
Supplement sponsor: American Academy of Family Physicians
Fam Pract Manag. 2023;30(6):13-18
A Guide to Relieving Administrative Burden is a series of supplements developed by the American Academy of Family Physicians (AAFP) to provide information about innovations proven to relieve administrative burden and optimize your family medicine experience. It is based on AAFP Innovation Labs conducted with physicians like you, as well as a comprehensive literature review. Whether you have a solo practice or are an employee of a large health system, the guide will help you consider and adopt proven innovations.
This is the second supplement in the series. It describes key AAFP advocacy efforts and techniques, technologies, and transformations to help reduce your prior authorization burden without compromising patient care.
Introduction
Prior authorization (PA) is a cost-control tool that requires payer approval before an order for a service or prescription is covered. The process is costly, inefficient, and opaque, and it is a leading cause of administrative burden for family physicians that continues to be overused and abused. In fact, a 2022 American Medical Association (AMA) survey found that 88% of surveyed physicians reported that PAs put a “high or extremely high” burden on their practice, with practices completing an average of 45 PAs per physician every week.1 This high volume of PAs requires physicians and their staff to take valuable time away from patient care to make phone calls, wait on hold, obtain and fill out forms, collect and submit medical documents, and appeal denials. Chief complaints about PA include the following:
It's still the bane of our existence.
My staff deals with it; it's a killer for them.
Our approval rate is 99.87%, and we still had to hire three additional full-time equivalents this year. It's very frustrating.
Why do I have to get prior auth again? It's a continuation of the same medication.
It takes 40 minutes to talk to someone after a denial.
For primary care practices, the median value of all the time spent interacting with health plans is nearly $48,000 per year per physician.2 The PA process also harms patients by delaying care and reducing adherence to treatment. Family physicians and their staff often bear the brunt of patients' frustration with PAs and the associated care delays.
Key Points
The burden associated with PA must be addressed with advocacy.
The AAFP strongly advocates for the automation and elimination of PA.
The techniques, technologies, and transformations outlined in this supplement can help reduce the burden.
The Prior Authorization Process
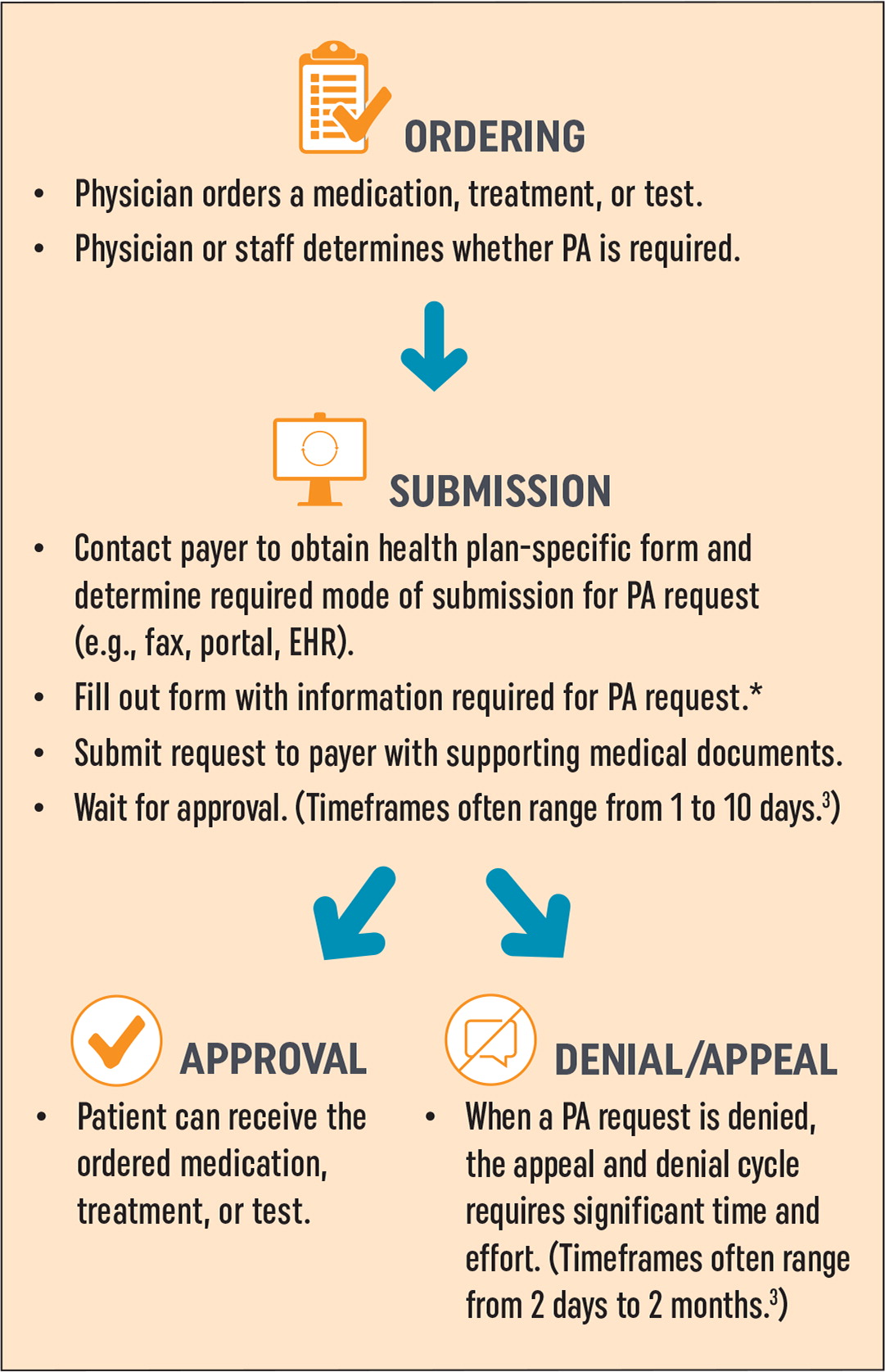
The phases of the PA process are ordering, submission, and approval or denial/appeal (Figure 1). Innovations can directly address issues in the submission phase to help reduce administrative burden for physicians and their staff. Much of the burden associated with the approval phase and the denial/appeal cycle is payer driven and must be addressed through advocacy and comprehensive policy reform. Technological innovations to streamline the entire PA process are evolving, but they have been focused on hospital and specialty practice revenue centers that offer high-cost diagnostic tests and therapeutics (e.g., cardiology practices, specialty testing labs). In most cases, primary care PAs are not associated with any practice revenue, so family medicine practices have not been a market for PA technology and service companies.
Impact of Prior Authorization
In December 2022, the AMA surveyed 1,001 practicing physicians regarding PA.1 Key findings from respondents included the following:
94% reported that PA delayed the start or continuation of necessary care.
88% reported that the burden associated with PA is high or extremely high for physicians and practice staff.
33% reported that a patient experienced a serious adverse event due to PA.
On average, physicians and practice staff spend about two days per week (14 hours) completing PAs.
In March 2023, the Medical Group Management Association (MGMA) surveyed executives representing 601 medical group practices regarding PA in Medicare Advantage (MA) plans.4 Key findings from respondents included the following:
97% reported that PA requirements resulted in care delays or denials.
84% reported an increase in PA requirements for MA in the last 12 months.
84% had to reauthorize existing Medicare-covered services when their patients switched plans.
72% had a required peer-to-peer discussion with a health plan clinician who was not from a relevant specialty.
Advocacy to Reduce Prior Authorization Burden
Streamlining and automating PA will not be enough to relieve the burden on family physicians and their patients. PA must be limited to far fewer products and services, and the process must be standardized and transparent.
AAFP Advocacy Goals
The AAFP fiercely drives efforts to reform PA and remains focused on enabling physicians and patients to have access to clear guidelines for PA requirements and timely responses from insurance plans. The following are key goals driving the Academy's advocacy to reduce PA burden.
PA and step therapy should be eliminated for the following5:
Physicians using appropriate clinical knowledge, training, and experience
Physicians in financial risk-sharing agreements
Physicians who have high approval rates (“gold carding”)
Services that are evidence-based standards of care
Services that are regularly approved
Medications that are standard, inexpensive, and generic
Durable medical equipment (DME) supplies for patients who have long-term or permanent chronic conditions
Patients who have a chronic disease that is under effective medication management
Patients already on a course of treatment under a previous plan
PA should be standardized across all payers in the following ways:
Require standard electronic prior authorization (ePA) application programming interface (API) for payers and electronic health records (EHRs)6
Standardize requests across the Centers for Medicare & Medicaid Services (CMS) and commercial payers5
Set response timeframes to 24 hours for urgent requests and 48 hours for nonurgent requests7
Attest that diagnosis is sufficient for medical necessity5
Payers should be fully transparent and provide access to the following7:
Patients' PA status (Note: This will help alleviate practice burden and prevent patients from blaming physicians and their staff for delays.)
Accurate, up-to-date formularies, drug tiers, and requirements for use of specific pharmacies
Alternative medications that do not require PA
Cost of medications, including out-of-pocket costs
Explanation of medical necessity determinations
Clinical criteria used for each denial
Coverage criteria summaries
AAFP Advocacy Win: 2024 Medicare Advantage and Part D Rule
Requires plans to only use PA to “confirm the presence of diagnoses or other medical criteria and/or ensure that an item or service is medically necessary,” not to delay or deter care.
Sets a minimum 90-day transition period for enrollees currently undergoing treatment who change to a new MA plan. During this period, the new plan cannot require PA for the active course of treatment.
Ensures that approval of a PA request for a course of treatment remains valid “for as long as medically reasonable and necessary to avoid disruptions in care in accordance with applicable coverage criteria, the patient's medical history, and the treating provider's recommendation.”
Requires all MA plans to establish a utilization management committee “to review policies annually and ensure consistency with traditional Medicare's national and local coverage decisions and guidelines.”
The Three T's for Addressing Prior Authorization Burden
In Tables 2, 3, and 4, you will find a list of techniques, technologies, and transformations for addressing PA burden that have been identified in the literature and by family physicians working with the AAFP Innovation Lab. A relative estimate of potential burden reduction and probable cost range for each innovation is also shown. Actual impact will vary based on the practice environment and the baseline level of burden associated with PA. More information about these innovations and others is available at aafp.org/simplification.
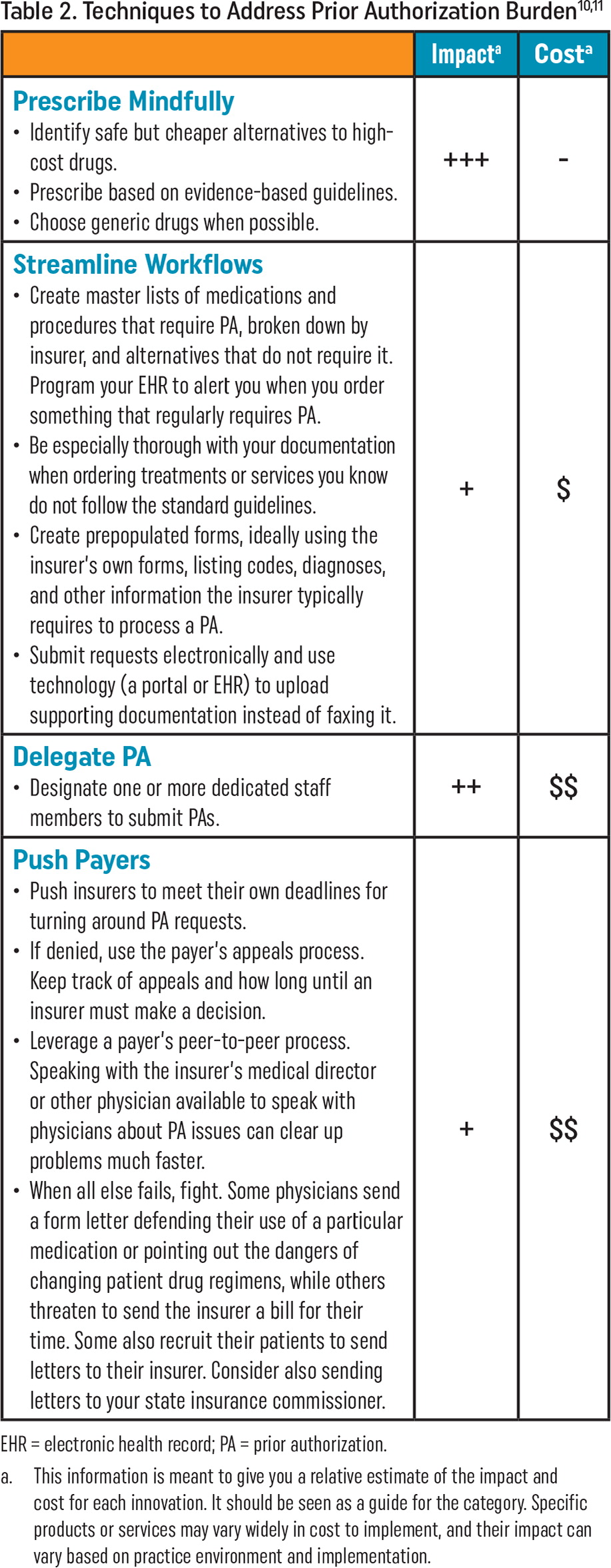
| Impacta | Costa | |
|---|---|---|
Prescribe Mindfully
| +++ | - |
Streamline Workflows
| + | $ |
Delegate PA
| ++ | $$ |
Push Payers
| + | $$ |
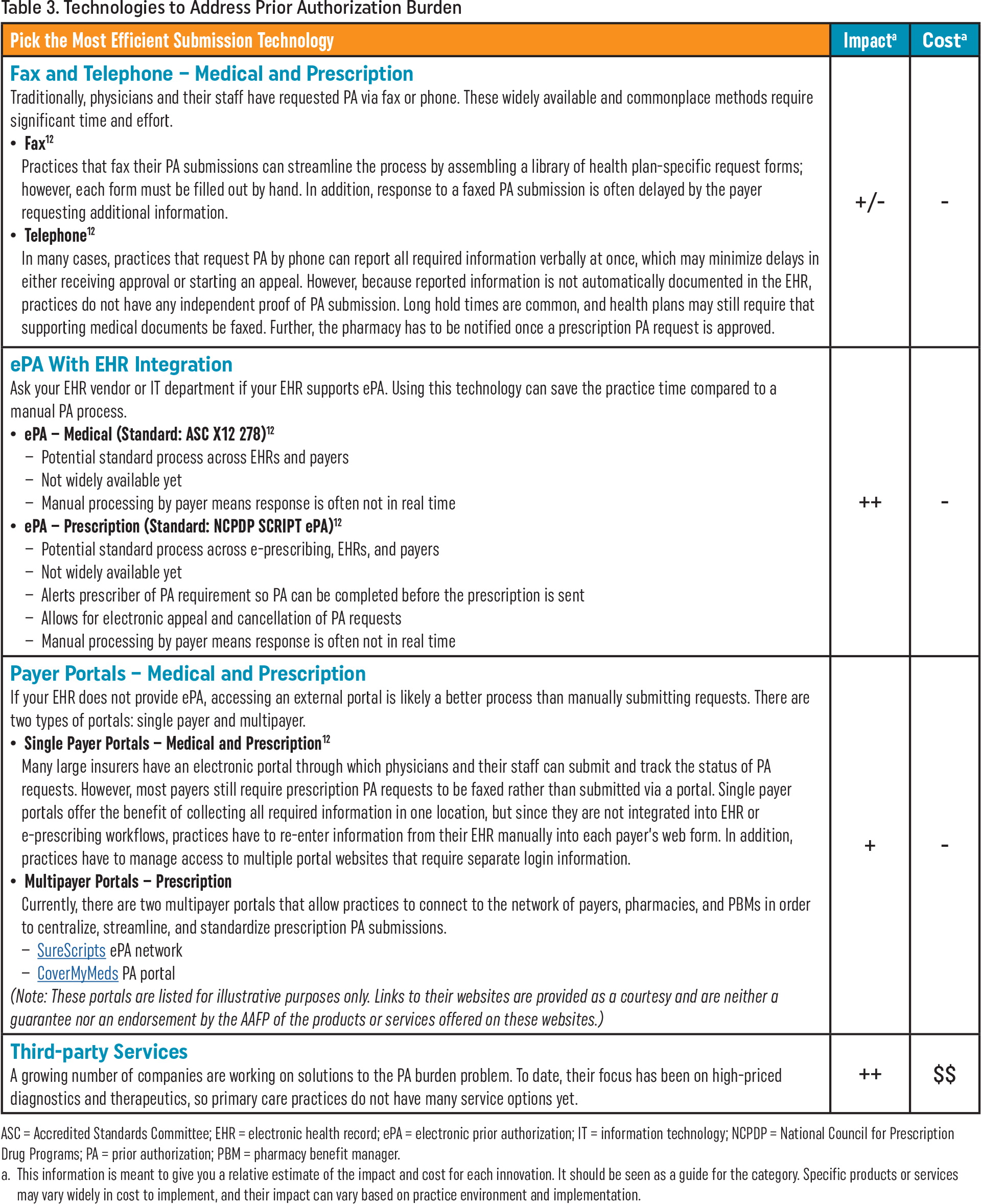
| Pick the Most Efficient Submission Technology | Impacta | Costa |
|---|---|---|
| Fax and Telephone – Medical and Prescription Traditionally, physicians and their staff have requested PA via fax or phone. These widely available and commonplace methods require significant time and effort.
| +/- | - |
| ePA With EHR Integration Ask your EHR vendor or IT department if your EHR supports ePA. Using this technology can save the practice time compared to a manual PA process.
| ++ | - |
| Payer Portals – Medical and Prescription If your EHR does not provide ePA, accessing an external portal is likely a better process than manually submitting requests. There are two types of portals: single payer and multipayer.
(Note: These portals are listed for illustrative purposes only. Links to their websites are provided as a courtesy and are neither a guarantee nor an endorsement by the AAFP of the products or services offered on these websites.) | + | - |
| Third-party Services A growing number of companies are working on solutions to the PA burden problem. To date, their focus has been on high-priced diagnostics and therapeutics, so primary care practices do not have many service options yet. | ++ | $$ |
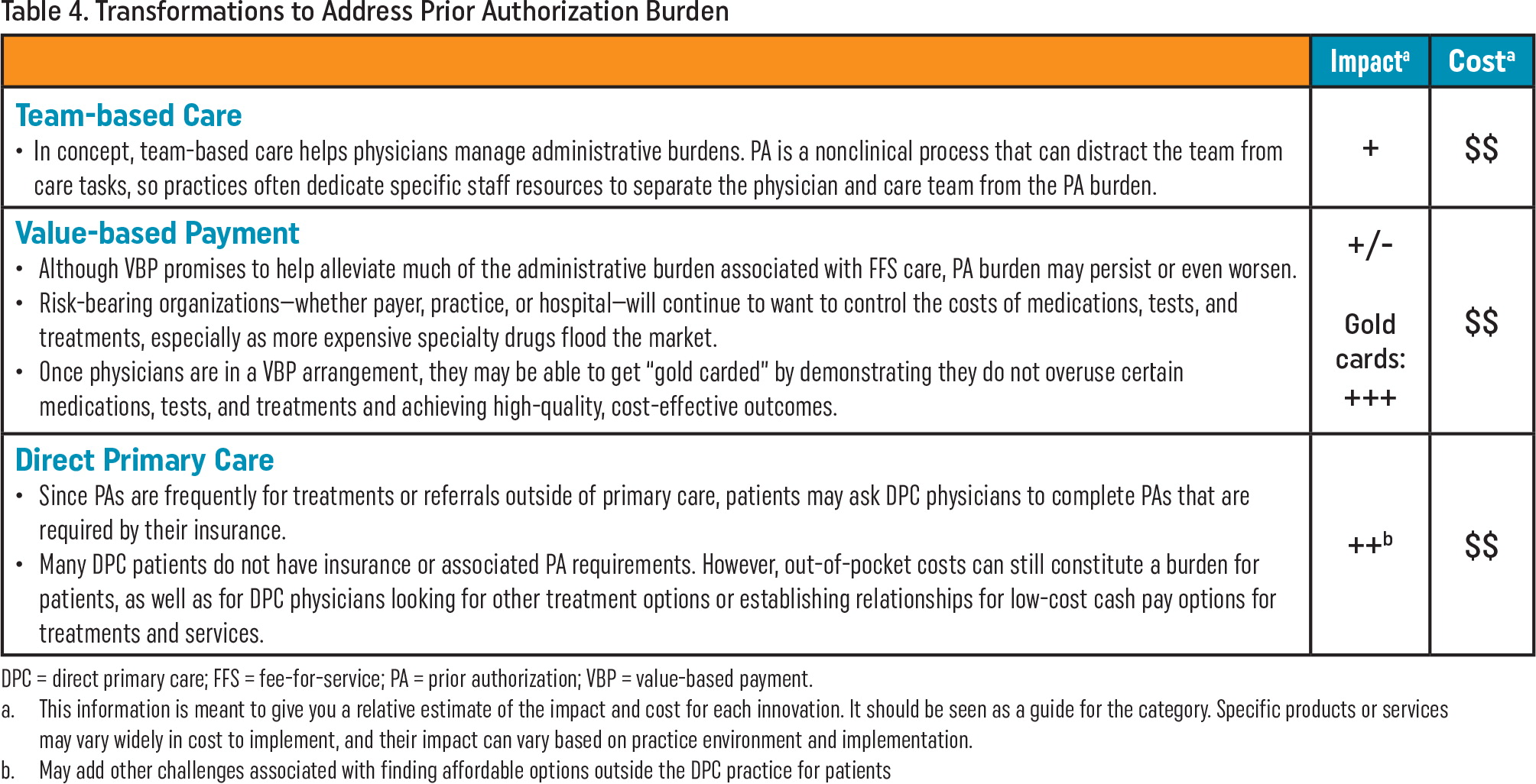
| Impacta | Costa | |
|---|---|---|
Team-based Care
| + | $$ |
Value-based Payment
| +/- Gold cards: +++ | $$ |
Direct Primary Care
| ++b | $$ |
Addressing the burden associated with PA requires significant advocacy efforts with the federal government, private payers, purchasers, and health information technology (IT) developers. The AAFP strongly advocates on behalf of its members in all of these arenas and will continue to do so. Adopting the techniques, technologies, and transformations outlined in this supplement can help family medicine practices reduce their PA burden. More work is needed to study the real-world impact of these innovations to help family physicians know what will truly work in their practices. The future holds great promise for the automation of PA through interoperability and the application of artificial intelligence, and the AAFP will continue to support advances in these areas.
The AAFP's Administrative Simplification webpage highlights the Academy's ongoing advocacy efforts and offers practice resources to help you take back your time and safeguard your well-being.
