Poverty and Health - The Family Medicine Perspective (Position Paper)
Introduction
Poverty is a complex and insidious determinant of health caused by systemic factors that can persist for generations in a family. Beginning before birth and continuing throughout an individual’s life, poverty can significantly impact health and health outcomes. The vision of the American Academy of Family Physicians (AAFP) is to transform health care to achieve optimal health for everyone. Primary care physicians and public health professionals continue to collaborate on a shared vision of improving population health. As the integration of primary care and public health continues, this shared vision becomes even more relevant, focused, and clear. Success in this new era means achieving better outcomes by transforming health care to overcome obstacles related to the social, environmental, and community determinants of health – including poverty.1,2,3,4
Family physicians have a unique perspective on local population’s health challenges because we serve generations of families and follow individual patients through different life stages. We are privileged to share the complex stories of individuals and families in sickness and health over long periods and across different care settings. Rather than viewing a single snapshot of a patient during an episode of illness, we know the patient’s whole story. We know the environmental, patient, and family factors that lead to illness and disease – and the patient’s need to manage their condition effectively. As lifelong collaborators in care, family physicians are well-positioned to understand each patient’s unique obstacles to better health and help overcome them.
Call to Action
The AAFP urges its members to become informed about the impact of poverty on health. Achieving the vision of optimal health for everyone requires a culturally proficient care team and a well-resourced medical neighborhood that supplies readily accessible solutions. Family physicians play a critical role in community health and can contribute through bold efforts in many areas. When these solutions are incorporated seamlessly into everyday practice workflows, family physicians and care teams can be true to the AAFP’s vision by achieving positive change for individuals, families, and communities, and improve population health.
The AAFP calls for action in the following areas:
Physician Level
- Become more informed about the impact of the social determinants of health (SDoH) and identify tangible next steps you can take to address and reduce health inequities
- Be aware of, and sensitive to, your patient’s specific circumstances to help them achieve their health goals
Practice Level
- Identify critical factors that impact patient health, leveraging The EveryONE Project and data collection on SDoH in electronic health records (EHRs)
- Understand each patient’s unique challenges and coping strategies and know what community resources are available
Community-Leadership Level
- Promote alignment with other private and public community resources to help advance the integration of primary care and public health
- Partner with other health care and social service organizations to connect directly to resources that mitigate poverty’s effect on health
Educational Level
- Drive change in undergraduate and graduate medical education to ensure future physicians are adequately prepared to prevent and address disparities caused by SDoH
Advocacy Level
- Work with local, state, and national governments to adopt a Health in All Policies approach that prioritizes health within goals and agenda-setting
- Advocate for regulatory frameworks and economic incentives to ensure public health and population health are critical to individual health care efforts
Understanding Poverty and Low-income Status
Poverty occurs when an individual or family lacks the resources to provide life necessities, such as food, clean water, shelter, and clothing. It also includes a lack of access to such resources as health care, education, and transportation.5 In the United States, federal poverty is expressed as an annual pre-tax income level indexed by the size of household and age of household members. For example, in 2020, the federal poverty income level was $12,760 for an individual younger than 65 years and $26,200 for a family of four.6 In 2019, approximately 10.5% of Americans were living below the poverty line. While overall poverty rates had been declining in the past several years, inequalities remain by SDoH, including race and racism, ethnicity, educational attainment, and disability status.7
The term “low income” generally describes individuals and families whose annual income is less than 130-150% of the federal poverty income level. For example, the Supplemental Nutrition Assistance Program (SNAP) is available to individuals with a gross monthly income of 130% of the federal poverty income level.8 Medicaid is open to families with an income of 138% of the poverty income level.9
Poverty and low-income status are associated with various adverse health outcomes, including shorter life expectancy, higher infant mortality rates, and higher death rates for the 14 leading causes of death.10,11 Individual- and community-level mechanisms mediate these effects.12 For individuals, poverty restricts the resources used to avoid risks and adopt healthy behaviors.13 Poverty also affects the built environment (i.e., the human-made physical parts of the places where people live, work, and play, including buildings, open spaces, and infrastructure), services, culture, and communities’ reputation, all of which have independent effects on health outcomes.14
Location matters, and there are often dramatic differences in health care delivery and health outcomes between communities that are only a few miles apart. For example, the Robert Wood Johnson Foundation (RWJF) found a 25-year difference in average life expectancy in New Orleans, LA, between inner city and suburban neighborhoods. Similarly, there is a 14-year difference in average life expectancy between two Kansas City, MO, neighborhoods that are roughly three miles apart.15
A study by The Commonwealth Fund assessed 30 indicators of access, prevention, quality, potentially avoidable hospital use, and health outcomes. The study found that populations with low-income status suffer disparities in every state. However, it also identified significant differences among states’ performances. For top-performing states, many health care measures of populations with low income were better than average and better than those for individuals with higher income or more education in lagging states. These findings indicate that low-income status does not have to determine poor health or poor care experience. Interventions seen in top-performing states, such as expanded insurance coverage, access, and coordination of social and medical services, can help mitigate poverty’s effects on health.16
SDoH are the conditions under which people are born, grow, live, work, and age, and include factors such as socioeconomic status, education, employment, social support networks, and neighborhood characteristics.4 These social factors have a more significant collective impact on health and health outcomes than health behavior, health care, and the physical environment.17,18 SDoH, especially poverty, structural racism, and discrimination, are the primary drivers of health inequities.19,20
Economic prosperity can provide individuals access to resources to avoid or buffer exposure to health risks.21 Research shows that individuals with higher incomes consistently experience better health outcomes than individuals with low incomes and those living in poverty.22 Poverty affects health by limiting access to proper nutrition and healthy foods; shelter; safe neighborhoods to learn, live, and work; clean air and water; utilities; and other elements that define an individual’s standard of living. Individuals who live in low-income or high-poverty neighborhoods are likely to experience poor health due to a combination of these factors.23,24
Violence is also more prevalent in areas with greater poverty. From 2008 to 2012, individuals in households at or below the poverty level experienced more than double the rate of violent victimization than individuals in high-income households.25 This pattern of victimization by violent behavior was consistent for both Black and white individuals. It significantly impacts the victim’s family and perpetrator’s family (through incarceration).
Because they intersect with so many SDoH, poverty and low-income status dramatically affects life expectancy.26 Education and its socioeconomic status correlate to income and wealth. These have powerful associations with life expectancy for both sexes and all races at all ages. Students from families with low income are five times more likely to drop out of high school than students from families with high income.27 In 2008, the life expectancy among U.S. adult men and women with fewer than 12 years of education was not much better than the life expectancy among all adults in the 1950s and 1960s.28
Poverty affects individuals insidiously in other ways that we are just beginning to understand. Mental illness, chronic health conditions, and substance use disorders are all more prevalent in populations with low income.29 Poor nutrition, toxic exposures (e.g., lead), and elevated levels of the stress hormone cortisol are factors associated with poverty that may have lasting effects on children beginning before birth and continuing after birth. These effects, which can influence cognitive development and chronic disease development, are dose-dependent (i.e., the duration of exposure matters).30,31,32 For example, the greater the number of years a child spends living in poverty, the more elevated the child’s overnight cortisol level and the more dysregulated the child’s cardiovascular response to acute stressors.31 Impaired development of the nervous system affects cognitive and socioemotional development and increases the risk of behavioral challenges, adverse health behaviors, and poor school performance.31,32 Recent studies have even identified a strong association between pediatric suicide and county-level poverty rates.33
However, the effects of poverty are not predictably uniform. Longitudinal studies of health behavior describe positive (e.g., tobacco use cessation) and negative (e.g., decrease in physical activity) health behavior trends in populations with lower and higher socioeconomic status. However, there is a socioeconomic gradient in health improvement. In other words, populations with lower socioeconomic status lag behind populations with higher socioeconomic status in positive gains from health behavior trends. Health behaviors are important in that they account for differences in mortality.34 The fact that positive changes in health behaviors are possible despite the challenges of poverty points to the importance of developing and implementing interventions that promote healthy behaviors in populations with low income.
Risk Regulators and Intervention
Poverty affects health in many different ways through complex mechanisms that we are just beginning to understand and describe. Living in poverty does not necessarily predetermine poor health.35 Poverty will not “cause” a disease. Instead, poverty affects both the likelihood that an individual will have risk factors for disease and its ability and opportunity to prevent and manage disease. An individual’s health outcomes (a physiologic expression) ultimately will be influenced by genetic and environmental factors, as well as health behaviors – all of which may be affected by poverty. Material conditions, discriminatory practices, neighborhood conditions, behavioral norms, work conditions, as well as laws, policies, and regulations associated with poverty make it a “risk regulator.”35 This means that poverty functions as a control parameter at a system level to influence the probability of exposure to key risk factors (e.g., behaviors, environmental risks) that lead to disease (Figure 1).
Figure 1: An Illustration of Risk Regulators in Social and Biological Context
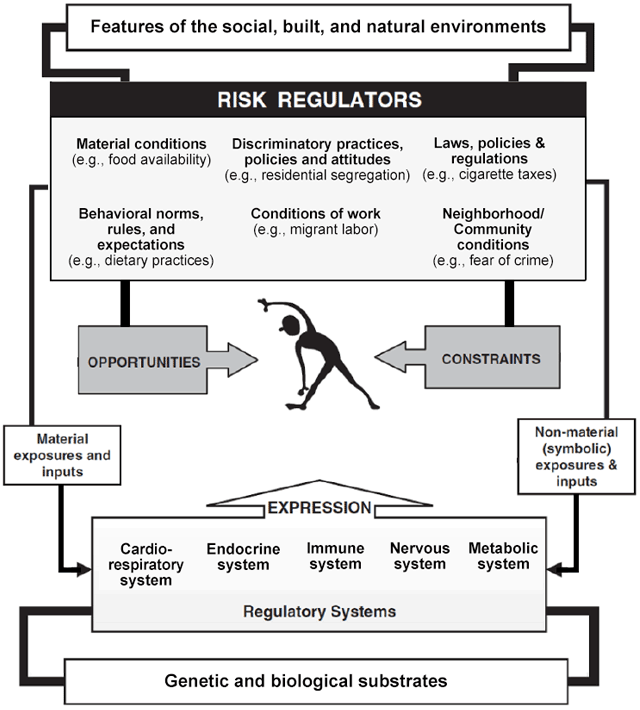
Reprinted with permission from Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650-1671.
Thinking of poverty as a risk regulator rather than a rigid determinant of health allows family physicians to relinquish the feeling of helplessness when providing medical care to families and individuals with low income.
Family physicians are uniquely positioned to devise solutions to mitigate the development of risk factors that lead to disease and the conditions unique to populations with low income that interfere with effective disease prevention and management. They can boost an individual or family’s “host resistance” to the health effects of poverty and tap into a growing array of aligned resources that provide patients and families with tangible solutions so that health maintenance can be a realistic goal.
Community-Oriented Primary Care (COPC)
Strong primary care teams are critical in the care of patients with low income. These populations often have higher rates of chronic disease and difficulty navigating health care systems. They benefit from care coordination and team-based care that addresses medical and socioeconomic needs.
In the United States, there is a move toward increased payment from government and commercial payers to offset the cost of providing coordinated and team-based care. Some payment models provide shared savings or care coordination payments in addition to traditional fee-for-service reimbursement. The practice transformations from COPC and payment models based on targets and meaningful use alter how we approach patient panels and communities.36 The rationale behind alternative payment models – particularly regarding the care of lower socioeconomic populations – is that significant cost savings can be realized when care moves toward prevention and self-management and away from crisis-driven, fragmented care provided in the emergency department or a hospital setting. By recognizing and treating disease earlier – and actively partnering with local public health services like health educators, community health workers, and outreach services – family physicians can help prevent costly, avoidable complications and reduce the total cost of care.
Community Responsive Care
Care team members can positively affect the health of patients with low income by creating a welcoming, nonjudgmental environment that supports a long-standing therapeutic relationship built on trust. Familiarity with the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care can prepare practices and institutions to provide care in a manner that promotes health equity.37
Patients with low income may be unintentionally shamed by the care team when their behaviors are seen as evidence of being “noncompliant” (e.g., missing appointments, not adhering to a medical regimen, not getting tests done). These patients may not be comfortable sharing information about the challenges that lead to their “noncompliant” behaviors. For example, a patient with low income may arrive 15 minutes late to an appointment because they have to rely on someone else for transportation. A patient may not take prescribed medication because it is too expensive. A patient may not get tests done because their employer will not allow time off from work. A patient may not understand printed care instructions because of low-literacy skills. Such patients may be turned away by staff because their tardiness disrupts the schedule, or they may even be dismissed from the practice altogether because of repeated noncompliance. Physicians and care team members should learn why the patient was noncompliant and promote an atmosphere of tolerance and adaptation.
Patients with low socioeconomic status and other marginalized populations rarely respond well to dictation from health care professionals. Instead, interventions that rely on peer-to-peer storytelling or coaching are more effective in overcoming cognitive resistance to positive health behavior changes.38 Physicians and care team members can identify local groups that provide peer-to-peer support. Such activities are typically hosted by local hospitals, faith-based organizations, health departments, or senior centers.
Screen for Socioeconomic Challenges
Family physicians regularly screen for risk factors for disease. Screening to identify patients’ socioeconomic challenges and other SDoH can be incorporated into practices using EveryONE Project tools. Once socioeconomic challenges are identified, physicians and their care teams can work with patients to design achievable, sustainable treatment plans. The simple question, “Do you (ever) have difficulty making ends meet at the end of the month?” has a sensitivity of 98% and specificity of 60% in predicting poverty.39 A casual inquiry about the cost of a patient’s medications is another way to start a conversation about socioeconomic obstacles to care.
A patient’s home and neighborhood affect health.40 The care team should ask the patient whether their home is adequate to support healthy behaviors. For example, crowding, infestations, and lack of utilities are all risk factors for disease. Knowing that a patient is homeless or has poor, inadequate housing will help guide care.
Set Priorities and Make a Realistic Plan of Action
Family physicians direct the therapeutic process by working with the patient and care team to identify priorities so treatment goals are clear and achievable. In many cases, suspending a “fix everything right now” agenda in favor of a treatment plan of small steps that incorporate shared decision making can help this process. It is likely that a patient with low income will not have the resources (e.g., on-demand transportation, forgiving work schedule, available child care) to comply with an ideal treatment plan. Formulating a treatment plan that makes sense for the patient’s life circumstances is vital to success.
For example, for a patient with limited means and multiple chronic conditions – including hypertension and diabetes – start by addressing these conditions. Colon cancer screening or a discussion about beginning statin therapy can come later. It may be easier for this patient to adhere to an insulin regimen involving vials and syringes instead of insulin pens, which are much more expensive. The “best” medication for a patient with low income is the one that the patient can afford and self-administer reliably. Celebrate success with each small step that takes a patient closer to disease control and improved self-management.
Help Newly Insured Patients Navigate the Health Care System
In many states, the expansion of Medicaid has allowed individuals and families with low income to become insured – perhaps for the first time. A newly insured individual with low income will not necessarily know how or when to make, keep, or reschedule an appointment; develop a relationship with a family physician; manage medication refills; or obtain referrals. They may be embarrassed to reveal this lack of knowledge to the care team. Physicians and care team members can help by providing orientation to newly insured patients within the practice. For example, ensure that all patients know where to pick up medication, how to take it and why, when to return for a follow-up visit and why, and how to follow their treatment plan from one appointment to the next. Without this type of compassionate intervention, patients may revert to an old pattern of seeking crisis-driven care often provided by the emergency department or a local hospital.
Provide Material Support to Families with Low Income
Resources that make it easier for busy physicians to provide support to families with low income include the following:
● Reach Out and Read is a program that helps clinicians provide books for parents to take home to read to their children. Studies have shown that Reach Out and Read improve children’s language skills.41
● 2-1-1 is a free, confidential service that patients or staff can access 24 hours a day by phone. 2-1-1 is staffed by community resource specialists who can connect patients to resources such as food, clothing, shelter, utility bill relief, social services, and even employment opportunities. Follow-up calls are made to ensure clients connect successfully with the resource referrals.
● The National Domestic Violence Hotline is staffed 24 hours a day by trained advocates who provide confidential help and information to patients who are experiencing domestic violence.
Local hospitals, health departments, and faith-based organizations often are connected to community health resources that offer services such as installing safety equipment in homes; providing food resources; facilitating behavioral health evaluation and treatment; and providing transportation, vaccinations, and other benefits to individuals and families with low income.
Practices can make a resource folder of information about local community services that can be easily accessed when taking care of patients in need. This simple measure incorporates community resources into the everyday workflow of patient care, thus empowering the care team.
Participate in Research that Produces Relevant Evidence
Much of the research about the effects of poverty on health is limited to identifying health disparities. This is insufficient. Research that evaluates specific interventions is needed to gain insight into what effectively alleviates poverty’s effects on health care delivery and outcomes. Family physicians can serve a critical role in this research because we have close relationships with patients with low income.42
Advocate on Behalf of Neighborhoods and Communities with Low Income
Family physicians are community leaders, so we can advocate effectively for initiatives that improve the quality of life in neighborhoods with low income. Some forms of advocacy are apparent, such as promoting a state’s expansion of Medicaid. Other efforts may be specific to the community served. For example, a vacant lot can be converted to a basketball court or soccer field. A community center can expand programs that involve peer-to-peer health coaching. A walking program can be started among residents in a public housing unit. Collaboration with local law enforcement agencies can foster the community’s trust and avoid the potential for oppression.43
Family physicians have local partners in advocacy, so we do not have to act in isolation. As a result of the Patient Protection and Affordable Care Act (ACA), nonprofit hospitals regularly report community needs assessments and work with local health departments to establish action plans that address identified needs. A Community Health Needs Assessment (CHNA) reflects a specific community’s perception of need, and each action plan outlines multi-sectoral solutions to meet local health needs. Local CHNAs are typically available online, as are the associated action plans. Family physicians can use information in the CHNA to access local health care leadership and join aligned forces in the communities we serve, thereby supporting the AAFP’s vision of achieving optimal health for everyone.
References
1. Sherin K, Adebanjo T, Jani A. Social determinants of health: family physicians’ leadership role. Am Fam Physician. 2019;99(8):476-477.
2. Commission on Social Determinants of Health. Closing the gap in a generation. Health equity through action on the social determinants of health. World Health Organization (WHO). Accessed March 22, 2021. www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf
3. Kovach KA, Reid K, Grandmont J, et al. How engaged are family physicians in addressing the social determinants of health? A survey supporting the American Academy of Family Physician’s health equity environmental scan. Health Equity. 2019;3(1):449-457.
4. American Academy of Family Physicians (AAFP). Advancing health equity by addressing the social determinants of health in family medicine (position paper). Accessed March 22, 2021.
5. World Vision. What is poverty? It’s not as simple as you think. Accessed March 22, 2021. www.worldvision.ca/stories/child-sponsorship/what-is-poverty#:~:text=1.-,What%20is%20the%20definition%20of%20poverty%3F,care%2C%20education%20and%20even%20transportation
6. Office of the Assistant Secretary for Planning and Evaluation. 2020 poverty guidelines. Accessed March 22, 2021. https://aspe.hhs.gov/2020-poverty-guidelines
7. United States Census Bureau. Income, poverty and health insurance coverage in the United States: 2019. Accessed March 22, 2021. www.census.gov/newsroom/press-releases/2020/income-poverty.html
8. United States Department of Agriculture. SNAP special rules for the elderly or disabled. Accessed March 22, 2021. www.fns.usda.gov/snap/eligibility/elderly-disabled-special-rules
9. U.S. Centers for Medicare & Medicaid Services. Federal poverty level (FPL). Accessed March 22, 2021. www.healthcare.gov/glossary/federal-poverty-level-fpl/
10. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80-94.
11. Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child. 1997;7(2):55-71.
12. Berkman LF, Kawachi I. A historical framework for social epidemiology. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2014.
13. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51 Suppl:S28-S40.
14. Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125-139.
15. Robert Wood Johnson Foundation. Mapping life expectancy. Short distances to large gaps in health. Accessed March 22, 2021. www.rwjf.org/en/library/articles-and-news/2015/09/city-maps.html
16. Schoen C, Radley D, Riley P, et al. Health care in the two Americas. Findings from the Scorecard on State Health System Performance for Low-Income Populations, 2013. Accessed March 22, 2021. www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2013_sep_1700_schoen_low_income_scorecard_full_report_final_v4.pdf
17. Booske BC, Athens JK, Kindig DA, Park H, Remington PL. County health rankings working paper. Different perspectives for assigning weights to determinants of health. University of Wisconsin Population Health Institute. Accessed March 22, 2021. www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf
18. County Health Rankings & Roadmaps. County Health Rankings model. Accessed March 22, 2021. www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model
19. Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51 Suppl:S28-S40.
20. National Academies of Sciences, Engineering, and Medicine. Communities in action. Pathways to health equity. Accessed March 22, 2021. www.nap.edu/catalog/24624/communities-in-action-pathways-to-health-equity
21. Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Task Force on Community Preventive Services. The Community Guide’s model for linking the social environment to health. Am J Prev Med. 2003;24(3 Suppl):12-20.
22. Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000.
23. Riste L, Khan F, Cruickshank K. High prevalence of type 2 diabetes in all ethnic groups, including Europeans, in a British inner city: relative poverty, history, inactivity, or 21st century Europe? Diabetes Care. 2001;24(8):1377-1383.
24. Healthy People 2030. Social determinants of health. Accessed March 22, 2021. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
25. Bureau of Justice Statistics. Household poverty and nonfatal violent victimization, 2008-2012. Accessed March 24, 2021. www.bjs.gov/index.cfm?ty=pbdetail&iid=5137
26. Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750-1766.
27. National Center for Education Statistics. Trends in high school dropout and completion rates in the United States: 1972–2009. Accessed March 24, 2021. https://nces.ed.gov/pubs2012/2012006.pdf
28. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803-1813.
29. Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the United States. Psychol Health Med. 2017;22(6):727-735.
30. Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18(11):953-957.
31. Lipina SJ, Colombo JA. Poverty and Brain Development During Childhood: An Approach from Cognitive Psychology and Neuroscience. Human Brain Development Series. Washington, DC: American Psychological Association; 2009.
32. Farah MJ, Noble KG, Hurt H. Poverty, privilege, and brain development: empirical findings and ethical implications. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice, and Policy. New York: Oxford University Press; 2005.
33. Hoffmann JA, Farrell CA, Monuteaux MC, et al. Association of pediatric suicide with county-level poverty in the United States, 2007-2016. JAMA Pediatr. 2020;174(3):287-294.
34. Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159-1166.
35. Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62(7):1650-1671.
36. American Academy of Family Physicians. Integration of primary care and public health (position paper). Accessed March 24, 2021. www.aafp.org/about/policies/all/integration-primary-care.html
37. U.S. Department of Health and Human Services. National CLAS Standards. Accessed March 24, 2021. https://thinkculturalhealth.hhs.gov/clas
38. Houston TK, Allison JJ, Sussman M, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011;154(2):77-84.
39. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med. 2011;2011:812182.
40. Braveman P, Dekker M, Egerter S, Sadegh-Nobari T, Pollack C. Housing and health. Robert Wood Johnson Foundation. Accessed March 24, 2021. www.dhss.delaware.gov/dhss/dph/mh/files/housingandhealth.pdf
41. Zuckerman B. Promoting early literacy in pediatric practice: twenty years of Reach Out and Read. Pediatrics. 2009;124(6):1660-1665.
42. O’Campo P, Dunn JR, eds. Rethinking Social Epidemiology: Towards a Science of Change. New York, NY: Springer; 2012.
43. President's Task Force on 21st Century Policing. Interim report of the President's Task Force on 21st Century Policing. Office of Community-Oriented Policing Services. Accessed March 21, 2021. https://cdpsdocs.state.co.us/ccjj/meetings/2015/2015-03-13_CCJJ_Presidents-21CentCommPolicingTF-InterimReport.pdf
(2015 COD) (January 2022 COD)