Am Fam Physician. 2013;88(11):757-761
Author disclosure: No relevant financial affiliations.
Vasectomy offers a safe, effective, and permanent method of male contraception, with an overall failure rate of less than 1% in pooled studies. Men older than 30 years in a stable, committed relationship appear to be the best candidates for vasectomy. The no-scalpel technique reduces operative complications, shortens operative time, and hastens resumption of sexual activity. Use of a jet injector instead of a needle to provide local anesthesia (no-needle vasectomy) may reduce pain. Bleeding and infection are short-term complications of vasectomy; long-term complications include sperm granuloma and postvasectomy pain syndrome. One postvasectomy semen analysis demonstrating azoospermia performed after three months and 20 ejaculations is sufficient to establish sterility. Vasectomy reversal is more likely to be successful if performed less than 15 years after vasectomy and in men whose female partner is younger than 40 years.
Vasectomy is a safe, reliable, and cost-effective option for permanent contraception in men. Of the more than 525,000 vasectomies done each year in the United States, family physicians perform approximately 13%.1 This article reviews common questions about vasectomy and presents evidence-based answers.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The no-scalpel technique is preferred for gaining access to the vas deferens during vasectomy. | B | 2 |
| Fascial interposition should be incorporated with the vasal occlusion technique during vasectomy. | A | 6 |
| One postvasectomy semen analysis demonstrating azoospermia performed after three months and 20 ejaculations is sufficient to establish sterility. | B | 4 |
| Recommendation | Sponsoring organization |
|---|---|
| Avoid routine preoperative testing for low-risk surgeries without a clinical indication. | American Society for Clinical Pathology |
What Are the Advantages of No-Scalpel Vasectomy?
No-scalpel vasectomy, in contrast to the traditional incisional technique, is a minimally traumatic approach to accessing the vas deferens that reduces operative complications, shortens operative time, and hastens resumption of sexual activity. No-scalpel vasectomy is therefore the preferred technique.2
EVIDENCE SUMMARY
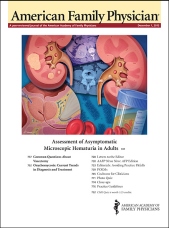
The traditional approach to accessing the vas deferens relies on a short scrotal skin incision made using a scalpel. Instead of making an incision, no-scalpel vasectomy uses a sharp, pointed hemostat (Figure 1) to puncture a small opening in the scrotal skin. A systematic review of two randomized controlled trials (RCTs) demonstrated the superiority of no-scalpel vasectomy over the incisional method in decreasing clinically relevant outcomes such as intraoperative bleeding (odds ratio [OR] = 0.49), postoperative hematoma (OR = 0.23), perioperative pain (OR = 0.75), postoperative pain (OR = 0.63), and postsurgical infection (OR = 0.21).2 Secondary outcomes such as shorter intraoperative time (OR = 2.4, six minutes or less; OR = 0.56, 11 minutes or more) and faster resumption of sexual activity were also better for no-scalpel vasectomy.2
What Are the Advantages of No-Needle Vasectomy?
No-needle vasectomy involves an alternative technique of administering local anesthesia using a high-pressure jet injector. It may reduce pain associated with local anesthetic infiltration.
EVIDENCE SUMMARY
No-needle vasectomy is an increasingly popular alternative to the standard local infiltration technique that uses a hypodermic needle. This technique uses a jet injection device (Figure 2) to deliver high-pressure anesthetic spray through intact skin and into the vas and surrounding tissues. A small single-blind RCT involving 50 patients demonstrated a statistically significant improvement in pain from anesthetic administration with no-needle vasectomy compared with needle injection. However, there was no difference in intraoperative pain between the two techniques.3 Although the jet injector can prevent injury from needlestick and eliminate the burden of syringe and needle disposal, its disadvantages include the initial cost of the device and the potential for inadvertent self-injection of the physician's middle finger through a scrotal exit wound created by the high-pressure spray when using the three-finger technique for vas isolation.

How Effective Is Vasectomy?
Vasectomy is the most effective and the only permanent method of male contraception, with a failure rate of less than 1% in pooled studies.4,5 Management of the vasal ends, which determines the procedure's effectiveness, can be accomplished in various ways but fascial interposition should be used routinely because it decreases vasectomy failure rates significantly.
EVIDENCE SUMMARY
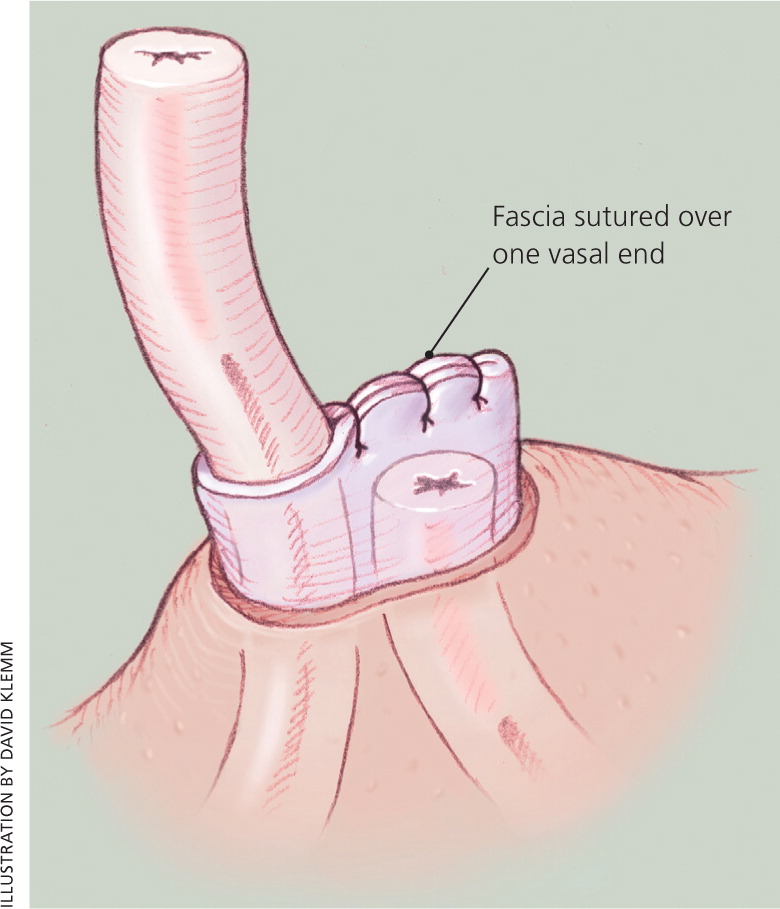
A systematic review of six RCTs demonstrated no difference in failure rate between the ligation and excision technique compared with vas occlusion with surgical clips (without transection of the vas).6 The same study evaluated the effects of fascial interposition (Figure 37 ), a method of burying one vasal end within the vasal sheath or surrounding connective tissue to separate the anatomic plane between the two vasal ends, hence minimizing the risk of recanalization. Fascial interposition was found to significantly reduce vasectomy failure at 34 weeks compared with no fascial interposition (OR = 0.42); however, it lengthened the operative time by two to three minutes.6 Vas irrigation with water (vs. no water) or with spermicidal agent (vs. water) has not been shown to decrease vasectomy failure rates. No RCT has evaluated the effectiveness of fulguration or electrocautery to occlude the vasal ends, or examined leaving the vasal ends open (without the use of sutures, clips, or fulguration).6
What Are the Complications of Vasectomy?
Bleeding and infection are short-term complications of vasectomy; long-term complications include sperm granuloma and postvasectomy pain syndrome.
EVIDENCE SUMMARY
Bleeding and hematoma formation, the most common complications of vasectomy, often result from injury to the pampiniform venous plexus. Perioperative bleeding occurs in 2.4% of no-scalpel vasectomies and 4.0% of incisional vasectomies, whereas hematoma occurs in 2.4% of no-scalpel vasectomies and 12.5% of incisional vasectomies.2 In extreme cases, these complications can lead to significant morbidity necessitating surgical interventions such as hemostasis, scrotal exploration, and hematoma evacuation. Postoperative infection occurs in 0.7% of no-scalpel vasectomies and 2.2% of incisional vasectomies.2
A sperm granuloma forms as an immunologic reaction to the extravasation of sperm from the testicular vasal end. This process is hypothesized to be protective because it prevents epididymal and testicular obstruction. Although most sperm granulomas are not painful and often disappear over time, they are believed to play a role in postvasectomy pain syndrome and recanalization during vasectomy failure.8
Postvasectomy pain syndrome is persistent or recurrent scrotal pain that occurs months or years after vasectomy. It is thought to be caused by underlying chronic epididymal congestion. Recent studies estimate the incidence of severe postvasectomy pain syndrome to be between 1% and 6%.9,10 Mild postvasectomy pain syndrome is treated symptomatically, whereas severe cases may require vasectomy reversal.
When and How Should Semen Analysis Be Performed to Check Sterility?
One postvasectomy semen analysis demonstrating azoospermia performed after three months and 20 ejaculations is sufficient to establish sterility.4 The entire ejaculate should be obtained after a period of abstinence of two days (but no more than seven days), kept at body temperature, transported within 60 minutes of collection, and analyzed in the laboratory within four hours of ejaculation.
EVIDENCE SUMMARY
The lack of standardized postvasectomy semen analysis protocols in vasectomy studies has made it difficult to accurately measure failure rates. A systematic review of 56 studies suggested that about 80% of patients achieve azoospermia three months after vasectomy and after 11 to 20 ejaculations.4 A small number of patients (1.4%) had persistent nonmotile sperm after vasectomy; some eventually achieved azoospermia.4 The British Andrology Society recommends that patients with persistent nonmotile sperm undergo monthly postvasectomy semen analysis until one test demonstrates azoospermia or two consecutive tests demonstrate low numbers of nonmotile sperm (< 100,000 per mL) and seven months have elapsed since vasectomy. The latter group may also stop using contraception because the probability of pregnancy is extremely low.5,11
Assuming vasal disruption and occlusion have been adequately achieved during surgery, and assuming the patient adheres to using another contraceptive method while awaiting confirmation of sterility, true causes of vasectomy failure include recanalization (early and late) and, more rarely, aberrant anatomy (e.g., the presence of a third vas). The presence of motile spermatozoa during the three-month postvasectomy semen analysis likely represents vasectomy failure and should be confirmed with another semen analysis one month later. Once motile spermatozoa are reconfirmed, patients should be notified and repeat vasectomy recommended. Recanalization following vasectomy is rare (0.4%) and pregnancy is even rarer (0.07%).4
According to World Health Organization protocols, the entire ejaculate should be obtained by masturbation after a period of abstinence of two days (but no more than seven days), collected in a nontoxic container, kept at body temperature at all times, transported within 60 minutes of collection, and analyzed in the laboratory within four hours of ejaculation. Exceptions to this rigorous protocol can be made if there are extenuating circumstances. However, if sperm motility needs to be verified, this protocol must be followed exactly.5,12
A common issue with postvasectomy semen analysis is compliance. In a review of 29 studies, a median of 19% of patients (range: 0% to 63%) failed to provide any semen sample. Of those who sent a semen sample, a median of 5% (range: 0% to 41%) only partially complied with the instructions.4 In response to this compliance issue, a novel, qualitative home test has been developed that can accurately detect sperm counts < 250,000 per mL (positive predictive value = 93%; negative predictive value = 97%). Although approved by the U.S. Food and Drug Administration, this test cannot assess sperm motility and is not yet supported by robust patient-oriented data in larger clinical trials.13
How Successful Is Vasectomy Reversal?
Microsurgical reconstructive techniques for vasectomy reversal have varying success rates. Two important predictors of success are time since vasectomy and age of female partner; reversals performed less than 15 years after vasectomy and having a female partner younger than 40 years are favorable predictors.14–16
EVIDENCE SUMMARY
Vasectomy reversal techniques involve reanastomosis of the testicular and prostatic vasal ends (vasovasostomy) or connecting the vas to the epididymis (vasoepididymostomy). Vasovasostomy patency rates have been reported between 75% and 86%; pregnancy rates range from 45% to 70%.17 Vasoepididymostomy, a technique used in the presence of epididymal obstruction, has patency rates between 31% and 92%, and pregnancy rates between 10% and 50%.17 Repeat attempts at microsurgical vasectomy reversal appear less successful than first attempts with patency rates between 75% and 79%, and pregnancy rates between 31% and 43%.18,19
A large retrospective multi-institutional study involving 1,469 men who underwent microsurgical reconstructive techniques showed a linear decline in patency and pregnancy rates as the time since vasectomy increased.18 Intervals of less than three years showed patency and pregnancy rates of 97% and 76%, respectively; intervals between three and eight years, 88% and 53%; intervals between nine and 14 years, 79% and 44%; and intervals of 15 years or longer, 71% and 30%.18 A smaller retrospective series of 213 microsurgical vasectomy reversal procedures (performed by one surgeon) showed similar patency rates regardless of interval; pregnancy rates were statistically lower (44%; P < .05) for intervals greater than 15 years compared with less than 15 years (82% to 89%).14
A more recent retrospective study of 334 patients undergoing vasectomy reversal (performed by one surgeon) showed similar patency and pregnancy rates regardless of interval. In this study, the only independent predictor of postreversal pregnancy was age of the female partner.15 This finding is identical to that of a retrospective series of 294 vasectomy reversals (performed by three surgeons) that demonstrated lower pregnancy rates if the female partner was 40 years or older than if the female partner was younger than 40 years (14% vs. 56%).16 Presence of sperm granuloma, one-layer vs. two-layer microsurgical vasovasostomy, and type of anesthesia used appear to have no effect on success rates.14,18
Aside from the variability in success rates, microsurgical vasectomy reversal procedures have significant economic implications. The cost of a successful vasectomy reversal, that is, one that leads to a successful pregnancy carried to delivery, ranges from $16,000 to $30,000. This is mostly an out-of-pocket expense for the individual or couple.20
Which Patients Are Good Candidates for Vasectomy?
Men older than 30 years in a stable, committed relationship appear to be the best candidates for vasectomy.
EVIDENCE SUMMARY
In a retrospective study involving 365 men who underwent vasectomy, patients in their 20s were 12.5 times more likely to request vasectomy reversal compared with men older than 30 years. In the same study, men whose wives worked outside the home were twice as likely to request vasectomy reversal compared with men whose wives stayed at home. Interestingly, men with children appear to request vasectomy reversal more than men without children. Religious affiliation, occupation, or number of marriages had no impact on request for reversal.21 Finally, change in marital status was strongly associated with request for reversal.22
Data Sources: A PubMed search was completed in Clinical Queries using the key term vasectomy. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. A search was also performed using Essential Evidence Plus. Search dates: October 2011 and August 2013.