
Fam Pract Manag. 2025;32(5):4-6
The publication of this content is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

Artificial intelligence (AI), also referred to as augmented intelligence, is rapidly expanding into nearly every aspect of our daily lives. This is also true for family physicians. AI is already reshaping clinical care and streamlining administrative tasks, the latter of which consumes an inordinate amount of time and energy in many practices. The American Academy of Family Physicians (AAFP) is working to ensure that family physicians are the leading voices in discussions and decisions regarding AI-enabled technologies being adopted in primary care settings across the country.
Primary care is uniquely positioned for AI transformation, yet it receives relatively little attention from the technology industry. Family physicians’ significant administrative burden and management of complex, guideline-driven medical conditions, along with high volumes of patient data, make primary care a prime candidate for the appropriate use of AI. Recognizing this opportunity, in the fall of 2024, the AAFP kicked off a collaboration with Rock Health, a leader in digital health technology, to ensure that AI is implemented in ways that strengthen and sustain primary care. The initiative is designed to ensure primary care is at the forefront of AI use in medical settings, and technology companies are building solutions informed by the needs of physicians delivering primary care. A primary care physician leadership committee was formed at the beginning of the initiative to shape and advance the project’s deliverables, including conducting a survey and developing CME, as described in this Beyond the Beltway article.
AI PRIMARY CARE PHYSICIAN LEADERSHIP COMMITTEE
Jennifer M. Peña (co-chair), MD, FACP, AAHIVS, Wisp, former White House Medical Unit
Brent K. Sugimoto (co-chair), MD, MPH, FAAFP, Decoded Health, California Academy of Family Physicians
Ricky Y. Choi, MD, MPH, Samsung Electronics America, Stanford University
Jackie Gerhart, MD, Epic, University of Wisconsin School of Medicine and Public Health
Winston Liaw, MD, MPH, Tilman J. Fertitta Family College of Medicine
Steven Lin, MD, Stanford University
Shweta Maniar, Google, RxSight, Orthofix, Allen Institute, USDM Cloud Compliance Advisory Board
Kameron Matthews, MD, JD, FAAFP, Cityblock Health
David Rushlow, MD, Mayo Clinic
Nipa Shah, MD, University of Florida
William B. Weeks, MD, PhD, MBA, AI for Health, AI for Good Lab, Microsoft
STARFIELD AI SUMMIT
The Starfield Summit on Advancing AI and Digital Health in Primary Care was held May 13–14, 2025, in Kansas City, Missouri. At the summit, the AAFP and Rock Health convened physicians and other clinicians with technology leaders, developers and other key stakeholders to deliberate on the future of AI and digital health in primary care. The deep discussions at the event underscored the transformative potential of AI—not as a replacement—but as an essential tool to augment the core values of primary care, which include accessibility, continuity, coordination and comprehensiveness.1
The overarching sentiment of attendees at the summit was clear—the integration of AI into primary care should deepen the bonds between physicians, care teams and patients. AI-enabled technologies—such as ambient documentation and load-balancing agents (i.e., automating routine tasks, enhancing clinical decision-making and reducing administrative burdens)—were recognized for their ability to restore precious time with patients, allowing for meaningful interactions and recentering visits on building trusting relationships with patients. Achieving this vision means recognizing AI as a trusted member of the care team by facilitating tasks, such as triage and personalized education. Freeing up time on such tasks allows physicians and care teams to focus on building stronger relationships with patients and accomplishing more complex tasks.
Attendees at the summit recognized the promise of AI in primary care, but also noted that AI may have potentially harmful impacts, so primary care leaders must remain vigilant when assessing and implementing AI tools and systems. It was also emphasized that the design of all digital health tools, including those utilizing AI, should be driven by physician and other clinician input to ensure they meet the needs of physicians, care teams and patients. To be trusted and drive efficiencies, summit attendees contemplated whether AI reliability must be nearly perfect or if AI should be assessed against current human and system error rates. There was general agreement that early AI adoption may initially result in inefficiencies before the full potential of AI tools and systems can be achieved. A consensus formed around making AI fluency a core component of primary care training and building market awareness and understanding tools were deemed essential for successful AI adoption. The ability to explain the tools was identified as crucial for building trust in AI capabilities and systems for physicians, care teams and patients.
The summit also addressed open questions, risks and challenges that AI adoption might bring to primary care. Maintaining clinical autonomy and focusing on patient care were identified as key concerns, with primary care AI champions needed to safeguard against compromising its values. Overreliance on AI could pose liability risks, and the financial incentives influencing the increased use of AI remain largely unknown. Legal, ethical and policy implications were also discussed. The lack of federal oversight could result in greater innovation but lead to a fragmented landscape with undefined liability and the potential for unsafe systems that pose significant concerns.
THE VISION FOR AI TO STRENGTHEN PRIMARY CARE
A comprehensive report, “The Starfield Signal: A Shared Vision and Roadmap for AI in Primary Care," co-authored by the AAFP and Rock Health, details the findings from the summit, survey data and research on AI in primary care. The report presents a shared vision for how AI can sustain and strengthen primary care, along with a roadmap for action, both of which are summarized here.
There was broad agreement that AI will change how health care is delivered. The unknown is whether the changes AI brings will strengthen or weaken the core attributes of primary care. The overwhelming consensus among summit attendees was that it can strengthen primary care, and it must. The views from the broad, cross-industry group of summit attendees serve as the basis for this shared vision.
The vision to strengthen primary care was described as AI-enabled, team-based and patient-centered care, allowing us to shift the narrative from “top of license” to “top of purpose” for physicians and other members of the care team. This means that just because AI can do something, it doesn’t mean that it should. Physicians and other human members of the care team must continue to represent the true human value of primary care.
THE VISION
AI can strengthen primary care to improve human health—but only if:
Physicians are involved throughout the innovation lifecycle
Training and support are provided
Key system barriers are proactively addressed
Summit attendees were emphatic that achieving this vision would require all key stakeholders—physicians, other clinicians, administrative leaders, technologists, payers and policymakers—to act boldly and collaboratively.
Another outcome gathered from summit attendees was the development of a roadmap for making the vision a reality. The roadmap outlines a significant number of “must-do” actions categorized into three key areas as shown in Table 1: convening relevant stakeholders, advocating to address system barriers and resourcing physicians, care teams and patients.
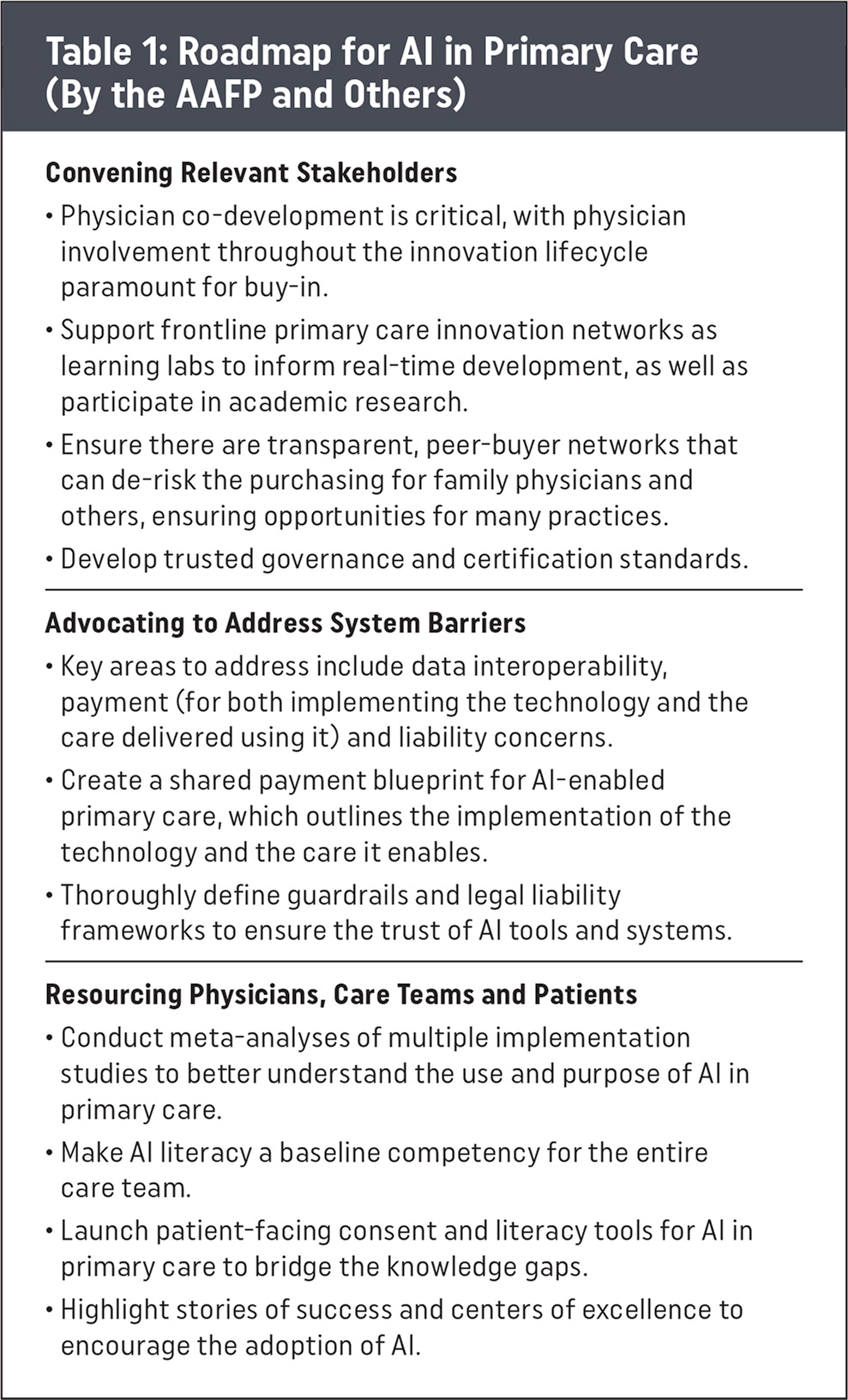
Roadmap for AI in Primary Care (by the AAFP and Others)
Convening Relevant Stakeholders
|
Advocating to Address System Barriers
|
Resourcing Physicians, Care Teams and Patients
|
Our next steps include collaborating with the American Board of Family Medicine to leverage their AI annual survey and incorporating AI-related questions into the AAFP’s Practice Profile Survey and other existing surveys. These opportunities will enable us to continue to monitor AI adoption across family medicine.
While there are still many uncertainties surrounding AI and its use in medicine, the Starfield summit concluded with a clear message—AI holds the potential to revolutionize primary care, but its success depends on careful planning, robust governance and a commitment to the core values of primary care. By following the outlined vision and roadmap, stakeholders can ensure that AI strengthens and sustains primary care, making it more human, equitable and essential than ever.
SURVEY OF FAMILY PHYSICIANS ABOUT AI AND DIGITAL HEALTH
In addition to the summit, the AAFP conducted a national survey with more than 1,200 respondents, mostly family physicians, along with other primary care clinicians, in the fall of 2024. Survey results were published in the AAFP’s Quick Tips blog and the Rock Health blog, AI Is in the Doctor’s Bag—And Primary Care Is Ready to Use It.
Key findings from the survey indicate high usage of digital health tools, with 92% of respondents using EHRs at least weekly, 83% using clinical decision support tools at least weekly and 74% using patient engagement tools at least weekly.2
Many clinicians are already using AI-adjacent tools and are open to adopting new technologies, both professionally and personally. Survey respondents expressed a strong desire for education and support in evaluating and implementing AI tools responsibly.
CME OFFERINGS
The survey highlighted a clear need for AI education tailored to family physicians. In response, we developed CME and a central hub for information that includes:
Our introductory AI in Family Medicine: Transforming Your Practice CME series consisting of three parts (30 minutes each) covering AI fundamentals and evaluation frameworks.
Our new Revealing AI Use Cases in Family Medicine CME featuring real-world examples of AI use.
Our AI in Family Medicine landing page centralizes CME offerings, along with other resources, such as the Society of Teachers of Family Medicine AI curriculum. This page will continue to grow as new materials are published, including the comprehensive Starfield Signal report.
