
Fam Pract Manag. 2025;32(4):49-52
The publication of this content is funded by an unrestricted grant from Pfizer Inc. and brought to you by the AAFP. Journal editors were not involved in the development of this content.
Family physicians are the most valued and trusted sources of health information for their patients. As you care for your patient population, it is important to strongly recommend COVID-19 vaccinations, just as you recommend all other vaccines. A recommendation from a health care professional is the strongest predictor of whether a patient will get vaccinated.1
Due to the concurrent circulation of respiratory viruses each year, it is important to discuss risk factors with your patients, as well as prevention and treatment plans that can reduce COVID-19 transmission in households and communities. This clinical guidance tool can help your practice team prepare to talk with patients about the benefits and risks of COVID-19 vaccinations, address their questions and help them make an informed decision. It highlights recommended approaches for encouraging patients to get a COVID-19 vaccine.
COVID-19 Vaccination Recommendations
Many people believe that vaccines are important. However, increased skepticism and concern about vaccination during the COVID-19 pandemic made some people hesitant to get any vaccines. It is important to talk about COVID-19 vaccinations when you have conversations about routine vaccinations with your patients, especially those at higher risk for severe COVID-19 illness. You can reassure your patients that COVID-19 vaccines are safe and effective and emphasize that getting vaccinated protects them, their families and their communities from serious illness, hospitalization or even death.
The American Academy of Family Physicians has approved the following 2024–2025 COVID-19 vaccination recommendations2 :
People 6 months and older should receive a 2024–2025 COVID-19 vaccine.
It is especially important for the following to get a 2024–2025 COVID-19 vaccine:
○ People 65 years and older
○ People at increased risk for severe COVID-19 infection
○ People who have never received a COVID-19 vaccine
Access the comprehensive 2024–2025 COVID-19 vaccination schedule.
Patient-Physician Conversations: Using Motivational Interviewing Strategies
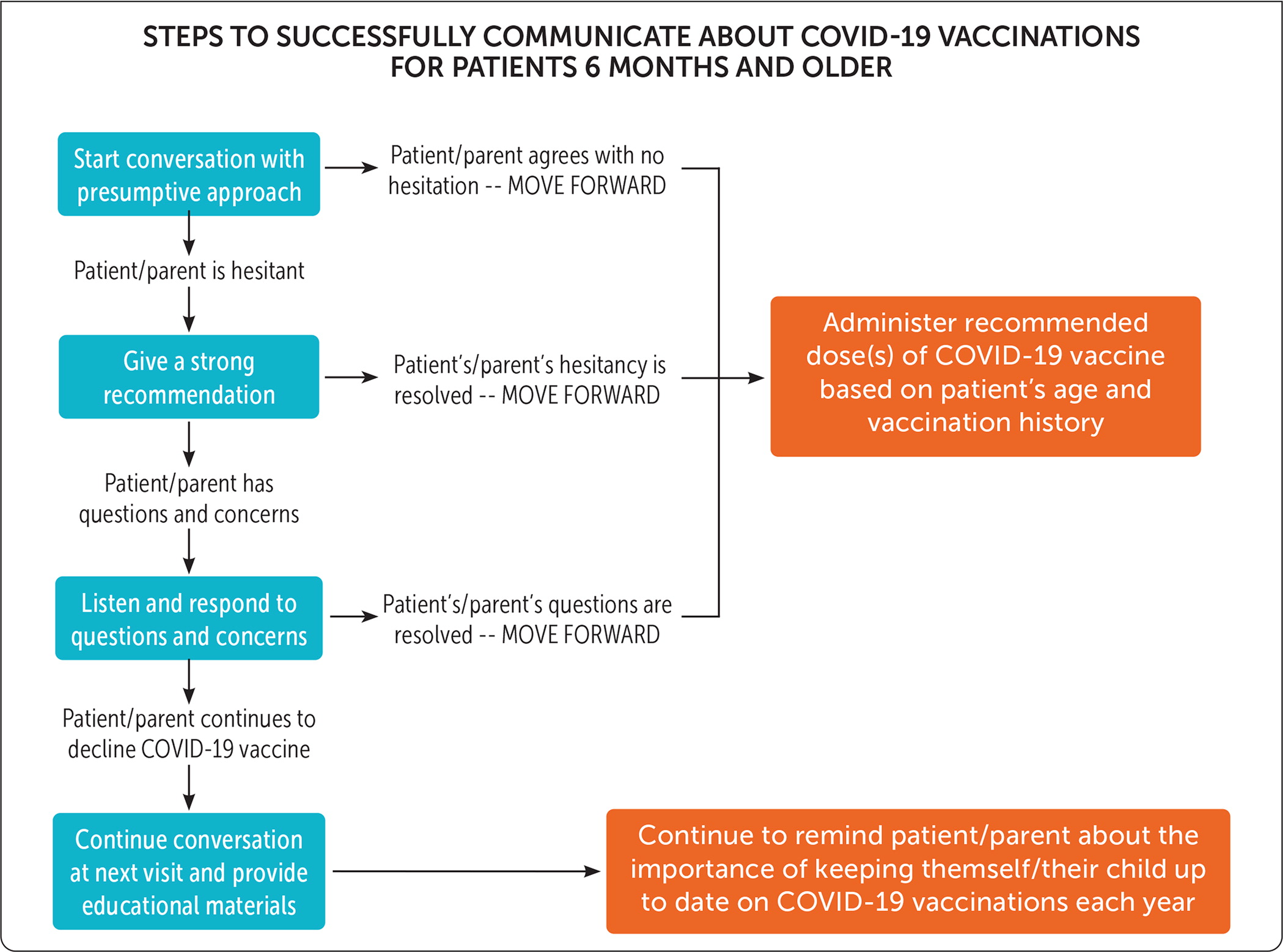
STEP 1. USE A PRESUMPTIVE AND POSITIVE APPROACH FOCUSED ON ILLNESS PREVENTION
When you recommend a COVID-19 vaccine to a patient, assume they will receive it that day. Rather than asking if your patient wants to be vaccinated, explain that they are due to get a COVID-19 vaccine and will be vaccinated during their visit. Highlight why the patient needs a COVID-19 vaccine to protect them, with a special emphasis on illness prevention.
“Hello, Mr. Rogers. I see you are here today for your diabetes check. Since you haven’t had your COVID-19 vaccine yet, we’ll give you that vaccine today to continue your preventive care.”
STEP 2. LISTEN CAREFULLY AND RESPOND WITH AN ATTITUDE OF CURIOSITY, EMPATHY AND COLLABORATION
Patients who are hesitant about getting a COVID-19 vaccine may be more willing to get vaccinated if you take an empathetic, collaborative approach with them. If a patient does not want to discuss getting a COVID-19 vaccine, respect their preference and leave the door open for a future conversation. Based on your patient’s exhibited emotions and expressed values, you may want to briefly explore why they do not want to talk about vaccination. It may also be helpful to provide patient education materials or point them toward reputable websites that offer COVID-19 vaccine information (e.g., familydoctor.org, Centers for Disease Control and Prevention).
“Mr. Rogers, I hear you saying you don’t want to get a COVID-19 vaccine today. Because I care about your overall health and want to help you avoid getting sick, I wonder if you would be open to talking about the COVID-19 vaccine at your next office visit.”
STEP 3. PRACTICE ACTIVE LISTENING AND USE MOTIVATIONAL INTERVIEWING STRATEGIES
At this point, it is important for you to focus on listening to gain understanding rather than trying to change your patient’s mind. It is unlikely that debating your patient will make them more willing to get vaccinated. Instead, show that you are sincerely curious about their feelings and concerns.
“Mr. Rogers, I hear your concerns and understand why you are hesitant to get a COVID-19 vaccine today. As your family physician, I’m here to give you the best medical advice to protect you and prevent any serious illness or medical complications.”
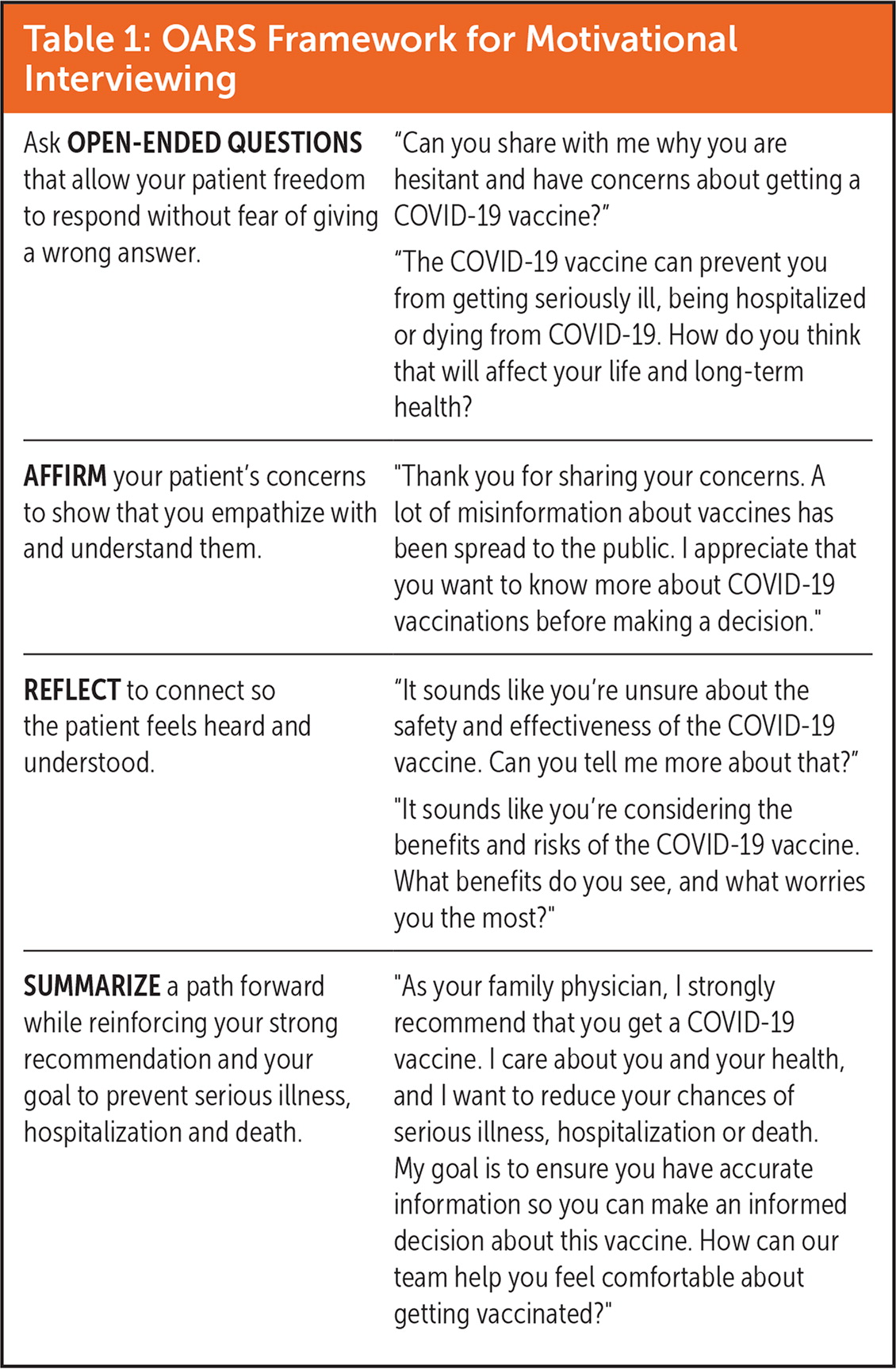
| Ask OPEN-ENDED QUESTIONS that allow your patient freedom to respond without fear of giving a wrong answer. | “Can you share with me why you are hesitant and have concerns about getting a COVID-19 vaccine?” “The COVID-19 vaccine can prevent you from getting seriously ill, being hospitalized or dying from COVID-19. How do you think that will affect your life and long-term health? |
| AFFIRM your patient’s concerns to show that you empathize with and understand them. | “Thank you for sharing your concerns. A lot of misinformation about vaccines has been spread to the public. I appreciate that you want to know more about COVID-19 vaccinations before making a decision.” |
| REFLECT to connect so the patient feels heard and understood. | “It sounds like you’re unsure about the safety and effectiveness of the COVID-19 vaccine. Can you tell me more about that?” “It sounds like you’re considering the benefits and risks of the COVID-19 vaccine. What benefits do you see, and what worries you the most?” |
| SUMMARIZE a path forward while reinforcing your strong recommendation and your goal to prevent serious illness, hospitalization and death. | “As your family physician, I strongly recommend that you get a COVID-19 vaccine. I care about you and your health, and I want to reduce your chances of serious illness, hospitalization or death. My goal is to ensure you have accurate information so you can make an informed decision about this vaccine. How can our team help you feel comfortable about getting vaccinated?” |
STEP 4. CONTINUE THE CONVERSATION AFTER VACCINE DEFERRAL
If a patient continues to decline a COVID-19 vaccine after you give a strong recommendation and engage in brief motivational interviewing, document the conversation and the patient’s deferral in their medical record. Indicate in future visit notes that the patient is due for a COVID-19 vaccine. Also, consider adding vaccine deferral to the list of active health issues. This will serve as a cue to talk about COVID-19 vaccinations with them at a subsequent visit.
Additional Resources
FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION
Pink Book Education Series: COVID-19 Vaccines — One-hour web-on-demand video that provides an overview of vaccination principles, general best practices, immunization strategies and specific information about COVID-19 vaccines.
COVID-19 Vaccine Administration and Coverage, Children and Adults, by Jurisdiction, United States — COVID-19 vaccination coverage estimates for children and adults based on aggregated Immunization Information Systems data from U.S. jurisdictions.
FROM THE AAFP
Shared Conversation Tool for COVID-19 Vaccinations — Clinical guidance tool to help family physicians and primary care teams initiate discussions with patients, parents and caregivers about the critical importance of COVID-19 vaccinations to prevent or minimize the severity of COVID-19 infections. Offers evidence-based strategies that can be incorporated into the practice workflow.
Improving Adult Immunization Rates Within Racial and Ethnic Minority Communities, Part 1: Quality Improvement, Recommended Vaccines, and Reducing Vaccine Disparities — Educational supplement that outlines how using a quality improvement process and other evidence-based strategies (e.g., Plan-Do-Study-Act cycles) can improve immunization rates among adult patients and boost the uptake of vaccines, including COVID-19 vaccines.
Improving Adult Immunization Rates Within Racial and Ethnic Minority Communities, Part 2: Communication Strategies and Overcoming Vaccine Myths, Misinformation, and Barriers — Educational supplement that focuses on practical strategies to communicate about immunizations and overcome myths, misinformation and barriers to improving vaccine confidence and vaccination rates within racial and ethnic minority communities.
Impact on Health Systems from COVID-19 and the Role of Social Determinants of Health — Educational supplement that highlights the impact of COVID-19 on health care systems and the social determinants of health that influence a patient’s health outcomes. Includes a call to action for family physicians to use their platform to ensure equitable access to COVID-19 vaccines, testing and treatments.
Key Takeaways for Family Physicians
COVID-19 can cause severe illness, hospitalization and death.2
A COVID-19 vaccine is recommended for people 6 months and older.2
It is important for previously vaccinated patients to get a 2024–2025 COVID-19 vaccine because vaccine protection wanes over time.
You can help patients understand your COVID-19 vaccination recommendation by educating them about the potential health impacts of COVID-19 illness and the benefits of getting vaccinated.
By showing empathy and understanding, you can help patients move from vaccine hesitancy to vaccine acceptance.
If you take a patient-centered approach that builds trust, a patient who defers a vaccine at one visit may be willing to get vaccinated at a future visit.
