
Fam Pract Manag. 2025;32(4):45-48
The publication of this content is funded by Abbott Diabetes Care and brought to you by the AAFP. Journal editors were not involved in the development of this content.
Primary care physicians and their teams are at the forefront of diabetes care in the United States. They are the first point of contact for most patients and provide continuous care for many adults with type 1 diabetes and an estimated 90% of all patients with type 2 diabetes.1 Their care is vital, as three-quarters of U.S. counties have no endocrinologist.2 With a lack of endocrinologists to treat many Americans with diabetes and the prevalence of the disease (e.g., about 1 in every 10 people in the United States has diabetes, and it is the eighth leading cause of death in the country),3 optimizing diabetes care by family and other primary care physicians is essential.
The evolution of assessing glycemia has progressed from urine glucose testing in the early 20th century into the 1960s, when blood glucose testing became available in physicians’ offices.4 In the 1980s, self-monitoring of blood glucose, or SMBG, became available to patients. Early glucose meters were cumbersome with limited accuracy. By 2004, a landmark advancement emerged when the first continuous glucose monitor, or CGM, was introduced. CGM measures interstitial glucose and consists of two basic types: those owned by the user providing real-time glucose data (i.e., personal CGM systems) and those owned by practices that can provide either blinded or unblinded data (i.e., professional CGM systems). CGM technology has progressed so that most do not require SMBG confirmation for treatment decisions, including insulin dosing.
The American Diabetes Association Standards of Care in Diabetes 2025 recommends routine use of real-time or intermittently scanned CGM for diabetes management in youth and adults on any type of insulin therapy, in addition to recommending it for adults with type 2 diabetes treated with glucose-lowering medications other than insulin.5 It is recommended to use as often as possible, with minimal gaps in usage. Intermittent or periodic use of personal or professional CGM for medication or lifestyle adjustment is recommended when consistent use of CGM is not feasible.
Despite the recommendations for CGM use, surveys estimate that only 38.6% of primary care clinicians6 and 44% of primary care nurse practitioners7 have ever prescribed CGM. Most frequently cited barriers to CGM implementation in primary care include insurance-related factors, such as limited insurance coverage, time-consuming prior authorization processes, extensive required documentation and prohibitive out-of-pocket costs to patients.8
The American Academy of Family Physicians conducted focus groups to explore the barriers to successfully implement and use CGM in primary care settings and determine potential solutions. Focus group participants included patients, primary care clinicians, durable medical equipment suppliers, pharmacy suppliers and health insurance plan representatives. This work builds on numerous resources and tools already developed by the AAFP.
Optimizing Approaches to Continuous Glucose Monitoring
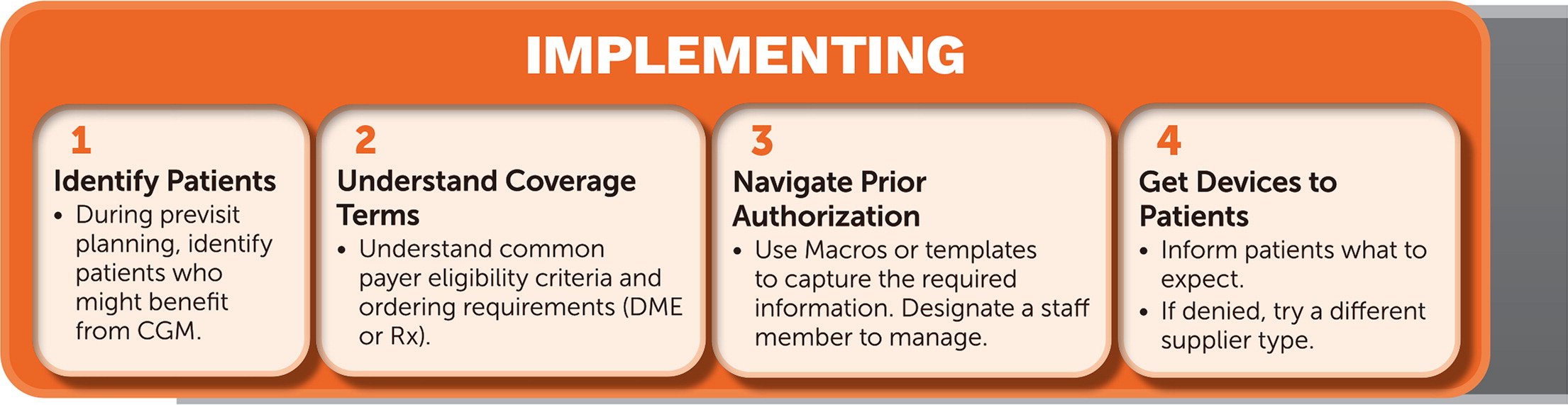
Whether starting out with CGM or looking to tackle existing hurdles, the following four steps can help you overcome the barriers identified in the focus groups. The steps in this supplement should not be considered a comprehensive guide to implementing CGM but rather an overview of key steps.
STEP 1: IDENTIFY PATIENTS WHO MIGHT BENEFIT FROM CONTINUOUS GLUCOSE MONITORING
As a best practice, pre-visit planning helps identify patients for potential use of CGM before they visit your office. However, don’t let that be a limiting factor if you identify an opportunity during a patient visit. The following simple tips can help identify patients who might benefit from CGM:
Run reports of all patients treated with insulin, other glucose-lowering medications or those not meeting glycemic targets (e.g., hemoglobin A1c ≥ 8.0%).
Assign care team member(s) to proactively identify patients who may benefit from CGM.
THINK ABOUT IT: Which care team member(s) are best suited to identify patients who may benefit from CGM? Do you currently have or are there processes you can implement to facilitate this work or technology to identify patients who may benefit from CGM?
STEP 2: UNDERSTAND THE TERMS OF INSURANCE COVERAGE
Understanding insurance coverage can be key to implementing CGM in your practice. Having a care team member who is well-versed with your most common payers in the following can help:
Knowing whether CGM is covered as a medical (i.e., durable medical equipment) or pharmacy benefit (or maybe both)
Knowing whether prior authorization is required for insurers, which is almost always the case unless you use a professional CGM
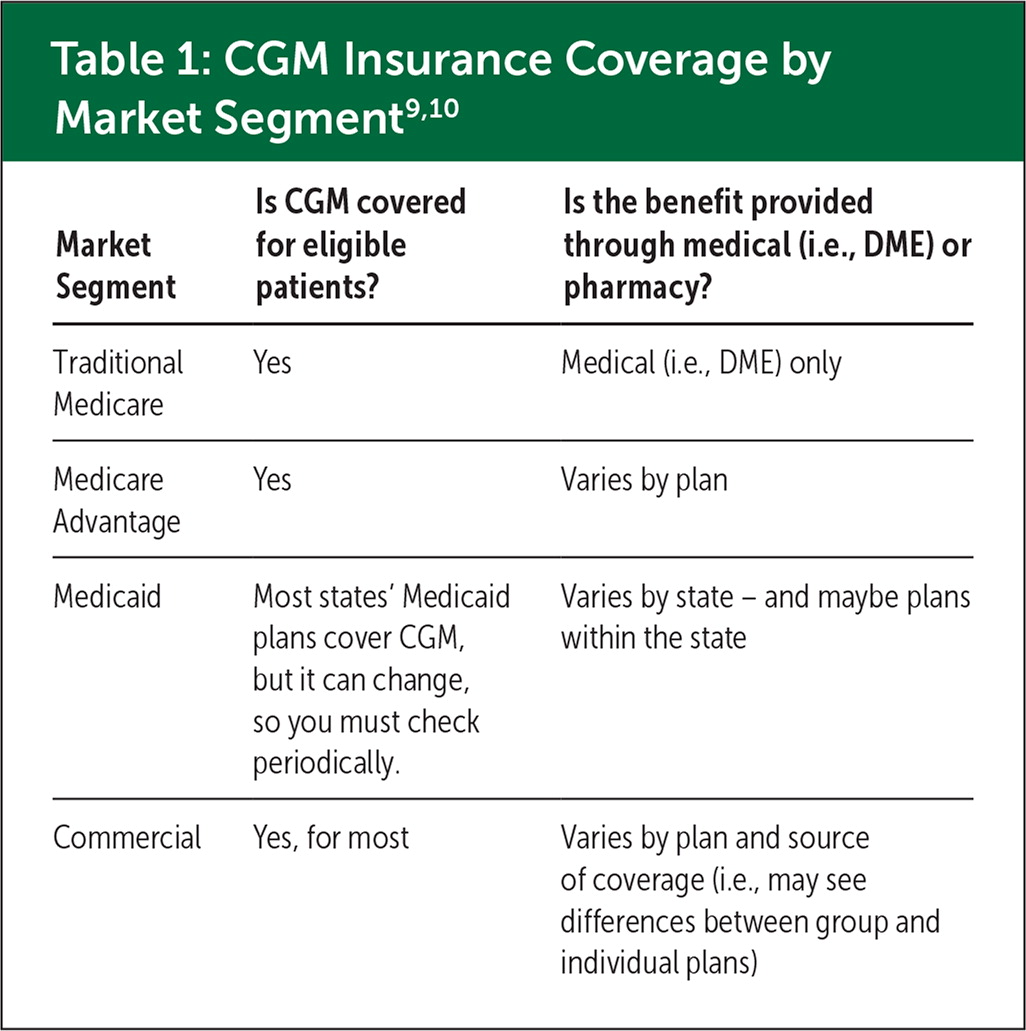
| Market Segment | Is CGM covered for eligible patients? | Is the benefit provided through medical (i.e., DME) or pharmacy? |
|---|---|---|
| Traditional Medicare | Yes | Medical (i.e., DME) only |
| Medicare Advantage | Yes | Varies by plan |
| Medicaid | Most states’ Medicaid plans cover CGM, but it can change, so you must check periodically. | Varies by state – and maybe plans within the state |
| Commercial | Yes, for most | Varies by plan and source of coverage (i.e., may see differences between group and individual plans) |
The type of insurance your patient has will dictate how their CGM benefit works. This includes the plan’s clinical criteria for CGM eligibility (see Step 3) and the recommended pathway for procuring the CGM sensors (see Step 4). While these vary across insurance plans, there are also distinct considerations related to the market “segment” from which your patient’s insurance comes.
Even a single “ABC” branded plan can have multiple pathways for its members to access CGM, depending on whether the coverage is provided through Medicare versus Medicare Advantage plan, Medicaid or commercial plans (either provided by their employer or purchased individually). Manufacturer representatives often know plan-specific coverage criteria and which plans cover CGM through pharmacy and which are covered through DME. Enlist their help.
KEY MESSAGE: Don’t assume that an order being denied means it’s not covered. Instead, send the order to another type of supplier or as a different type of benefit (e.g., if it is denied as a pharmacy benefit, send it to a DME supplier; and if it is denied as a DME benefit, send it to a pharmacy).
THINK ABOUT IT: Are your practice’s insurance experts helping you navigate the coverage complexity associated with CGM?
STEP 3: NAVIGATE PRIOR AUTHORIZATION REQUIREMENTS
Internal workflows, such as the following, can help tremendously:
Use macros, smart phrases, auto text, etc., to ensure your office notes contain the information suppliers and/or payers require. Structure them to capture all the essential elements to maximize the likelihood of successful authorization the first time. Medicare eligibility guidelines are a good starting point for creating templates. Update your electronic health record templates as requirements change.
Be familiar with the patient’s insurance eligibility requirements (e.g., Medicare requires treatment with insulin or a history of problematic hypoglycemia; some payers require a certain number of SMBG checks per day).
Consider using an “e-prescribing” or “DME e-prescribing” platform (e.g., Parachute Health or DMEscripts) to streamline the process of ordering, including prior authorization. Unlike the e-prescribing functionality native to most EHRs, they often have eligibility requirements for specific insurance plans and connect to participating suppliers covered by your patient’s insurance. You are also able to monitor the progress of the order.
Use macros to document and guide CGM data interpretation. Ensure you capture key CGM metrics and therapy changes to justify billing for CGM interpretation.
Create order sets and favorites that include the CGM sensor and separate reader/receiver required by Medicare.
Pre-populate orders to save time (e.g., use continuously, change every 15 days, dispense 90-day supply, four refills).
When appealing denials, quote standards of care and/or scientific literature supporting CGM use in your patient’s specific situation.
THINK ABOUT IT: Have your insurance experts provided a cheat sheet for insurance requirements? Is it frequently updated?
STEP 4: EFFICIENTLY GET CONTINUOUS GLUCOSE MONITORS IN PATIENTS’ HANDS…OR ON THEIR BODIES
It can be challenging to know at the point of care if a plan covers CGM under a pharmacy or DME benefit unless you have previously followed the above steps. Getting the order filled can also be confusing for patients, who may not understand their coverage. DME suppliers expressed that many patients do not respond to outreach and contact efforts, and their orders are never filled. Inform patients they may need to follow up with pharmacies or suppliers.
Choose a dual supplier who can process the order under pharmacy or DME benefits. They can reprocess the order with one if it’s denied under the other.
It can seem effortless and tempting to send the CGM order to your patient’s preferred pharmacy where they get all their medications. If CGM is denied at a local pharmacy, the pharmacy may not know how to redirect the patient. Likewise, patients may wrongly believe that if it’s denied at their preferred pharmacy, then their insurance does not cover the device. Using a dual supplier can potentially solve this problem.
If you’re not using a dual supplier and CGM is denied, submit it to the other type of supplier (pharmacy versus DME).
Utilize suppliers and manufacturer support when available. Some will offer one-on-one patient support in setting up the CGM system, including help with the cloud account to share CGM data with you. Some suppliers and manufacturers have partially completed forms (e.g., names, addresses, etc. already filled out) to save you time.
Provide professional CGM as an option for your patients. It may not require prior authorization and provides helpful information for treatment decisions. The investment can be as little as $60, which can be recouped through fee-for-service billing for interpretation. Unfortunately, this is unavailable for those not on FFS billing, including Federally Qualified Health Centers.
Get samples from CGM manufacturers. You and your team members can try setting up and using the devices to get a feel for the patient’s experience. If you help set up the devices with the patients, you can review their data to guide treatment decisions.
KEY MESSAGE: When you send a CGM order to a DME supplier, tell your patient to expect a call from an unfamiliar number (i.e., “ABC Medical” or “XYZ Supply”) and to call back when they get a vague voicemail (e.g., “I’m calling about a medical device”). Suppliers can’t leave more specific information (e.g., using language like “diabetes” or the doctor’s name). Ideally, tell the patient the name of the company that will be calling.
THINK ABOUT IT: Have you explored professional CGM or obtained samples from your local manufacturer representatives to let patients try CGM?
Sustaining Your Program
ENLIST YOUR TEAM
Enlist the help of your practice team to perform the tasks that make sense in your environment. Dedicate time to developing workflows and training staff. Lean on existing resources from the AAFP and from manufacturers or suppliers to understand the details of implementing CGM and the nuances of coverage.
One physician told us, “Our medical assistants help us through this process, and when someone learns something, they share it with the others.”
Some successful practices noted that having a CGM champion (i.e., clinical pharmacist, diabetes care and education specialist or another team member with knowledge in diabetes care) can be especially helpful.
EMPOWER, ENGAGE AND EDUCATE PATIENTS
CGM can help patients take control of managing their diabetes. One family physician shared that before incorporating CGM into his practice, he would repeatedly tell his patients how different foods might affect their glucose levels. Once they started using CGM and could see their real-time glucose levels change, they’d return to him and say, “Doc, you wouldn’t believe what happens when I eat a bagel!”
For patients, this knowledge can be empowering, engaging and educational – all at the same time. Numerous studies show that CGM alone – without other interventions like medication adjustment – is associated with a decrease in HbA1c.5
Providing care for patients with diabetes is a cornerstone for most family physicians. Using CGM can help you make treatment decisions with your patients easier and improve their health and quality of life. Optimizing practice workflows for CGM makes providing that care less burdensome for you and your staff.

Get Paid for Your Efforts
If you bill FFS, there are CGM-specific service codes you can bill to be compensated for your efforts. These include the following codes11:
95249 – Startup of a personal CGM system
95250 – Startup of a professional CGM sensor, which covers the cost of the CGM sensor and your efforts
95251 – Interpretation of at least 72 hours of CGM data
Visit the AAFP’s CGM webpage for more information, including tips on when to bill CGM with an evaluation and management service.
CGM can enhance value-based care by helping you achieve improved performance on quality metrics. For example, patients can often reach target glycemic levels faster by optimizing medication doses through CGM than by relying on HbA1c levels. Note: The National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set program allows GMI (i.e., a calculated value from the CGM-derived average glucose) instead of HbA1c in its glycemic assessment measures.
