Vibe Check #1: Is Family Medicine Right For Me?
Discover the diverse paths, passions, and impact of real family physicians — and see how family medicine could fit into your future
Part of the Vibe Check: Is Family Medicine Right for Me? webinar series, presented by the AAFP in partnership with the Association of American Medical Colleges (AAMC), this session features inspiring family physicians who share their career journeys, the versatility of family medicine, and insights into choosing the right medical specialty.
What You'll Learn:
- How family medicine offers diverse career paths, including geriatrics, preventive medicine, and public health
- The role of family physicians in navigating complex healthcare systems
- Strategies for physician well-being and preventing burnout
- The importance of advocacy and leadership in shaping healthcare
Who Should Watch?
- Medical students exploring specialty options
- Residents considering fellowships or subspecialties
- Anyone passionate about holistic, patient-centered care
Watch the webinar recording above or read the full transcript below to get inspired by the real-life stories of family physicians shaping the future of healthcare!
Table of Contents
- Welcome and Introductions
- Panelist #1 – Dr. Alex McDonald: Leadership and Breadth
- Panelist #2 – Dr. Ryan Walker: Community Health and Identity
- Panelist #3 – Dr. Kelly Thibert: Advocacy and LGBTQ+ Care
- Panelist #4 – Dr. Ian Coker: Rural Hospitalist and Critical Care
- Panelist #5 – Dr. Emily Briggs: Private Practice and Full-Scope Care
- Dr. Bright Zhou: Panel Reflections and Context
- Dr. Briggs on Daily Life and Choosing FM
- Dr. Coker on FM Flexibility and Clinical Fit
- Dr. Thibert on Combining Science and Advocacy
- Dr. McDonald on Sports Medicine and Civic Leadership
- Dr. Walker on Integrative Care and Organizing Black FM Physicians
- Panel Q&A: What They Wish They Knew Before Applying to FM
- Final Takeaways and Farewell
The Panelists

Bright Zhou, MD (Host)

Emily Briggs, MD, MPH, FAAFP

Ian Coker, DO

Alex McDonald, MD

Kelly Thibert, DO, MPH

Ryan Walker, MD, MPH
Don't Miss Vibe Check #2
Find out how another panel of inspiring family physicians started their careers in the second installment of our webinar series.

Dr. Bright Zhou (host) All right, good evening, everyone. I'm so excited to see everyone here. And I'm very excited to welcome us all to our first Vibe Check session about family medicine. My name is Bright Zhou. I use they/them. I just graduated from residency, and I'm so excited that you're joining what is going to be an incredible panel of family physicians ahead of us tonight. We have the pleasure of sharing an hour with real family physicians who are super awesome. Participating in very innovative patient care that highlights the full spectrum of what our specialty does. Thank you to everyone who submitted their questions ahead of time, and we're gonna use those to help guide the discussion. But if we don't get to your questions, feel free to put them into the Q&A. And also, if you think of anything new, definitely let us know, and if we have time to address it today, we'll try our best to get back to you.
Dr. Bright Zhou (host) Our staff from both the AAFP and the AAMC will be monitoring the Q&A throughout our discussion to address all the questions and make sure that we're all heard. But really, we're just so excited to hear from our expert family physicians who are on our panel today. And so, without any further ado, I'd love to start the introductions. A big thank you to all our family physicians who are sharing their time with all of us this evening and also taking time from their patients and their communities to share why our specialty is the best. So, without further ado, let's start with Dr. McDonald.
Dr. Alex McDonald Hey, everyone. I'm really excited to be here. I'm Alex McDonald. I practice family medicine and sports medicine at Kaiser Permanente in Fontana, California. I am one of the core faculty for our residency program here. I also am one of our sports medicine clerkship directors and longitudinal integrated curriculum preceptors for the Kaiser Permanente School of Medicine. So, I teach medical students and residents. I also teach our sports medicine fellows.
Dr. Alex McDonald I do lots of things – I get bored easily. So, I try and do a huge variety of things throughout my day, which is what I love about family medicine. There are so many different aspects which keep me kind of engaged. I practice inpatient medicine; I practice outpatient medicine. I could go on and on and on and on. But that's a little bit about me. I also have a couple of what I like to refer to as my "extracurricular hats." And so, I serve as a trustee for the California Medical Association. I'm also president of the California Academy of Family Physicians here in California, and I'm also a local school board member. I got elected to my school board about a year ago. So, family medicine can do so many things to impact so many lives, both in the clinic, in the hospital, but then beyond that in our communities and even at the state level. So, that's a little bit about me and what I do. And I'll blather a lot more later during my discussion about how I got to where I am.
Dr. Bright Zhou (host) Thank you so much, Dr. McDonald. Next, let's hear from Dr. Walker.
Dr. Ryan Walker Hi, I'm Dr. Walker. I use she/her pronouns. I am a family medicine physician as well as board certified in obesity medicine. I also completed a fellowship in integrative medicine. I practice at a community health center, and I do full spectrum outpatient care. I focus on caring for people who are unhoused and who have substance use disorders, both in the clinic, but also outside, particularly in a shelter, as well as in a respite unit that is run by our clinic as well. I also serve as the family medicine clerkship site director at our clinic, and I am a clinical associate professor for one of the courses called Perspectives in Medicine, where I focus on population health, and that's both for Tufts University School of Medicine. And lastly, I am the co-founder and executive director of the Association of Black Family Medicine Physicians. And I think in this conversation it's important to also acknowledge other identities: being black and also being a first-generation college graduate from the South and from a single-parent family. I like to say I was raised by a village in which I was raised by three generations of women, including my grandmother and my great-grandmother, who I call Granny, because I bring them to this conversation as well as everything that I do. And so, I'm so excited to be here, and thank you for having me.
Dr. Bright Zhou (host) Thank you so much, Dr. Walker. We've heard from two family physicians and heard two completely different paths, and I'm so excited to really dive into this for all our panelists. Next, I'd love to hear from Dr. Thibert.
Dr. Kelly Thibert Thank you so much. I'm Dr. Thibert. My pronouns are she/ her. I'm coming to you from Las Vegas, Nevada. That's not where I'm from – I moved here a year ago. My path has been so wild and wonky, and it's brought me to the best specialty in medicine. I know I'm a little biased. But I was born and raised in South Florida. I did my training in osteopathic medical school and public health in South Florida. And then took my show on the road after medical school. Took a year off between med school and residency to serve as the national president of the American Medical Student Association. So, I'm really involved in advocacy and activism, and that's been a great passion of mine. And after family medicine residency in Columbus, Ohio, I headed back to Florida (and I'll get into this a little bit more later) but currently I'm in Las Vegas, Nevada. I practice at the VA Medical Center. I do outpatient family medicine for female identified veterans. But I've also started the first LGBTQ primary care clinic in the VA in the nation. So, I'm proud to do that and provide full spectrum family medicine or primary care for our LGBTQ plus veterans, including hormone replacement therapy.
Dr. Kelly Thibert I'm also an abortion provider and consider myself a strong activist and advocate in many realms, including through the AAFP and my state academy, the Nevada Academy of Family Physicians. I'm so excited to be here with you all this evening. I am so excited to tell you about family medicine and all the wonderful things you can do. Thank you so much for being here.
Dr. Bright Zhou (host) Wow, okay, I hope we all are feeling the energy rise as we continue to hear from these amazing physicians. Next, let's hear from Dr. Coker.
Dr. Ian Coker Hi, thanks for coming. I'm Ian Coker. I get to follow those three, so I’m not at all intimidated. I am a DO as well. I am a hospitalist at Aspirus Divine Savior Hospital in Portage, Wisconsin, which is about 45 minutes to an hour north of Madison. I provide inpatient care, including ICU care. I am a hospitalist, so I work seven days in a row. And then I have seven days off, which are wonderful. The seven days in a row sure gets tiring by the end.
Dr. Ian Coker I went to the Arizona College of Osteopathic Medicine at Midwestern University, which is in the Phoenix area, for medical school. And then I trained at St. Elizabeth Health Care Family Medicine Residency, which is an Edgewood, Kentucky, or the greater Cincinnati area, which is probably where more people will be familiar with. Graduated medical school in 2020, which meant starting residency during the COVID-19 pandemic. We can touch more about that later about how you end up in med school and then as a hospitalist – they are related. I am a hospitalist at a 25-bed hospital. I do have an APP with me, but I'm the only attending in-house during the day. I do have my own ICU where I do have tele-CU support, but I am responsible for my own procedures. So, I do intubation, central lines, arterial lines, some thoracentesis and paracenteses as well. I do manage the vents with the assistance of RT and intel ICU as well, so my day-to-day can be very different, depending on the day, But outside of work, I like to ride my bike. My wife's also an FM doc. She does OB, which is something I won't touch. And we have a two-year-old and another kiddo on the way and two dogs. So, we keep busy outside of that. Looking forward to talking to you guys more.
Dr. Bright Zhou (host) Okay, breadth. Okay, we love to hear this breadth from our panel. And our last introduction that we're going to hear from is the amazing Dr. Briggs.
Dr. Emily Briggs Well, thank you. I'm so excited to be part of this panel. Such wonderful family docs and such a great breadth. I'm Emily Briggs. I am a full-scope family doc in Central Texas. I'm private practice, owning my own practice. I started my practice 15 years ago, hung my shingle and just went from there. I provide inpatient/outpatient care, obstetric care, including operative obstetrics, lots of procedures in the office as well as in the hospital. A lot of maternity care, reproductive health, and through my journey, did a lot with organized medicine, as some of the other panelists mentioned. That's where I network, and I've really grown as a physician.
Dr. Emily Briggs In central Texas, I have served and am currently serving as the board chair of the Texas Academy of Family Physicians and have been involved quite heavily with the Texas Medical Association, which of course is all the specialties in medicine. At the national level, I've served as a board member for the American Academy of Family Physicians when I was a brand new, new physician. And I now represent the AAFP to the American Medical Association, along with 24 of my very closest friends. So organized medicine has been a wonderful way to continue to advocate for our specialty and our patients. At the state level, I've had the opportunity to serve as the Chair of the Perinatal Advisory Council, where we developed the designation levels for maternity care and neonatal care for the entire state of Texas. And so, through that pathway, not only do I have my fellowship in the American Academy of Family Physicians, but I was recently honored by ACOG in getting an honorary fellowship. I'm not aware of any other family physician that's ever had that before. So, that's my story so far, and I'm excited to be here. Thank you.
Dr. Bright Zhou (host) Thank you again to all our panelists for their brief introductions. We're going to hear a little bit more about their journeys to family medicine shortly. Just a few things I wanted to say to introduce our session today. As all our panelists are aware, choosing medical specialties is one of the hardest things to do as a medical student. I was there probably most recently of all the panelists, and I wish I could have been here to hear about all the different things that family physicians really can do. And so, that's really the intention of today's panel, as well as to help students envision a career that allows themselves to find satisfaction, wellness and true patient care and patient reach in their practice.
Dr. Bright Zhou (host) The American Association of Medical Colleges helped create the Careers in Medicine program, which is a career planning program, and they're partnering with us today to help medical students and those who advise them to choose among all the incredible specialties that exist. So, our first slide here introduces the Careers in Medicine, or CIM, which is basically a toolkit for students to help you guide yourself, thinking about what things are important to you, what are your issues that are important to your future career in terms of how you might decide on a specialty, and also what sorts of practices you might want to be in. It's designed to transform the vocational theory into more of an actionable way to allow medical students to make significant career decisions, such as what specialties they choose and which residency programs to pursue.
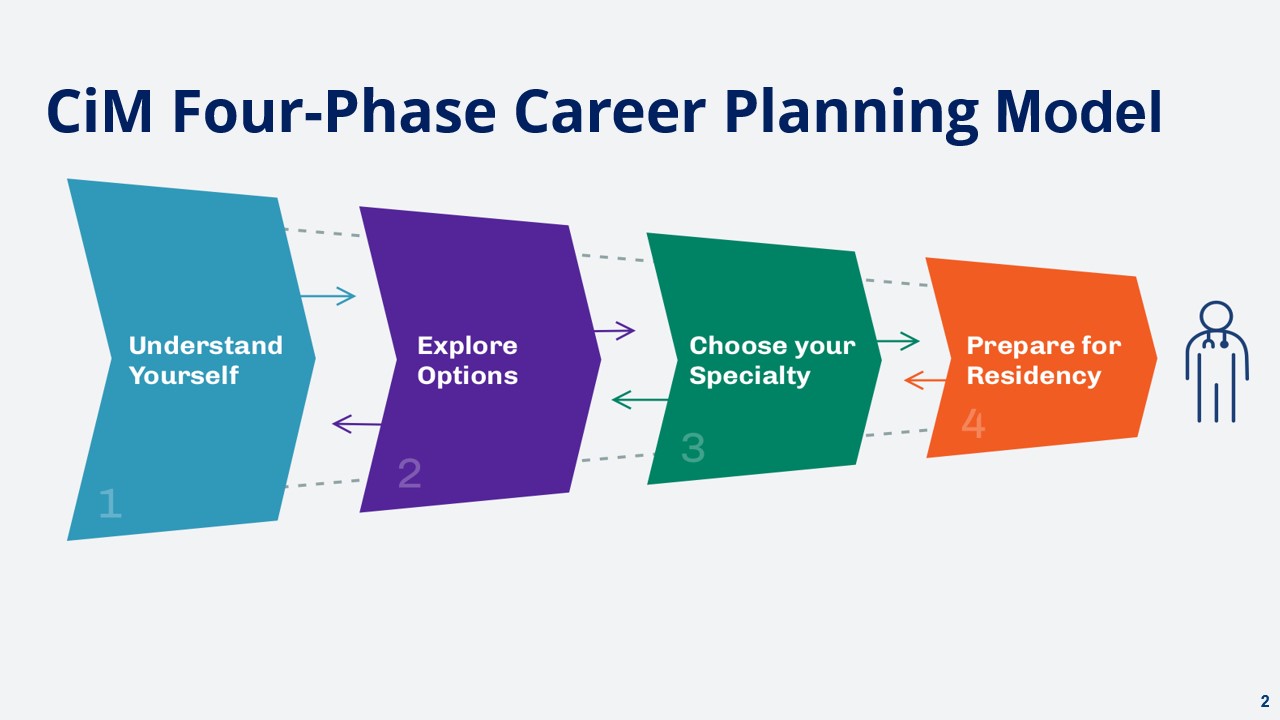
Dr. Bright Zhou (host) And I should mention that CIM is an AAMC member benefit, and it is free to most of our U.S. MD, U.S. DO, and Canadian MD students and advisors. And this four-phase career planning model is the foundation of our CIM program. Phase two, the explore options, includes all the specialty profiles for over 160 specialties and subspecialties. But today, we're going to focus on the family medicine specialty profile. So, I encourage you all to check this out afterwards if you've been inspired by our panelists. And you can see the Overview tab here that's being displayed, which shows information that's most interesting to students as they start to explore their specialty and practice options.

Dr. Bright Zhou (host) All right, now with that introduction to the goals of our session today, I think the part we're all here for is to hear about how these incredible family physicians got their start. How they ended up choosing family medicine, and what advice they might have for all of us here in the room, both students and residents, as we start to decide on what our career practice and paths might look like. So, let's start first with Dr. Briggs.
Dr. Emily Briggs Thank you. I guess I'll start with what my typical day looks like. My typical day, because I'm inpatient and outpatient, I will start my day taking my daughter to school. And then I go to the hospital and round on any patients that I might have there. Maybe I had a delivery in the middle of the night. Maybe just having some inpatient patients to see for chest pain or, you know, various things. Then I go to my office, have my clinic day, and I have lunch with my husband, who is my office manager. We're in a small practice; it's just me and one other family doc. And then by the end of the day, if I've admitted anybody else throughout the day, I go round on them and then go back home and spend time with my wonderful family.
Dr. Emily Briggs Sometimes at 2 a.m. I go back for a delivery. There are two hospitals in the community, and so, I do deliver at both. Not so happily, but you go where you got to go because that's where your patients are. And I absolutely love that I get to have such a dynamic day each and every day.
Dr. Emily Briggs I do have students and residents that come rounding with me. I have high school students that come and visit with me for the first hour of my day often, just to give them a feel for what family medicine is like. And when I have residents and medical students coming with me, they're the ones that are actually delivering the babies. I make sure that they put hands-on on everything we do because that's what's so important. At the end of this, I'll be talking with you a little bit about just how important it is to say yes to everything. So, that's my typical day. The best part of my day, of course, is spending my time with family. Today, I had a student ask me if my patients become my family. And I would say, absolutely. Just as much as I become a member of their family, they become a number of mine, especially in a smaller community.
Dr. Emily Briggs How did I choose family medicine? Well, when I was in third year, I started off my third-year clerkships going to a pediatric clerkship, and I absolutely loved taking care of the kiddos, figuring out the medicine for those tiny humans, but I really did not care for the parents. Then I did a night float routine. And I absolutely loved the medicine component and staying up at night and getting things done and being the only people in the hospital. That was awesome. And then I did my inpatient rotation. And I loved the medicine component, the complexity of all of that. And then, I did surgery. And oh my gosh, working with my hands, that was the best. I wanted that instant gratification. It wasn't until the very end of my clerkships that I had my family medicine rotation. And I realized, “Wait a minute, I can do all of this stuff. I can choose what I'm going to do. I can do a little bit or a lot. I can choose what type of patients to see as far as what disease conditions. I can do obstetric care as well as inpatient, outpatient, pediatrics, adults, everything.” That's my specialty. That's why I chose family medicine.
Dr. Emily Briggs Now, during that time, I became pregnant with my first daughter. And in the meantime, I figured, you know what? I shouldn't just have a medical degree. I might as well get a master's in public health. So, I took a year off between my third and my fourth year. And I pivoted. And I got my master's in public health at that time. So, when I finished, I finished my entire thing and got my MD-MPH at the end, which was a wonderful pivot. And, I had a girl, and that was wonderful, too. So, that was a very unexpected moment.
Dr. Emily Briggs One thing that I would suggest when you are choosing what residencies, if you decide to go into family medicine, and as you know all of us think you should, the thing that I looked for the most was an unopposed residency. When I was going through and factoring in all the things that I knew I wanted to do. I knew I wanted to go back to a small town, having come from a small town. I knew I wanted to do full scope. I knew I wanted to get my hands on everything. And in residency, I wanted to have a breadth of experience that would allow me to have the decision of what direction to take my practice and my patient population. So, when I chose a residency, I had lots of options: academic, private, community. I decided to go with an unopposed residency so that I could be one of the very few residents there and be the one that they would ask to do things.
Dr. Emily Briggs The other thing that I wanted to touch on was my organized medicine experience. I mentioned at the beginning when we introduced ourselves that I went through and got involved with all the academies, really, but that's because as a medical student, I went to my first TAFP meeting, and I got the bug. I got the fire for family medicine. And this is going to sound dorky: I got the fire for parliamentary procedure. I absolutely loved resolutions, advocacy, bringing all these voices together that I could never even consider what somebody else's perspective might be. And I get to hear these perspectives. And it helped to craft the physician that I am today. Now, granted, I've been in private practice for 15 years now, and I don't see that changing. But I've also had the opportunity to travel through the Texas Academy for both family medicine as well as the Texas Medical Association, and then also get perspectives from all the other states and specialty societies through the AAFP and the AMA. It has been a wonderful experience. So, I encourage you that if you have the opportunity to be involved in organized medicine, definitely do that and you can do it because if I can do it – have a wonderfully healthy, happy family and a private practice that is also wonderfully happy and healthy – then that means any of you can do it. That's my story, thanks.
Dr. Bright Zhou (host) Thank you so much, Dr. Briggs. I'm just absolutely in awe, first, about the scope of your practice. One piece that really resonates with me and that I think may resonate with our students is how eager you are to learn. That's something I would really love to highlight for those of you out there who fall in love with everything in your specialty. I think it is something that all our panelists can relate to. That eagerness to care for both the postpartum pair, right? Not just for the peds, not just for the post-partum parents, but for both pairs. And I think for those of us who are third years or fourth years, that's one of those moments to consider family medicine. And then, of course, that desire to apply it into advocacy and policy – I just love that. That's something that I would love to drive home for our audience. Thank you so much for sharing.
Dr. Bright Zhou (host) Next, I'd love to introduce Dr. Coker.
Dr. Ian Coker Hi. I am a rural hospitalist, and – spoiler now – I had no expectation that this was what I was going to do when I started. Like many of you, I didn't really have one moment when I thought, "Oh, I'm going to be a doctor when I grow up." I liked people; I liked my science classes. I figured healthcare was an option for me, but I wasn't quite sure. So, I went to college at Linfield College, which is a small liberal arts school in Oregon. There, we had to do a freshman writing class called an inquiry seminar. Mine was called Illness Healers in the Writing Life. We read books by Atul Gawande, Perry Klass, Abraham Verghese, and I loved it. We spent hours talking about the patient experience, patient autonomy, what it meant to be a doctor and a patient to a lot of these people. And I think that's what kick-started me on that journey – really falling in love with these stories.
Dr. Ian Coker Once I started medical school, I wanted to keep an open mind as far as what specialty I wanted to do. But I eventually did say yes to being our family medicine interest group’s first-year representative. And I was at an osteopathic school, so it's with the ACOFP. That came with a free trip to the ACOFP conference. I loved the people I met there. I felt like I had found my people. I put my name out there for the National Student Executive Board, and I was elected parliamentarian. And then in the later years, I was elected president. So, I really enjoyed that work where we were promoting family medicine across osteopathic schools. And then in my fourth year, I served as the student trustee of the Foundation Board of Trustees for the AAFP, which was also a blast. And, again, I felt like I was working with people that I really resonated with, and that's what, I think, drove me to family medicine.
Dr. Ian Coker But a big part of the reason we're even having this panel is there's lots of different ways to do family medicine. Between my first and second year of med school, I was out in the Boston area in Chelsea. I did a primary care program where we worked with patients with addiction medicine, did research on access to naloxone, and I really enjoyed those patients' stories. They were all different. They were interesting. They were exciting. And at that point in my career, I thought, "Oh, I'm going to work in a federally qualified health center. I might do an addiction medicine fellowship." And here I am not doing any of that. So, when it came time to take a residency, at that point, I had met my now-wife at medical school. We were doing the couples match, and we both wanted to do FM. She wanted to have the option to do obstetrics. At that point, I had some thoughts that I didn't want to do just one thing. I wanted to maybe have the options to do urgent care, hospital medicine, addiction medicine. I wanted flexibility. And like Dr. Briggs, I knew I wanted an unopposed program, because I knew I learned best when I got my hands on things. I was never someone who's very good at watching and then doing it after watching. I really needed to be doing the work. So, when we were trying to decide what residency program, then if you're kind of in that boat where you're trying to say what to do, look up the grads of the programs. We were, you know, a lot of times they'll put out, programs will put on their website: these are the grads – this is what they're doing now. And that can help show you what that training prepares you to do.
Dr. Ian Coker So we ended up at St. Elizabeth because it had a little bit of everything for us. I mentioned earlier, I started residency right when the pandemic started. We joked that none of us had seen our residency classmates without masks until a couple of months into starting residency. But as part of that, everything was stressed. And we were a 500-bed hospital; we were the only residency program. So, we had a lot more critical care and hospital experience than I think was normally expected. We were the code team, the procedure team, the rapid team – so we were doing a lot of that on patients who were very sick. But I felt like this was the first time I really felt like I found my stride clinically. When I was on rotations, I liked a lot of things, but some things were more natural; some things weren't. And I really feel like I was doing my best work. And in residency clinic, a lot of times I felt I had a hard time connecting with the story of the patient, figuring out what was going on with the patient. It felt murky versus when I was in the hospital, things felt clear. I knew what I was doing. I felt like I was good work for my patients. And I really felt like I was able to get them better in a tangible way.
Dr. Ian Coker So, when it came time to pick a job and a few goals: 1) practice at the top of my scope 2) keep as many skills as I had, and, looking back, there was probably a third goal, which is: I really like it when my patients are my patients. I really hated handing off care, either at the end of the week or when there were rumblings of a closed ICU or the surgical ICU closed, and we would hand off patients there and we wouldn't see them again. And that really bothered me. So, after we looked at a lot of jobs to realize that for me, all those goals would probably be best met at a smaller hospital. So, we ended up here in Portage.
Dr. Ian Coker As a smaller hospital, I usually have a lot more time to spend with my patients. So, my day-to-day is not too different from a bigger hospitalist in that I come in, I round, I have multidisciplinary meetings with the support staff, pharmacy, therapy, skilled nurse, social work, to talk about placement for patients if that's what we need to do. But when that's said and done, sometimes I get lots of admissions; sometimes I don't get any. So, on the days that I have time, I like to spend time with my patience in the afternoons, making sure they understand what's going on with their care and what the goals of their care are and why they're still admitted.
Dr. Ian Coker I do have less services to do things for me here. So, sometimes there's difficulty in transferring patients. We're trying to determine how best to triage, but it can be really satisfying when you triage appropriately. I also have to consider a lot of differentials that I don't always have the backup to help with. I have a general surgeon, an orthopedic surgeon, as far as in-person consults. But other than that, it's telehealth. And some of the specialists are awesome, but it's really as good as the sign-out you can give them. If you didn't ask a question, they can't go back and ask that patient that question later. So, it's an exciting way to practice, but it is a challenging way to practice.
Dr. Ian Coker One of the things I wanted to touch on quickly: I decided I liked hospital medicine in that clinic after doing all this clinic work to prepare for family medicine residency felt really off-kilter. I was like, "Oh gosh, I'm betraying everything I ever stood for." And I ended up talking to Dr. Christina Kelly, who's someone I consider a bit of a mentor. That's the other thing: when you have mentors, use them. And she was like, "It's not where you practice, it's how you practice." And that really resonated with me. I do feel like I get to spend a lot of time with my patients, and I really have the philosophy of, "when you're admitted to the hospital, you're my patient, under my care, until you physically see your PCP." And that's something that I think I get to do here that I may not get to do at a much bigger place. So, that's kind of how I got here. I didn't think I'd be doing this when I started, and I do really like it, but I don't think it's for me forever. I really miss academia, actually – I really miss teaching. So, I think, in the future, I'd like to incorporate more of that in my practice.
Dr. Bright Zhou (host) Thank you so much Dr. Coker. I really appreciated that story. The story part and the people as the core of what brought you in, starting from your very first interest in medical humanities, going into the advice that I also wholeheartedly echo about finding your people. And a nod to Dr. Briggs' point about organized medicine maybe being one of those places where you do find your people and your mentors, and certainly I can totally relate as places where I've found my own, as well. And really highlighting, again, the breadth, the scope of our practice is so large, and I think we've heard from two speakers who are absolutely maximizing the scope of their practice, and it is something that is a draw to family medicine. In addition, being able to choose more selectively and work at whatever scope you choose to work at, I think, is another draw of family medicine. We'll hear that from some of our other speakers as well. Thank you so much, Dr. Coker. And I'd love to hear from Dr. Thibert next.
Dr. Kelly Thibert Thank you so much, Bright, I appreciate it. I also didn't think I'd be a physician. Nobody in my family practiced medicine. And, in fact, my brother was the only person who I knew who was going to college. I didn't know anybody else who had pursued education beyond high school. So, I didn't really have a plan as to what I was going to do. So, I was following my brother's footsteps, hoping he was leading me on the right path.
Dr. Kelly Thibert I happened to take an anatomy and physiology class in high school. Again, because my brother took this class and said it was fun. And we got to the point of the year where we got do dissections, and I just fell in love. Right now, as a vegetarian, I feel bad saying that, but looking back on it, the anatomy and physiology piece, just learning how something functioned that you couldn't see with your eye and learning the science behind that – it was just breathtaking to me. And so, I went up to my teacher one day at lunch, and I said, "How do I dissect for a living?" And he was like, "That's a weird question, Kelly. What do you mean?" I said, "I don't know, I want to do this. I want to learn more about how things work like this in a body and how I can help in those ways." And he said, "Well, I think you want to be maybe a medical examiner." And I was like, "Okay, cool. How do I do that?" And so, he told me I wanted to go to medical school. And I was like, "I also don't know what that means. Tell me, what would going to medical school mean?" And he said, "Well, you're going to want to be a physician." That's what a medical examiner was. So, coming out of high school, my thought process was, I want to dissect. I'm going to be a medical examiner. And that was it. I knew nothing about what this process entailed.
Dr. Kelly Thibert So I happily went along to my undergraduate career at the University of Central Florida. I majored in Molecular Microbiology. After changing my major from chemistry to molecular microbiology (brother did not lead me on the correct path with the chemistry major there). So, I did that and then probably a year into my science training, I started to learn that there were minors you could do. And so, I started to minor in women's studies, which was something I was very privileged to get the opportunity to participate and learn in in high school, so this was a continuation of my knowledge and learning of women's studies, which was wonderful. So, with that minor and then also with my science background my underlying question was, "I really love both of these things, but how do I get them to meld together, and do they even do that?" I had no idea. So as a lost pre-med at this time, or what I declared as pre-med because, again, I didn't know what I was doing, I joined the American Medical Student Association or AMSA. And it was there that I really began to bud as an activist and an advocate and really learn that medicine is activism, and medicine is advocacy, and this, in fact, was going to be the place for me. I just didn't know how much I had to learn still about the whole process.
Dr. Kelly Thibert And so, with that, I was on the road to the entirety of medical school at Nova Southeastern University College of Osteopathic Medicine in South Florida. I went in there and was like, "I have my women's studies background. I have my medicine background. I'm going to be an OB-GYN – that's got to be the way that I'm going, right?" And I thought it was going to be the only fit for me. But again, one year into my training, I decided to pursue another level of education. So, I actually started to pursue my masters of public health concurrently with my doctorate of osteopathic medicine. And it was one of the best decisions I made in medical school because it really helped me to change how I viewed medicine, how to practice medicine, and what it meant to be a part of the medical community and caring for whole communities that we live in and that we work in and that we teach in.
Dr. Kelly Thibert And so, my final year of medical school, my very last rotation, that's when I decided I was going into family medicine. So, I was rotating at a FQHC, a federally qualified healthcare center. And this osteopathic physician that I was with was incredible. He was also a DOMPH, like I was about to be, and he was caring for his community. He was caring for members of my community, the LGBTQ+ community. He was caring for folks who were living with HIV. He was providing care for people who couldn't be seen in other places. He was also participating in public health, in community forums and advocating alongside and for the patients that he was seeing. It was here; this was the light bulb. Family medicine is it. This is the place for me. It has everything that I want to do. It's full spectrum. I can do procedures. I can take care of people chronically, acutely. I can get involved in public health and advocacy and activism and teaching. And aside from all the other specialties, me just loving every single one of them, this was the one that encompassed everything. And I didn't have to choose because I could do it all, which was wonderful.
Dr. Kelly Thibert Going into residency, it was essential that my residency program prepared me for whatever it was that I wanted to do. So, like many of the other folks that you heard, I chose an unopposed program as well. I wanted to be very strong inpatient, outpatient, OB, pediatrics, procedures, teaching – all the things. So that's what I did, and it was wonderful. During residency, I became more heavily involved in the American Academy of Family Physicians. And I was very fortunate and privileged to be elected to serve on the board of the AAFP as a resident director. Here, I expanded my advocacy and activism, education and opportunities even further. So, as I graduated from residency at the beginning part of COVID, so as Dr. Coker was coming in, I was exiting, and it was hard to find a job at that time graduating from residency when the pandemic started. So, I ended up in a position I never thought I would end up in, and as a resident, you need a job, you need money, so I took a job. But I was able to use my advocacy skills to encourage my organization to allow us to expand the population of pediatric patients who were covered by Medicaid, which was huge. I was able to convince them to let us practice gender-affirming healthcare, for which I was the only doctor doing that, eventually on the West Coast of Florida because of how our policies were changing. And so, with that, I was able to also advocate for me to moonlight doing abortion care, and I just got to grow as a first-time new family physician on my own.
Dr. Kelly Thibert And so, with the continuous changes in my home state, my wife and I decided to leave the state of Florida, and we ended up in Las Vegas, here in Nevada, and things have been so incredibly different. Again, I'm no longer providing pediatric care since I'm at the VA Medical Center. But I did let you know in my intro all the cool things I get to do here at this hospital, providing care for our female identified veterans, our LGBTQ veterans, and still teaching students and residents, providing abortion care, and still doing my advocacy and activism. So, I'm super honored and just privileged to be in this space. I'm so happy that I found family medicine. I am so bummed that I've found it so late in medical school, but I'm excited that you all are here learning about it. And so, I think the beauty of family medicine is that we can continuously grow and learn. We can stay the course; we change direction. No matter what, we still have our skill set, and we can ebb and flow with our own lives within our specialty, which is great. And this is the best specialty. I'll say it again, I know I'm biased, but it truly is the best one. Thank you all so much.
Dr. Bright Zhou (host) Wow, thank you so much, Dr. Thibert. And I don't know if you know this, Dr. Thibert and I are twin flames because I entered medical school also wanting to do medical examiner from my path as an archeologist. And I thought that I was going to be a pathologist and all that stuff. So very different paths that brought us here. And I think Dr. Thibert eloquently and beautifully explained how the breadth of family medicine extends in addition to our clinical scope. But also, it extends into all the different kinds of work we do, whether it's teaching, whether it is organized medicine, whether its advocating on the individual level or the systemic level or the micro level of the systemic levels. So, I think there's the breadth that we talk about and that we think of as students that happens clinically, but there's also this incredible other breadth of advocacy work and activism work that we as students are interested in. And I'm so glad that we all get to be on this panel and learn from our panelists. And with that, I'd love to continue hearing about the melding of the breadths and the depths from our next panelist, Dr. McDonald.
Dr. Alex McDonald I'm Alex McDonald. I knew from a relatively young age that I wanted to go into medicine. I taught swimming lessons when I was younger and as a preteen and then did my lifeguard training. And I loved the physiology, the anatomy, the CPR, the first aid better than I liked the lifeguarding and the swimming pieces of it, actually. And so, that's what first got me interested in medicine. I didn't think I was smart enough to go to medical school, honestly, and so I remember very clearly telling my mom, "Oh, you know what, maybe I'll just be an EMT or like a paramedic or someone that doesn't have to go to school until they're like 30." And I don't know, I just felt like I wasn't good enough, honestly. But I pursued, and I persisted. And in college, I found some advisors who were really encouraging for me to do that work. And then I realized I got motion sickness. And so, riding in the back of the ambulance was a really bad idea. So, I nixed that plan pretty early on.
Dr. Alex McDonald Then I went to medical school at University of Vermont. And I didn't really know what I wanted to be. I always loved kids. I was thinking if you'd have asked me when I first started medical school what I want to do, I'd probably say pediatrics. I had an amazing pediatrician growing up who I admired and really enjoyed wanting to work with children. But then I realized it was sort of limiting.
Dr. Alex McDonald And during my third-year rotations, I liked a little bit of everything. If I was on my surgery rotation, I was going to be a surgeon. When I was my cardiology rotation, I was going to be a cardiologist. And I got through the end of third year of medical school, and I really liked everything. I could see myself doing all those things and just wanting to learn as much as possible. And I toyed with ER a little. I thought, "Hey, you know what? I want to be the kind of doctor that treats everything. If I was in an airplane and there's a medical emergency, I want be able to handle that." And initially I thought a little bit about emergency room, but I realized they didn't actually treat the whole patient; they just threw band-aids on things and moved along the way. I love some of my ER colleagues, but that wasn't for me.
Dr. Alex McDonald And then I remember very clearly, again, at the end of third year/beginning of fourth year medical school, my advisor was like, "Well, it sounds like you kind of want to be a family physician," and I didn't even really know what that was. I knew I wanted to be a family physician, but I didn't have a name for it. I didn't know that existed. And then I went into family medicine. I had a little bit of a circuitous journey. I took some time between medical school and residency. Actually, I raced full-time as a professional triathlete for about four years. And during that time, I got hit by a truck and broke both my legs while riding my bike. And so, suddenly, I was a patient. And being a patient in a very dysfunctional healthcare system was a rude awakening. And so, I knew I really wanted to be able to help provide that care and be that grounding for patients moving forward and not just do surgery or give them the medication and send them on their way. I wanted to help treat the whole athlete, so to speak. And so, I realized that a sports medicine fellowship was probably in my future, but within the context of family medicine. I didn't just want to do sports medicine. I really wanted to do a little bit of everything.
Dr. Alex McDonald And so, I found my way to family medicine, and it was a bit of a mistake, a bit of a circuitous journey to get to where I am, but I'm just so incredibly happy. I would have been happy doing anything, I'll be honest. I would've been happy being a surgeon. I would be happy being a pediatrician. But the breadth and the spectrum of what I can do as a family physician is just so powerful, and it makes me so incredibly happy.
Dr. Alex McDonald I have multiple generations of families. I have babies and moms and grandmothers who I take care of, both in the clinic as well as in the hospital (hopefully not too often, but occasionally), and I really enjoy being able to provide that continuous, comprehensive whole-person care. I like to think of family medicine as sort of a web, right? We all have our core competencies, but I do a little bit more sports medicine than some of my colleagues. One of my colleagues does a little more dermatology. And so, we have this ability to grow and flex over our careers. And we all have our area of interest where we do a little bit more, but that's not all of us. And we can kind of grow and flex. And we've been described – Dr. Wanda Feiler makes me think of this term – we are the pluripotent stem cells of the healthcare system. You can take a family doctor and put them in any community, anywhere in the world, and we have skills and tools which we can adapt and build to help that community with their health and to become healthier.
Dr. Alex McDonald Like Dr. Briggs, I found my way to advocacy, wanting to have an impact greater and expand my voice and the breadth and the way that I care for my patients beyond the four walls of the exam room or the hospital. I love treating patients one at a time. I love taking care of patients one at a time. It is the most rewarding thing in the world when a patient stands up and gives me a hug at the end of the visit. But to be able to magnify the scope and the breadth of what I do by teaching medical students, to help encourage them to learn how to practice good medicine so they can go forward and take care of hundreds or thousands of patients. But then also with the advocacy and some of the health policy work that I do. I'm very passionate about social determinants of health. We know that 80 to 90% of what makes a person healthy has nothing to do with medical care. It has to do with where they live, where they work, where they play, who they play with, and those pieces were something that I wanted to have more of an on.
Dr. Alex McDonald So, I started going to Sacramento, and I was blown away by how little our elected officials knew about medicine and knew about health care, even though they were making laws which directly impacted the care that we provide and the way that we provide that care. And so, I continued to go and advocate, and I was like, "This is ridiculous. Why am I just going to advocate for someone else about what's important, about what it means to practice medicine and how we can improve the health of our communities when I can just go do it myself?" And so, I ran for our local school board. Education is the most foundational aspect of good health. We know that people who have better education, have better social mobility, have better access to clean water and fresh foods and health care in general. And so, I decided I'd throw my hat in the ring and put my money where my mouth is and serve as an elected official on my local school board, and it has been an amazing experience to be able to be in the room where it happened, so to speak, to be to help bring the perspective of health and as a healthcare physician.
Dr. Alex McDonald I can go on and on, but I'll stop there. I'm on my six minutes, and I'm just so excited about what I do. If you've seen one family doctor, you've seen one family doctor. Because we do so many different things, and collectively we do everything, but individually we don't do everything because that would be ridiculous.
Dr. Bright Zhou (host) I love that. And I'm laughing because I'm sensing the theme of Dr. McDonald's introduction is flexibility. And to start off with this flexible moment, and we're so glad that I'm hearing that Dr. Walker is back on and ready to come up next, but just wanted to talk about that flexibility and truly how you've modeled flexibility, both deciding to take time off and become a professional athlete and then choosing all the different ways that your path has allowed you to be flexible, while also doing all of the other themes that we've heard from our previous speakers. Being a full spectrum activist, advocate, being a full spectrum clinician, as well as being someone who's rooted in a blend of medical humanities, sciences, arts and people. So, I just love it. I love it; we love family medicine. Thank you so much for sharing that. Next, we are going to hear from Dr. Walker.
Dr. Ryan Walker Thank you all so much. So, for me, I always wanted to be a doctor. I utilized a lot of my undergraduate career to explore and figure out what it was that I wanted to do. I think what had probably the most impact was the experience that I had in my formative years, from the ages of 15 to 22, in serving as a sexual reproductive health advocate and educator. And so, with some focuses on HIV, safer sex practices, and I just enjoy the aspects of organizing community discussions, engaging in conversations about health, about things that are kind of taboo and just making them fun and engaging and dispelling myths – things of that nature. I really wanted to be able to continue these components of building community, having conversations and educating, as well as teaching, into my professional life as a physician. And so, I ultimately decided at the end of undergrad that I want to go into family medicine.
Dr. Ryan Walker At that time, I didn't know a lot about family medicine, but I knew that they got to do a lot of different things. They were in the communities that I was raised in. And so, I was like, "Okay, I want to do that." When I went in at Tufts University, I also knew I wanted to pursue public health. And so, at Tufts, I was in their dual MD/MPH program. And I identified, okay, who are the family med docs here? Fortunately, at Tufts, there's a very strong engagement of family medicine docs throughout the whole curriculum, and so I figured out, "Okay, who should I talk to, and how do I decipher what it was that I wanted to do?"
Dr. Ryan Walker And so, I remember doing a Careers in Medicine aspect, and one of the people that was leading it was a family medicine doctor. And at that time, I was like, "I want to do family medicine, and I want do internal medicine." And there were two dual degree programs. I was like, "These are the two that I looked at." And they're like, “You don't have to do that." And I was, "Wait, what?" And they were like, "You can do family medicine alone and be inpatient." And so, I thought I wanted to be inpatient, and I was going to birth babies and do all these things. And so, then I was like, "Oh, OK, maybe I need to reevaluate." And then eventually, I was, like, "Oh, maybe I also want to do psychology." And so, it was always family medicine and maybe something else. Ultimately, I figured out that I'm just going to do family medicine.
Dr. Ryan Walker Also early on, I decided where I wanted to practice. And so, in doing a lot of my educational work, working with marginalized populations, particularly communities of color that are low social economic status, I decided that I was going to commit to serving at a community health center. And I applied to be a National Health Service Corps scholar. I got the scholarship first year, and I was like, "Okay I'm committed." And so, then I was like, "Wait, I need to find more about community health centers other than just from the aspect of being an educator in my formative years in undergrad." And so, as part of that, during my first year, I was like, "I want to set up community health center visits." And so, I did it. And it was very interesting to learn the breadth of what community health looks like.
Dr. Ryan Walker And so, I was like, "Okay, I want to actually train at a community health center." And so, I trained at Lawrence Family Medicine Residency, which is based in Lawrence, Massachusetts. Our residency is also unopposed. It wasn't the reason why I chose it, necessarily, but it was based in a community health center. And we also work at a hospital, but we're not based within the hospital system. And so, that, I think, afforded me a very different perspective, because we were very clinic heavy, but also very inpatient heavy. And so, part of that was also because we're a four-year program, which is also a bit different. Most residencies are three-year programs, and I think one of the reasons why I did that was because I felt that the curriculum allowed me to be a bit more flexible and delve a little bit more into certain areas of concentration.
Dr. Ryan Walker Many programs may have areas of concentration in which you can utilize more of your elective time to focus on different aspects. Some of that might be HIV, hepatitis B aspects. Some of that may be doing more women's health. I went in and knew I wanted to do integrative medicine. And one of the reasons why I wanted to do that was because in my community, I know oftentimes there are people who don't want to do traditional medicine. I said, "How do I prepare myself to be able to offer other opportunities or alternatives to what I may suggest as an allopathic physician?" And so, moving forward within that, I also found obesity medicine and trained in that during COVID. Because I was able to do it through some non-clinical aspects and then be able to also practice it with integrative medicine.
Dr. Ryan Walker And then moving forward, I also found some medical students that were organizing among themselves during residency and trying to find out what type of residencies they wanted to pursue. And I ultimately developed an “Apply Into Residency” series for them. And that group of students turned into the Association of Black Family Medicine Physicians. And so, here I was finding myself on the board trying to organize how do we talk about taboos of being a Black person within medicine, a Black person within family medicine, and self-advocacy for our ourselves and community and building communities among the nation. And, we've engaged a lot of IMG students, which are integrative medicine graduate students.
Dr. Ryan Walker So, in that aspect, I've been able to learn a lot about different experiences across the country among residents and in my own clinical space. I work part-time. I decided that while I love outpatient medicine, I couldn't do it full-time, and I wanted to be able to have the time to run ABFMP as a nonprofit organization. And do more teaching at Tufts. And so, I do that both in a clerkship aspect clinically, and then I also do that by helping to organize and plan and teach within the perspectives in medicine course, where we do focus on social determinants of health, talking about the patient experience and how do we integrate interdisciplinary aspects of medicine. I'm going to stop there, and I'm excited to answer some additional questions.
Dr. Bright Zhou (host) Thank you so much, Dr. Walker. And as I'm hearing your story, I'm really, really impressed by the trust that you've been able to build from the start of your career in the communities that you serve. I think that starting from your work as a sexual health counselor to your work now in ABFM really relies on both getting trust, but then also developing that trust into a form of advocacy in itself. And that's something we've heard from our other panelists as well. Both in terms of the trust that exists within a clinic room, as well as the trust exists way outside of it and all the different forms that exist, as Dr. McDonald said, outside of the four walls of our clinic.
Dr. Bright Zhou (host) With our last four minutes left, I'd like to ask each panelist to answer one last question that our lovely staff have prepared before we say good night. The question is: what do you wish you had known about family medicine when you applied into it? If you had to do it over again, would you still choose family medicine? I can see why they just called this one question, because I'm sure we all will say “yes.” But the first question I'm very interested in is: What do you wish you had known about family medicine when you applied? And anyone can start.
Dr. Emily Briggs I can answer that. I would say that to do a preceptorship, when I was in my clinicals in my medical school years, I didn't realize early on that I could go and rotate with different family docs and see what it was like to do community-based or academic-based, or the different types of programs. As Alex mentioned earlier, plasticity is what some people call the "jewel" of family medicine. That's what we are. We have great plasticity. We can fit in anywhere. Shawn Martin, I think, might've coined that. But to do a preceptorship is what I wish I had known about.
Dr. Alex McDonald I'll go next. I wish I knew how challenging, yet exciting, yet rewarding family medicine is and will be. Never, ever, ever, ever let anyone tell you that you're too smart to go into family medicine because it's a lie. It's a lie. Family medicine is probably one of the most challenging specialties, because you have to know so much about so many different things. So, that's the one thing I wish I knew and had more confidence as a medical student to stand up and say, "Well, maybe if you were only smart enough to learn one organ system, family medicine is not right for you." So, anyway, I digress. No shade to our amazing colleagues, but that's what I wish I knew. And clearly, I would go into family medicine again if I had the choice.
Dr. Ian Coker I can go. I mean, hopefully this panel has been helpful for you to see that there's a lot of different ways to do family medicine. And I guess when you're a student, sometimes you think you know because you've seen a few things, right? But someone said earlier, if you've met one family doctor, you've met one family doctor. So, I guess I wish I had really an understanding of just how many ways you can go about this and that doing any of these ways does not make you any less of a family doctor just because you're not doing what everybody thinks a family doctor's supposed to do. And yes, I would definitely do it again.
Dr. Ryan Walker I will say that I don't know if you all were able to tell, but I'm an avid planner. And so, I'm like, "I plan, and it's supposed to move this way." And I think what I realized, especially when applying to residencies, is that there can be a season within family medicine. I wish that I was like, "Okay, I don't have to have all of the things, but I can think that maybe, at this point in my time, it may look this way, it might look a different way." And there will be times in which you might focus on one aspect. And so, I think, for me, having grace within family medicine, because I want to do it all; I can't always do it all at the same time. And so, realizing that there may be a time and a season for everything. And I would most certainly do family medicine again.
Dr. Kelly Thibert I wish I had known more family medicine doctors. The initial folks who encouraged me to look at family medicine were the OBGYNs that I was rotating with, who I was telling every day all the things I love. But I was nervous about not being able to do procedures or abortion care, and they were like, "No, family medicine can do it all. You should probably check that out." And it was so important to hear that from attending physicians. So, I think had I been involved in the AAFP as a medical student and gotten to know all the breadth and all these different family docs who do incredible things, it would have solidified my decision so much earlier on in my career. And I would 100% choose it again. I just would have chosen it sooner and would have been so much happier because I would have had even more time in this specialty and within the AAFP.
Dr. Bright Zhou (host) Amazing, incredible. Thank you so much to our panel. My answer to what I wish I would have known is: I wish I had watched this panel. I wish this panel was available to me, and luckily it will be available to all of you for free.
Dr. Bright Zhou (host) Reminder that AAFP membership is also free for medical students. So please join us at aafp.org/join. Thank you again to all our esteemed colleagues and panelists.