
Fam Pract Manag. 2023;30(6):31-36
The publication of this AAFP supplement is funded by an unrestricted grant from Sanofi Pasteur Inc.
Flu Vaccination Disparities and Their Toll
The COVID-19 pandemic exposed deep racial and ethnic health disparities that continue to plague our country. While we enacted strategies that produced some equity in COVID-19 vaccination, other vaccine disparities reemerged last year. For example, during the previous flu season in 2022–23, vaccination rates among people of color were much lower in all age groups1:
Black children had the lowest flu vaccination rates at 51% (versus 53.6% among white children, 58% among Hispanic children, and 60% among other children of color).
Black individuals who are pregnant had the lowest flu vaccination rate at 30.4% (versus 48.9% in the overall population of individuals who are pregnant; all demographics of individuals who are pregnant declined in the 2022–23 flu season).
Black adults (39.3%) and Hispanic adults (35.2%) had lower flu vaccination rates (versus 52.8% of white adults).
Black adults 65 years and older (40.2%) and Hispanic adults 65 years and older (32.1%) were much less likely to receive a flu vaccine (versus 55.2% of white adults 65 years and older).
Similarly, only 9.5% of Black individuals versus 16.7% of white individuals received the bivalent COVID-19 vaccine as of May 2023. Similarly, only 45% of Black individuals versus 51.9% of white individuals received the COVID-19 completed primary series.2
Research has shown the impact of these disparities. Black individuals have consistently higher rates of severe flu outcomes, as they are nearly two times more likely to be hospitalized and 1.7 times more likely to be admitted to the intensive care unit due to flu compared to white individuals.3
Hospitalization, intensive care unit (ICU), and in-hospital death rate disparities are especially pronounced among children 0–4 years, with non-Hispanic Black children 2.2 to 3.4 times more likely than white children to experience these outcomes.
Factors of Racial and Ethnic Disparities in Flu Vaccination and Outcomes
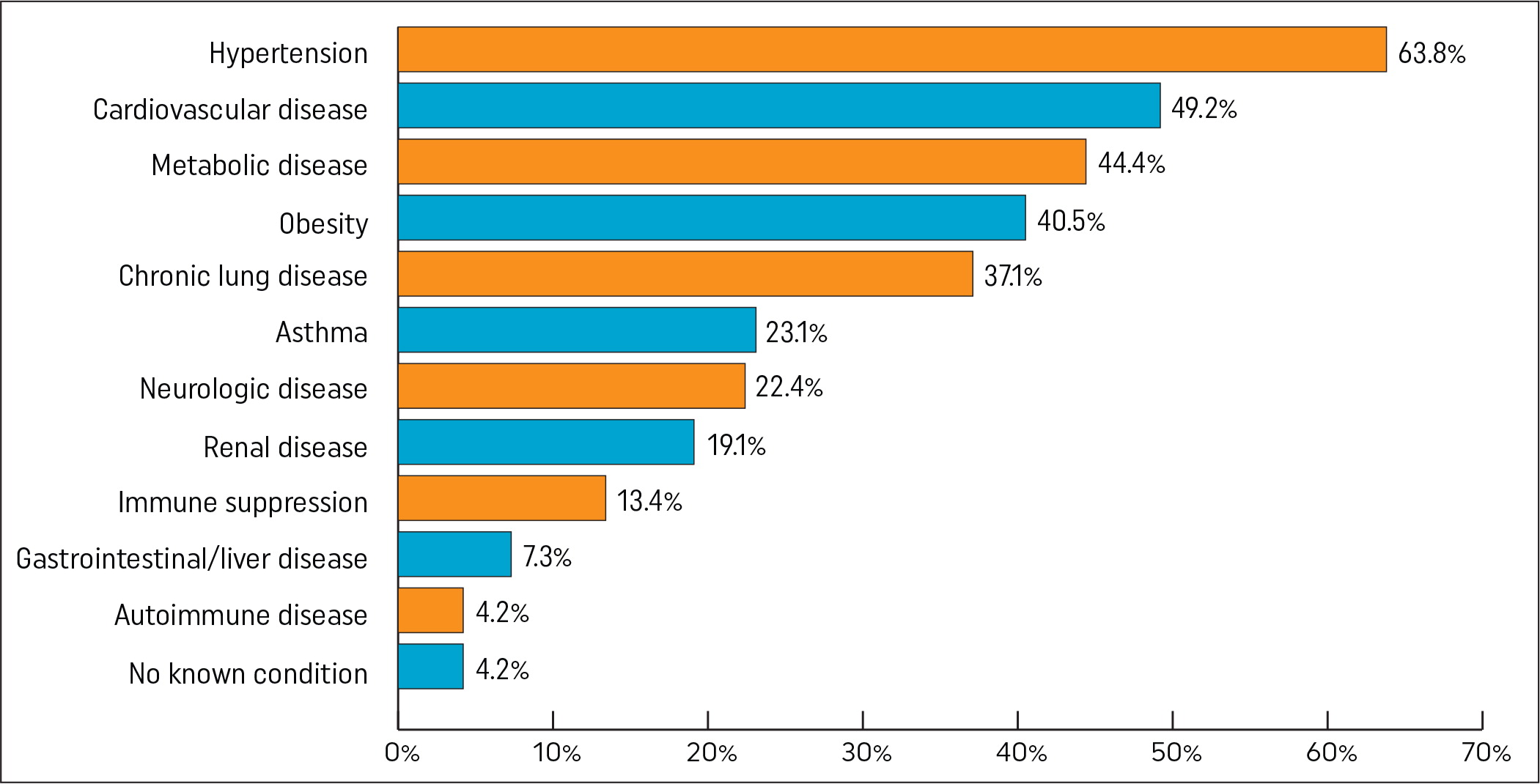
Multiple factors contribute to racial and ethnic disparities in flu vaccination and outcomes. Black, Hispanic, Native American, and other people of color disproportionately suffer from chronic illnesses, including diabetes, cardiovascular disease, kidney disease, and obesity,4 all of which increase vulnerability to influenza and hospitalization.5 Nine out of 10 people hospitalized with flu had at least one underlying health condition, with Figure 1 highlighting the medical conditions that most often lead to hospitalization when adults contract the flu.6
Experiences of discrimination and mistrust of medical professionals, reduced access to treatment, and various social determinants of health (SDoH) contribute to the disproportionate impact of cardiometabolic disease and other chronic conditions.7 These health conditions and social factors, in turn, lead to disparities in flu vaccination and worse health outcomes when those individuals contract the flu.
A national survey found that Black individuals are more likely to perceive higher risks of the side effects and greater barriers to receiving a flu vaccine; lower knowledge about it; and less likely to trust the flu vaccine and believe people close to them wanted them to get it. While these are discouraging, there were promising results from the survey, as 70% of Black individuals reported that public health guidelines are somewhat, fairly, or extremely important in determining whether they should get the flu vaccine. This suggests opportunities exist for health care team members and public health agencies to improve education and communication about flu vaccine effectiveness.
Still, structural and overt racism are intimately connected to the factors that lead to racial and ethnic health disparities. Racism translates into the experience of discrimination and resulting stress suffered by individuals, as well as inferior environments in which people live regarding healthy food access, personal safety, and access to nondiscriminatory, high-quality health care. Racism in the health care system manifests itself at the individual level, through implicit bias, and at the system level, through structural factors such as resource allocation.9 This all results in less trust in the health system and less equitable access to care for individuals who need it most.
Family Physicians Can Drive Health Equity
Family physicians already play an essential role in promoting health equity, providing the most health care across the lifespan to underserved populations in the United States and treating a more diverse population of patients than any other medical specialty.10 This fact led one group of primary care leaders to conclude that “health equity must be the foundation of the future of primary care.”11 They promoted the ideals of enhanced attention to patient convenience, cultural humility, structural competency, community engagement, and collaboration.
Community engagement is a crucial ingredient of health equity promotion. Leaders and influential community members, such as family physicians, pastors, stylists, barbers, and other leaders in schools, media outlets, civic organizations, and social clubs, understand their communities and are trusted voices to their members. Multiple studies have found that churches and other community strongholds can effectively partner with health care teams to promote vaccination and address other health issues important to underserved communities, such as cardiovascular disease, diabetes, lupus, and cancer screenings.12–16
Sustained engagement between community members and trusted leaders offers an opportunity to better understand community needs about various health issues, including local access to vaccines and other services, access to resources to meet SDoH needs, and advocacy for the community's health. Ultimately, this sustained relationship can translate into increased trust and health promotion in underserved communities of color.8
Addressing Disparity Gaps
Family physicians provide appropriate, compassionate, and knowledgeable health care for our patients, which requires being informed about what is important to them and their families. Determining what is important often involves understanding your patients' culture, language, and traditions. Consequently, emphasizing prevention, managing chronic conditions, and treating acute illnesses in a culturally and linguistically sensitive manner is a hallmark of our specialty.
With an increased focus in health care on illness and disease prevention, vaccinations have become a focal point in family physicians' efforts. Following the COVID-19 pandemic, maintaining up-to-date vaccination status was deemphasized for some patients, but it remains a vital practice for preventive medicine.
As discussed, flu vaccination rates have been historically lower for minority and underserved patients. Lower rates may be partly due to distrust, mistreatment, and barriers to vaccine access. Those patients' understanding of the history of the mistreatment of Black individuals may include their knowledge of the Tuskegee syphilis experiment, which involved following untreated Black men with syphilis to document the course of the disease.17 There is also the knowledge of J. Marion Simms performing gynecologic surgeries on enslaved women without anesthesia to document differences in how Black and white people experienced pain.18 These are just a couple of notable stories, with many other similar shameful stories in medicine's history.
In addition, many minority and underserved patients may lack a medical home or usual source of care. Lack of a medical home may be due to no insurance coverage or lower income. The often-episodic nature of their interface with the health care system may mean they seek health care only when they are required or emergencies arise and don't participate as actively in preventive care as patients not facing these barriers.
As a family physician, your patient may be one you have provided care for decades or one you're seeing for the first time. Regardless of the circumstance, we must never pass on an opportunity to discuss prevention. For many minority patients with poorly controlled hypertension, a significant prevention measure includes flu vaccination, especially for heart disease and stroke risk. For example, patients with a recent acute coronary syndrome (ACS) have a more than 50% risk reduction of cardiovascular death after receiving seasonal influenza vaccination.19
As health providers, we may perceive receiving the flu vaccine as routine care, but failure to receive it is often not the patient's choice alone. Studies have consistently shown a relationship between socioeconomic status and influenza immunization rates in many high-income countries, as patients with lower income levels receive the flu vaccine at lower rates than individuals with higher income levels.20 All patients should receive the recommendation, but family physicians may want to emphasize recommending the flu vaccine to lower-income patients.
Likewise, it behooves us as family physicians always to be aware of the clinical season and which viruses may be circulating in and around our communities. Influenza is an acute respiratory infection with variable degrees of systemic symptoms, including fever, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, fatigue, vomiting, and diarrhea.21 Even though influenza can present with wide-ranging symptomology, some studies estimate as high as 28% of influenza-infected patients are asymptomatic.22
Of the four types of influenza viruses, types A and B are responsible for the yearly epidemics of respiratory disease and, occasionally, pandemics.23–25 Influenza is transmitted mainly via respiratory droplets but may also be transmitted by direct contact with an infected person or indirect contact via surfaces. It is important to remind and emphasize safety measures to all our patients regarding viral infections, such as covering their mouths when they cough or sneeze, hand washing, and mask-wearing (when appropriate), to protect themselves and the most vulnerable members of their communities.
Protecting High-risk Groups
As family physicians often experience, most individuals with uncomplicated influenza have mild, self-limiting illness and recover in less than two weeks. However, for some patients, particularly those in high-risk groups, influenza can lead to hospitalization from more severe complications, including myocarditis, encephalitis, rhabdomyolysis,26 sinusitis, pneumonia, myositis, respiratory and kidney failure, sepsis, and possibly even death.27 Individuals in high-risk groups include the following28:
Adults 65 years and older
Children younger than 2 years
Patients with asthma
Patients with neurologic and neurodevelopment conditions
Patients with blood disorders
Patients with chronic lung disease
Patients with endocrine disorders
Patients with heart disease
Patients with kidney disease
Patients with liver disorders
Patients with metabolic disorders
People who are obese with a body mass index (BMI) of 40 or higher
People younger than 19 years on long-term aspirin- or salicylate-containing medications
People with a weakened immune system
People who have had a stroke
Chronic health problems can be exacerbated when certain individuals are infected with influenza. This is not an exhaustive list, but the following health problems can worsen when contracting influenza: emphysema, chronic bronchitis, asthma, ischemic heart disease, and congestive heart failure.27 Along with these health issues, individuals with the following pre-existing medical conditions are at increased risk of influenza-related complications: conditions that compromise airway clearance, asthma, chronic pulmonary, kidney or heart disease, immunosuppression, long-term aspirin therapy in patients younger than 19 years, metabolic disorders, obesity, sickle cell anemia, and other hemoglobinopathies.
Other groups considered to be at high risk include non-Hispanic Black persons, Hispanic or Latino persons, American Indians and Alaska Natives, people who live in long-term care facilities, children younger than 5 years, and post-partum women.23,28,29 According to the Centers for Disease Control and Prevention (CDC), racial and ethnic minority groups have historically and continue to experience lower influenza vaccination coverage, higher rates of severe influenza, and higher rates of hospitalization due to the flu compared to white individuals.30
Given the different iterations of COVID-19 variants causing increasing respiratory and other symptoms, it has become increasingly important to encourage patients at risk and their families to get influenza vaccination as a first line of defense. Many of the same patients described above are at increased risk of infection and complications from COVID-19 variants as they emerge. Consequently, emphasizing the benefits of prevention by receiving up-to-date vaccinations for influenza, COVID-19, and respiratory syncytial virus (RSV) should play a significant role in our discussions about seasonal defenses leading to healthy outcomes.27
Diagnostic Testing
Given that there may be overlapping symptoms between influenza and COVID-19, diagnostic testing may be necessary to inform earlier treatment decisions. Swab-based screening tests now can screen for influenza A and B and COVID-19. Rapid influenza diagnostic tests (RIDTs) identify influenza A and B viral nucleoprotein antigens in respiratory secretions and are commonly available for patients at an increased risk of complications.31 They are relatively inexpensive and may aid in early treatment decisions. However, while RIDTs are fast and convenient, they can often produce false-negative results. Reverse transcription PCR (RT-PCR) is considered by many to be the gold standard for influenza testing, but they have the downside of being more expensive.31–33
The good news is that rapid tests for early detection of influenza and other respiratory viruses are changing, with newer tests gaining U.S. Food and Drug Administration (FDA) approval at faster rates. It would be best to check with your laboratory that provides routine studies to see what they might find effective in your community.
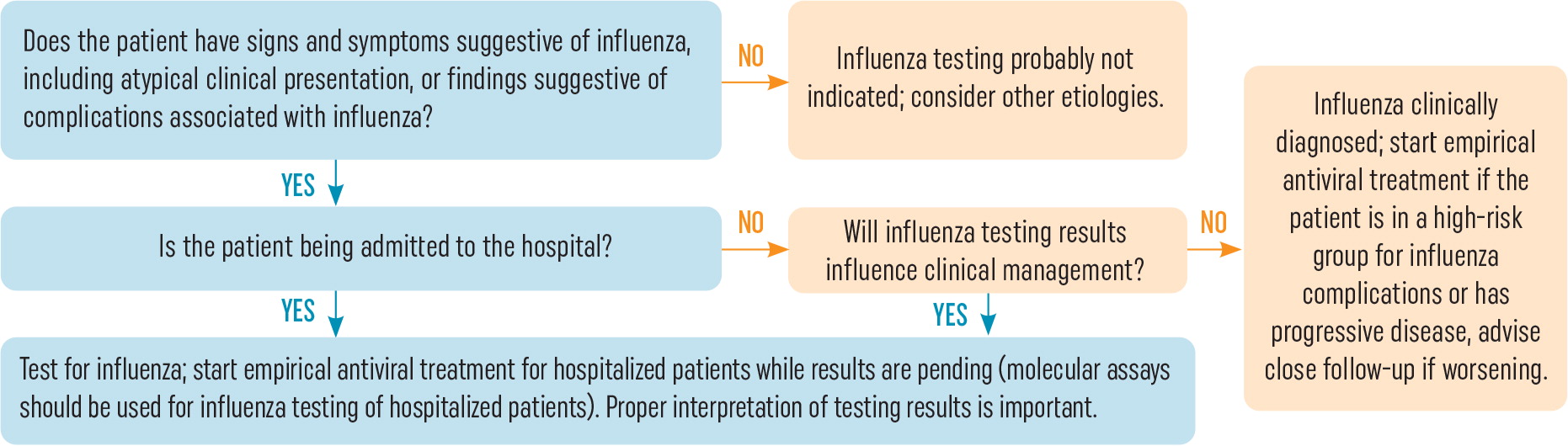
For patients who are significantly symptomatic or require hospitalization, Figure 2 offers guidance for initiating antiviral testing, treatment, and planning potential admission or coordinating admission with another physician.
Call to Action
It is critical to educate patients that influenza vaccinations are essential to protect against serious respiratory infectious diseases. Family physicians are the most valued and trusted sources of health information for their patients. While many patients believe that vaccines are essential, during the COVID-19 pandemic, many others expressed skepticism, were concerned, and became hesitant about all vaccines.
Assisting family physician practices and other point-of-care health care providers to improve influenza vaccination rates for underserved and vulnerable populations is an American Academy of Family Physicians (AAFP) priority. Family physicians are critical in promoting health equity and providing health care across the lifespan to underserved populations. To achieve the goals of improving equitable influenza vaccination rates for underserved and vulnerable populations, the AAFP recommends that family physicians:
Recommend and/or administer influenza vaccinations during all patient visits (i.e., routine well, annual health check-ups, etc.).
Recommend and/or administer age-appropriate annual influenza vaccinations to all your patient populations.
Ensure that vulnerable and underserved populations 65 years and older are recommended and/or administered any higher dose or adjuvanted influenza vaccine.
Prioritize recommending influenza vaccinations to lower-income patients.
Educate physicians and health care teams about the SDoH factors that contribute to suboptimal influenza vaccination uptake.
Address misinformation and myths while understanding your patient population's culture, language, and traditions.
Engage and educate communities about various health issues and encourage influenza vaccinations in community settings.
Family physicians must clearly communicate to all patient populations that influenza vaccinations are safe and effective, and their protection maximizes immunity and minimizes the burden and impact of infectious diseases. These actions and following the AAFP's recommendations can help reduce racial and ethnic disparities and improve vaccination uptake while closing many patient knowledge gaps when seeking preventive care and the protections that vaccinations provide.
Resources
The publication of this AAFP supplement is funded by an unrestricted grant from Sanofi Pasteur Inc.
