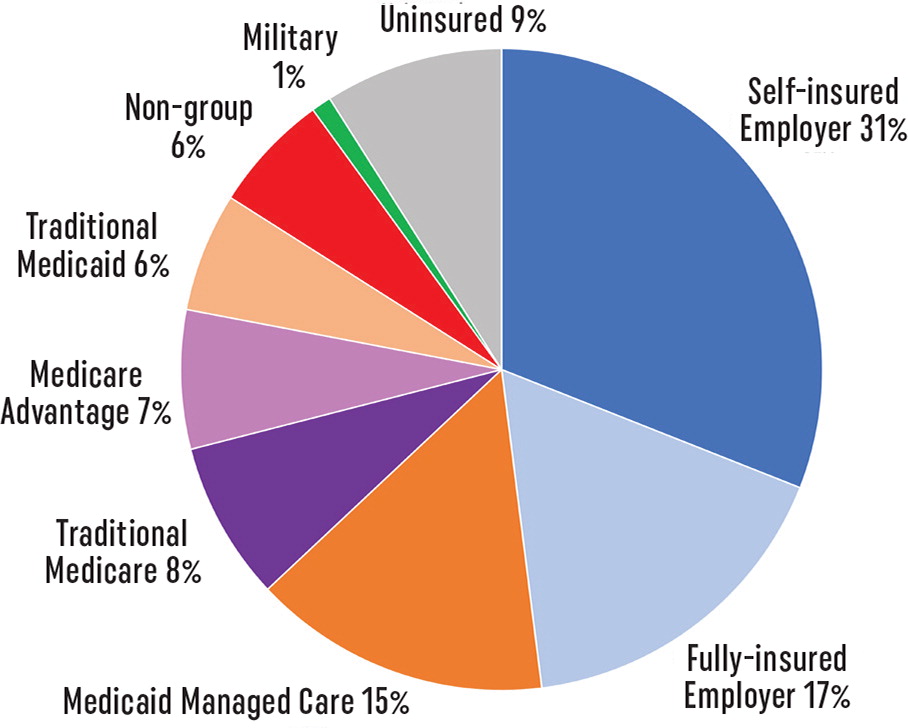
Broad distinctions between public and private are often made when classifying or categorizing payers (i.e., the entities who decide which services are covered by insurance plans, terms of payment, amount of payment for covered services, prior authorization approvals, and documentation requirements). Research and other health care cost, utilization, or quality reports typically delineate Medicare, Medicaid, and commercial payers (employer sponsored insurance). While these broad categories are useful for research and reporting purposes, the AAFP believes they underestimate the complexity of the health care payer landscape and the number of decision-makers that influence the level of payment and burdens that practices experience.
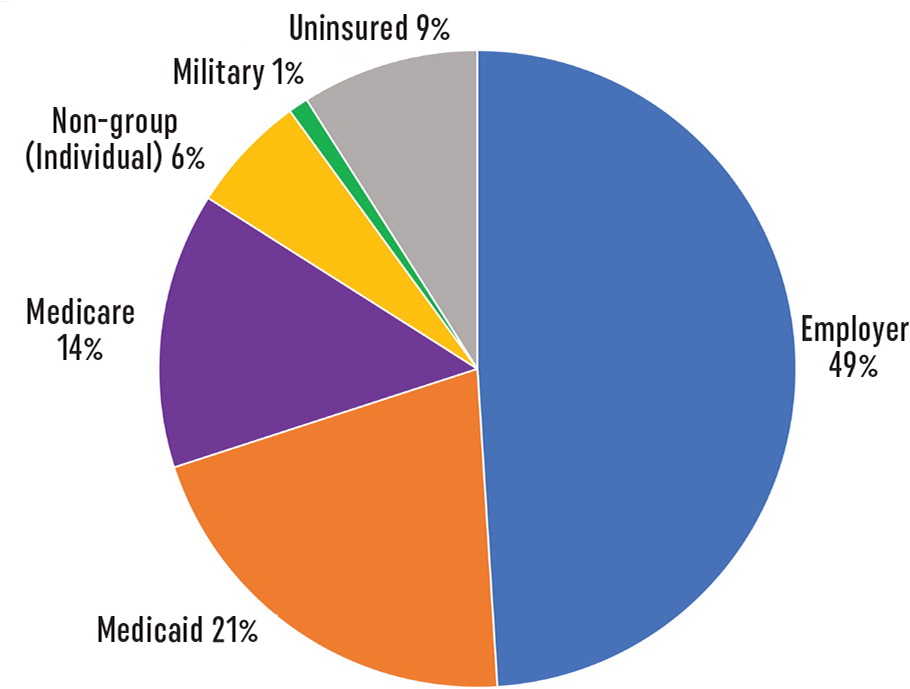
Based on this view, approximately 36% of Americans have public insurance through Medicare, Medicaid, and military coverage.5 Approximately 55% obtain coverage through private insurance, such as an employee or eligible dependent through employer coverage or individually purchasing non-group coverage, most of which happens through the exchange marketplaces.
The privatization of public coverage through Medicare Advantage and Medicaid Managed Care arrangements means that private payers are administering coverage for a growing number of enrollees in these public programs.6,7 And while employer-sponsored insurance covers the largest percentage of Americans,5 it is further complicated by a growing number of self-insured employers, which means each employer acts as the fiduciary on behalf of its plan, with the potential to add even greater complexity to the coverage and payment landscape.
AAFP ACTIONS
The AAFP has long advocated for the best interests of its members with the largest national health plans. While the Academy focuses its efforts at the national level, we understand that regional health plans significantly influence the payment barriers and administrative requirements you face daily in many markets. We will be sharing with state chapters the strategies the AAFP is implementing to extend the impact of our advocacy with national health plans. We encourage states to share with us what is and what is not working in their markets to enhance and accelerate our overall impact in this critical shared work.
We are also actively working to expand our impact with large employers and union trusts who purchase coverage on behalf of their workforce and/or members. Many of these organizations consider strengthening primary care central to achieving their health care improvement and cost management goals and are advancing initiatives to support their employer members in implementation.8,9
Too often, these private advocacy efforts undertaken by the AAFP happen outside the view of our members. The Beyond the Beltway series is our effort to rectify this. This new series will be written and developed by AAFP staff as an informational series. In the series, we will aim to:
Share the AAFP's private advocacy efforts to transform markets in favor of family medicine and primary care.
Empower AAFP members and allies with resources and insights that allow you and other stakeholders to confidently tackle the challenges of payment and burden in your states, regions, cities, and towns.
Keep you abreast of progress, regardless of its significance or even how minor it may seem.
In future installments, look for information focused on changes in the quality and performance measurement environment, evolving expectations around managing patients' health-related social needs, and updates on AAFP tools and resources for private stakeholder engagement.
We recognize that this is a broad and complicated landscape to navigate, and we vow to do our best to identify and feature the information we believe is most important to you and your practice. We also welcome your input on what matters to you and what is working in your local environment because the AAFP firmly believes that we are all in this together, and we can and will fix it together. You can contact the team at katef@aafp.org. Continue to look for the Beyond the Beltway series in future issues of FPM. They will have the same look and feel as this feature.