
The coming HCC overhaul will increase the importance of accurate and precise diagnosis coding to fully capture patients' health risks.
Fam Pract Manag. 2023;30(6):6-12
Author disclosures: no relevant financial relationships.

The Centers for Medicare & Medicaid Services (CMS) is updating its patient risk scoring system in 2024 in a way that will change payments that are based on hierarchical condition category (HCC).
The current HCC model was developed when the health care system used ICD-9 diagnosis codes. On Jan. 1, CMS will begin transitioning payment to a new system based on ICD-10-CM codes, as well as revise which diagnoses result in HCCs that carry increased payments.1 CMS says its new model “reflects more current costs associated with various diseases, conditions, and demographic characteristics.”2 But the changes will likely downgrade some patients' risk adjustment factors (RAFs), which could lower payments for practices that participate in capitated payment plans through either Medicare Advantage or private payers who use the CMS risk adjustment methodology. The change from the current system (Version 24, or “V24”) to the new system (“V28”) drew objections from a coalition of medical groups during the public comment period,3 but CMS is moving forward, albeit with a three-year phase-in (CMS is already using the new model but will base only 33% of payment on it in 2024).
Overall, CMS is predicting that RAF scores will drop by about 3% when the phase-in period is complete,4 but for some practices it could be more. It all depends on your patient panel and the prevalence of certain high-risk conditions within it. For practices that participate in capitated payment programs based on HCCs, the new model will increase the importance of accurate, precise, specific diagnosis coding to fully capture patient risk. That should not only result in payments that more accurately reflect risk, but it can also help practices identify which patients need more care or outreach to avoid hospitalizations or poor health outcomes.
This article provides a brief refresher on HCCs and a summary of what changes are likely to be weightiest for family medicine.
KEY POINTS
The Centers for Medicare & Medicaid Services is overhauling its hierarchical condition category (HCC) payment model to better reflect ICD-10 diagnosis coding versus ICD-9.
When fully phased in, the changes will decrease patient risk adjustment factor scores by an estimated 3%, reducing payments to practices that participate in capitated payment models based on risk.
Practices can ameliorate the effects of the changes by using the most precise, specific diagnosis codes possible to fully capture patient risk
WHAT ARE HCCS AND HOW DO THEY GET CAPTURED?
HCCs are categories of diagnosis codes, assigned a numerical score (known as a “coefficient value”) related to how much the diagnosis is associated with future financial risk. HCCs provide a snapshot of the overall severity of a patient's medical conditions that health plans combine with age and other demographic information to estimate patients' future health care costs.5 This combination of HCC scores and demographic risk factors creates a RAF score, which is then used to determine per-patient payments in capitated value-based payment arrangements. All ICD-10 codes map to an HCC, but only a little more than 10% map to “payment HCCs” that increase the amount paid.6 Examples of ICD-10 codes mapped to payment HCCs include E11.65 for type 2 diabetes with hyperglycemia and I11.0 for hypertension with congestive heart failure.
The payment revisions that start Jan. 1 are based in part on a clinical reclassification of the HCCs. CMS conducted a review of conditions coded more often in Medicare Advantage compared to fee-for service plans and removed more than 2,000 diagnostic codes from the V24 HCC model when developing V28.3 These eliminations included some diagnosis codes frequently used in family medicine (see “Examples of common codes no longer in payment HCC model”), causing consternation among commenters who feared that eliminating them from HCCs could have negative health impacts, particularly when it comes to slowing disease progression.7 But CMS said the move to an ICD-10-based system allows for more specificity in diagnosis coding, and the revisions mainly reflected the removal of codes that were non-specific and did not accurately predict cost.8
EXAMPLES OF COMMON ICD-10 CODES NO LONGER IN PAYMENT HCC MODEL
Malnutrition (E44.1)
Secondary thrombophilia (D68.69)
Depression in remission (F32.5)
Mild depression (F32.0/F33.0)
Coronary artery disease with angina (I25.118)
Aortic aneurysm without rupture (I71.x)
Aortic atherosclerosis (I70.0)
Practices should educate physicians about the changes and ensure the new HCCs are uploaded and active in their EHR.
Though the HCCs have changed, the strategies for capturing risk stay the same:5
Be specific: avoid using symptom codes or unspecified codes when you can use a more specific diagnosis code,
Try to capture patients' ongoing diagnoses annually,
Include codes for complications and secondary diagnoses (especially during annual wellness visits),
Make sure your documentation supports the diagnosis codes you use,
Don't use “history of” diagnosis codes for conditions you're actively treating,
Take advantage of diagnosis code specificity tools if your EHR has them.
Although fewer diagnosis codes map to “payment HCCs” in V28 (7,770 compared to 9,797 in V24), the new model actually increases the number of payment HCCs from 86 to 115, because of the increased specificity of the new model. Understanding these new categories will be important for value-based payment.
With the addition of almost 30 new payment HCCs, most of the HCCs were renumbered, even if the disease group itself did not have any other changes. In HCCs whose names and numbers did not change, there still may be changes to individual diagnoses mapped to them. It's complex, but the changes most relevant to primary care physicians are highlighted below.
CHANGES MOST RELEVANT TO PRIMARY CARE
While many disease groups see an expansion of their HCC codes in V28 (and a few will see a contraction), perhaps the group of most note is diabetes.
The Diabetes Disease Group expands from three HCCs to four, as CMS adds a new one for pancreas transplant status (HCC 35), which will move to the top of the diabetes HCC payment hierarchy in V28. Two of the three existing categories see their names change. The “acute complication” category becomes “diabetes with severe acute complications,” and the “diabetes without complication” category becomes “diabetes with glycemic, unspecified, or no complications.” “Diabetes with chronic complications” keeps the same name in V28 (HCC 37).
Notably, diabetes is one of two disease groups (congestive heart failure is the other) in which HCCs are “constrained” (as CMS calls it) in V28, meaning that all diabetes HCCs (excluding pancreas transplant status) carry the same weight, regardless of complications. (See “Constraining of diabetes HCCs.”) Two of the three diabetes HCCs will have a significantly lower coefficient value, which could have a major financial impact on practices that care for a lot of patients with diabetes.
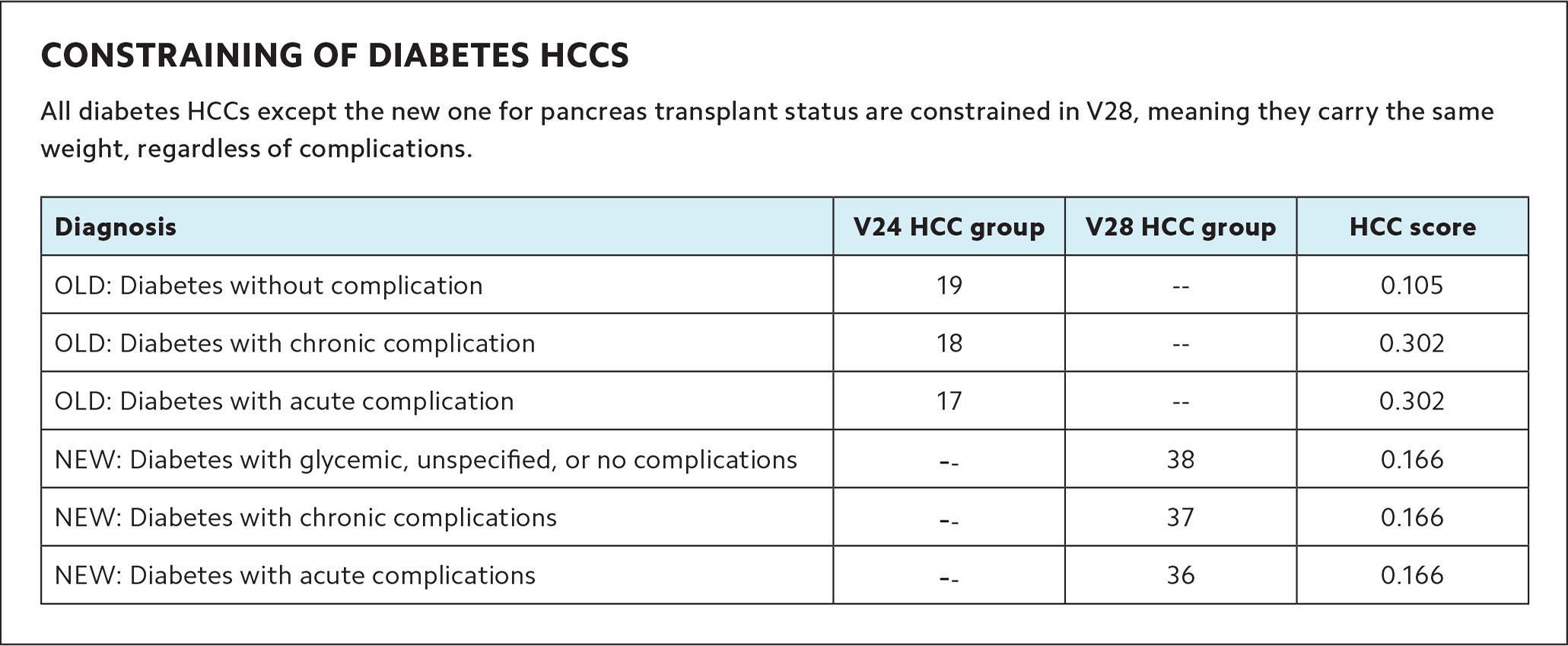
| Diagnosis | V24 HCC group | V28 HCC group | HCC score |
|---|---|---|---|
| OLD: Diabetes without complication | 19 | -- | 0.105 |
| OLD: Diabetes with chronic complication | 18 | -- | 0.302 |
| OLD: Diabetes with acute complication | 17 | -- | 0.302 |
| NEW: Diabetes with glycemic, unspecified, or no complications | -- | 38 | 0.166 |
| NEW: Diabetes with chronic complications | -- | 37 | 0.166 |
| NEW: Diabetes with acute complications | -- | 36 | 0.166 |
Here is an example from an analysis of how a patient's RAF score will change under V28.9 The patient is 70–74 years old, and has diabetes mellitus with peripheral artery disease, malnutrition, atrial fibrillation, toe amputation status, and heart failure with reduced ejection fraction. In HCC V24, this patient's RAF score would have been 2.446, because each of the conditions/complications increased the HCC score. But in V28, the same patient's RAF score is only 1.014, largely because malnutrition has been eliminated from HCC weighting, and peripheral artery disease and toe amputation have been rolled into the diabetes code.
The Gastrointestinal (GI) Disease Group expands from three HCCs to five in V28. The group maintains two existing HCCs (intestinal obstruction/perforation and chronic pancreatitis) and adds a new one (HCC 77) for intestine transplant status with complications. Also, the inflammatory bowel disease HCC from V24 is split into two more specific HCCs in V28 for Crohn's disease and ulcerative colitis (see “New and updated HCC groups”).
NEW AND UPDATED HCC GROUPS
The Centers for Medicare & Medicaid Services is adding or updating dozens of hierarchical condition categories (HCCs) in its new HCC model, V28. Here are some key payment HCCs that are important to primary care.
Diabetes Disease Group
NEW
- HCC 35 (Pancreas Transplant Status)
UPDATED
- HCC 36 (Diabetes With Severe Acute Complications)
- HCC 38 (Diabetes With Glycemic, Unspecified, or No Complications)
Gastrointestinal Disease Group
UPDATED
- HCC 77 (Intestine Transplant Status/Complications)
NEW
- HCC 80 (Crohn's Disease [Regional Enteritis])
- HCC 81 (Ulcerative Colitis)
Musculoskeletal Disease Group
UPDATED
- HCC 92 (Bone/Joint/Muscle/Severe Soft Tissue Infections/Necrosis)
- HCC 93 (Rheumatoid Arthritis and Other Specified Inflammatory Rheumatic Disorders)
NEW
- HCC 94 (Systemic Lupus Erythematosus and Other Specified Systemic Connective Tissue Disorders)
Blood Disease Group
ALL NEW OR UPDATED
- HCC 107 (Sickle Cell Anemia [Hb-SS] and Thalassemia Beta Zero)
- HCC 108 (Sickle Cell Disorders, Except Sickle Cell Anemia [Hb-SS] and Thalassemia Beta Zero; Beta Thalassemia Major)
- HCC 109 (Acquired Hemolytic, Aplastic, and Sideroblastic Anemias)
- HCC 111 (Hemophilia, Male)
- HCC 112 (Immune Thrombocytopenia and Specified Coagulation Defects and Hemorrhagic Conditions)
- HCC 114 (Common Variable and Combined Immunodeficiencies)
- HCC 115 (Specified Immunodeficiencies and White Blood Cell Disorders)
Cognitive Disease Group
UPDATED
- HCC 125 (Dementia, Severe)
- HCC 126 (Dementia, Moderate)
- HCC 127 (Dementia, Mild or Unspecified)
Substance Use Disorder Disease Group
NEW
- HCC 135 (Drug Use With Psychotic Complications)
- HCC 136 (Alcohol Use With Psychotic Complications)
- HCC 137 (Drug Use Disorder, Moderate/Severe, or Drug Use With Non-Psychotic Complications)
- HCC 138 (Drug Use Disorder, Mild, Uncomplicated, Except Cannabis)
- HCC 139 (Alcohol Use Disorder, Moderate/Severe, or Alcohol Use With Specified Non-Psychotic Complications)
Psychiatric Disease Group
NEW
- HCC 153 (Personality Disorders; Anorexia/Bulimia Nervosa)
UPDATED
- HCC 152 (Psychosis, Except Schizophrenia)
- HCC 154 (Bipolar Disorders Without Psychosis)
- HCC 155 (Major Depression, Moderate or Severe, Without Psychosis)
Heart Disease Group
NEW
- HCC 221 (Heart Transplant Status/Complications)
- HCC 222 (End-Stage Heart Failure)
- HCC 223 (Heart Failure with Heart Assist Device/Artificial Heart)
- HCC 224 (Acute on Chronic Heart Failure)
- HCC 225 (Acute Heart Failure [Excludes Acute on Chronic])
- HCC 226 (Heart Failure, Except End-Stage and Acute)
- HCC 227 (Cardiomyopathy/Myocarditis)
Vascular Disease Group
NEW
- HCC 267 (Deep Vein Thrombosis and Pulmonary Embolism)
Lung Disease Group
NEW
- HCC 276 (Lung Transplant Status/Complications)
- HCC 279 (Severe Persistent Asthma)
UPDATED
- HCC 278 (Idiopathic Pulmonary Fibrosis and Lung Involvement in Systemic Sclerosis)
- HCC 280 (Chronic Obstructive Pulmonary Disease, Interstitial Lung Disorders, and Other Chronic Lung Disorders)
- HCC 283 (Empyema, Lung Abscess)
Neoplasm Disease Group
UPDATED
- HCC 17 (Cancer Metastatic to Lung, Liver, Brain, and Other Organs; Acute Myeloid Leukemia Except Promyelocytic)
- HCC 18 (Cancer Metastatic to Bone, Other and Unspecified Metastatic Cancer; Acute Leukemia Except Myeloid)
- HCC 19 (Myelodysplastic Syndromes, Multiple Myeloma, and Other Cancers)
Metabolic Disease Group
NEW
- HCC 49 (Specified Lysosomal Storage Disorders)
UPDATED
- HCC 50 (Amyloidosis, Porphyria, and Other Specified Metabolic Disorders)
- HCC 51 (Addison’s and Cushing’s Diseases, Acromegaly, and Other Specified Endocrine Disorders)
Liver Disease Group
NEW
- HCC 62 (Liver Transplant Status/Complications)
- HCC 68 (Cholangitis and Obstruction of Bile Duct Without Gallstones)
Neurological Disease Group
UPDATED
- HCC 191 (Quadriplegic Cerebral Palsy)
- HCC 192 (Cerebral Palsy, Except Quadriplegic)
- HCC 193 (Chronic Inflammatory Demyelinating Polyneuritis and Multifocal Motor Neuropathy)
- HCC 195 (Myasthenia Gravis with [Acute] Exacerbation)
- HCC 196 (Myasthenia Gravis without [Acute] Exacerbation and Other Myoneural Disorders)
- HCC 199 (Parkinson and Other Degenerative Disease of Basal Ganglia)
- HCC 200 (Friedreich and Other Hereditary Ataxias; Huntington Disease)
The Musculoskeletal Disease Group expands from two HCCs to three. The addition is due to the rheumatoid arthritis and inflammatory connective tissue disease category being separated into two HCCs in V28, due to clinical severity and course and related spending:
- HCC 93 for rheumatoid arthritis and other specified inflammatory rheumatic disorders,
- HCC 94 for systemic lupus erythematosus and other specified systemic connective tissue disorders.
The Blood Disease Group has undergone significant changes in V28, expanding from three HCCs to seven. The group's three broad HCCs (severe hematological disorders, disorders of immunity, and coagulation defects and other specified hematological disorders) have been separated into seven more specific categories.
“Disorders of Immunity” will be separated into two HCCs:
- HCC 114 (Common Variable and Combined Immunodeficiencies), and
- HCC 115 (Specified Immunodeficiencies and White Blood Cell Disorders).
This will allow clinicians to separate the more clinically severe common variable and combined immunodeficiencies from other specified immunodeficiencies and white blood cell disorders, while unspecified, non-specific, and lower-severity immune disorders will be mapped to a non-payment HCC.
“Severe Hematological Disorders” in V24 will expand to four different HCCs in V28:
- HCC 107 (Sickle Cell Anemia [Hb-SS] and Thalassemia Beta Zero),
- HCC 108 (Sickle Cell Disorders, Except Sickle Cell Anemia [Hb-SS] and Thalassemia Beta Zero; Beta Thalassemia Major)
- HCC 109 (Acquired Hemolytic, Aplastic, and Sideroblastic Anemias) and
- HCC 111 (Hemophilia, Male).
Additionally, V28 will add specificity to the “Coagulation Defect and Other Specified Hematologic Disorders” category, which will become the new HCC 112 for “Immune Thrombocytopenia and Specified Coagulation Defects and Hemorrhagic Conditions.” Other or unspecified conditions in this category will be mapped to a non-payment HCC.
The Cognitive Disease Group expands from two HCCs to three in V28. In the V24 model, cognitive disease had one HCC for dementia with complications and one for dementia without complications. The updated V28 model has three: HCC 125 for severe dementia, HCC 126 for moderate dementia, and HCC 127 for mild or unspecified dementia.
The Substance Use Disorder Disease Group expands from three HCCs to five in V28. The V24 model combined all substance use into three broad HCCs. V28 has separate HCCs for drug use or alcohol use, either with or without psychosis. “With psychosis” diagnoses are at the top of the risk hierarchy.
The Psychiatric Disease Group adds one HCC and has several changes to existing HCCs in V28. The HCC for reactive and unspecified psychosis has been reconfigured to “psychosis, except schizophrenia” (HCC 152). Several diagnoses clinically consistent with non-schizophrenic psychosis were added to this HCC (e.g., delusional disorders; manic and depressive [bipolar] disorders, severe, with psychotic behavior; and major depressive disorder, severe, with psychotic features).
Personality disorders (HCC 153) move up the payment hierarchy in V28 because of their higher associated costs. Anorexia/bulimia have been added to this HCC for the same reason.7
The last change in this disease group is the splitting of V24's “major depressive, bipolar, and paranoid disorders” HCC into two separate HCCs: one for bipolar disorders without psychosis (HCC 154) and one for moderate or severe major depression without psychosis (HCC 155). CMS removed psychosis from these two categories because it has its own HCC in V28 (HCC 152). The agency separated bipolar disorder from major depression because of its greater clinical severity.
Probably most important for outpatient primary care, any codes for psychiatric diagnoses that are mild, unspecified, in remission, subsequent encounter, and sequela are mapped to non-payment HCCs in V28.7
The Heart Disease Group expands from five HCCs to 10 to add granularity to heart failure and other chronic cardiac conditions. V28 separates cardiomyopathy and all heart failure types and stages into five new codes:
- HCC 222 for end-stage heart failure,
- HCC 224 for acute on chronic heart failure,
- HCC 225 for acute heart failure, excluding acute on chronic,
- HCC 226 for heart failure, except end-stage and acute,
- HCC 227 for cardiomyopathy/myocarditis.
Of these, end-stage heart failure carries a higher payment than the others.
V28 also created two new HCCs for heart transplant status/complications and heart assist device/artificial heart. Only patients with heart failure (versus an acute condition) who are mapped to a heart failure HCC will also be mapped to the heart assist device/artificial heart HCC, if they have such a device. Coronary atherosclerosis remains non-payment in V28, but the more severe manifestations of unstable angina (HCC 229) and acute myocardial infarction (HCC 228) are payment HCCs. Another important change for outpatient primary care is that stable angina pectoris becomes a non-payment HCC in V28.
The Vascular Disease Group still has three HCCs, but they have changed. The number of diagnosis codes affiliated with the group increased to 365, allowing for more granularity in diagnosis. Codes that indicate more serious cases of vascular disease will remain in the payment HCCs, while “other” and “unspecified” diagnoses map to a non-payment HCC in V28. For example, codes for atherosclerosis with rest pain and with ulceration or gangrene usually indicate a more resource-intensive disease state, so they are mapped to an HCC at a higher payment level (HCC 263), while the broader “vascular disease” HCC in V24 has become a non-payment HCC in v28 and has been replaced with a new category (HCC 267) for deep vein thrombosis and pulmonary embolism. The category that includes atherosclerosis of arteries of the extremities, with intermittent claudication will become a non-payment HCC.
The Lung Disease Group expands from five HCCs to seven in V28, adding one for lung transplant status/complications (HCC 276) and one for severe persistent asthma (HCC 279), which was not previously a payment HCC diagnosis.
The Kidney Disease Group contracts from five HCCs to four. V28 has removed two HCCs for dialysis state and acute renal failure, and separated the Stage 3 chronic kidney disease (CKD) HCC into two different ones: HCC 328 for stage 3B moderate CKD and HCC 329 for stage 3 (except 3B) moderate CKD. This change is based on the increased granularity in ICD-10 for Stage 3 CKD. Chronic kidney staging is still used to define the HCC hierarchy for kidney disease, with Stage 5 at the top.
Dialysis status has been reclassified as a non-payment HCC in V28 because it captures transitory dialysis and, according to CMS, “the removal from payment allows the costs to flow through to actual conditions that created the need for dialysis, such as congestive heart failure or sepsis.”7 If dialysis is chronic, patients will have end-stage renal disease (ESRD) and will be under the ESRD model anyway. Acute renal failure was also reclassified as a non-payment HCC because it is considered transitory. If it is not transitory, patients will fall under the CKD HCCs.
The Neoplasm Disease Group will expand from five HCCs to seven as all metastatic cancers and acute leukemias (currently in one HCC) are separated into three distinct HCCs:
- HCC 17 (Cancer Metastatic to Lung, Liver, Brain, and Other Organs; Acute Myeloid Leukemia Except Promyelocytic),
- HCC 18 (Cancer Metastatic to Bone, Other and Unspecified Metastatic Cancer; Acute Leukemia Except Myeloid),
- HCC 19 (Myelodysplastic Syndromes, Multiple Myeloma, and Other Cancers).
The other four cancer HCCs (lung, lymphoma, bladder/colorectal, and prostate/breast) will carry over to V28 but get new numbers.
The Metabolic Disease Group will expand from three HCCs to four, with a new payment HCC added for specified lysosomal storage disorders because they have been deemed high cost based on Medicare Part B drug spending. Metabolic disorders and endocrine disorders will also be separated into two separate HCCs based on spending and clinical considerations:
- HCC 50 Amyloidosis, Porphyria, and Other Specified Metabolic Disorders, and
- HCC 51 Addison’s and Cushing’s Diseases, Acromegaly, and Other Specified Endocrine Disorders.
Morbid obesity remains as an HCC (HCC 48) but, as mentioned, protein-calorie malnutrition will be removed as a payment HCC.
The Liver Disease Group expands from three HCCs to five by maintaining its previous HCCs (end-stage liver disease, cirrhosis, and chronic hepatitis), and adding two in V28:
- HCC 62 (Liver Transplant Status/Complications)
- HCC 68 (Cholangitis and Obstruction of Bile Duct Without Gallstones).
The Neurological Disease Group will expand from eight HCCs to 12 as several conditions will be coded with more specificity in V28.
The V24 HCC code for “Myasthenia Gravis/Myoneural Disorders and Guillain-Barre Syndrome/Inflammatory and Toxic Neuropathy” will be separated into four HCCs in V28. Acute Guillain-Barre Syndrome will become a non-payment HCC, but if the condition becomes chronic it changes to payment HCC 193 for “Chronic Inflammatory Demyelinating Polyneuritis and Multifocal Motor Neuropathy.” Myasthenia gravis will be separated into two payments HCCs based on spending and clinical severity: HCC 195 for “Myasthenia Gravis with (Acute) Exacerbation” and HCC 196 for “Myasthenia Gravis without (Acute) Exacerbation and Other Myoneural Disorders.”
The V24 cerebral palsy HCC will also be separated into two HCCs in V28: HCC 191 for “Quadriplegic Cerebral Palsy” and HCC 192 for “Cerebral Palsy, Except Quadriplegic.”
The Parkinson’s and Huntington’s Diseases HCC from V24 will also be separated into two distinct HCCs in V28: HCC 199 for “Parkinson and Other Degenerative Disease of Basal Ganglia” and HCC 200 for “Friedreich and Other Hereditary Ataxias; Huntington Disease.”
FOR MORE INFORMATION
This summary does not provide information on all the new V28 HCCs or delve into the ICD-10-to-HCC mappings for the revised model. A side-by-side comparison of all the new V28 HCCs codes and their V24 counterparts is available in the CMS advance notice published Feb. 1.8 The CMS risk adjustment webpage also includes proposed ICD-10-to-HCC mapping information available to download to further help practices navigate these significant HCC changes.10
