
Am Fam Physician. 2017;95(11):717-724
Patient information: See related handout on hives, written by the author of this article.
Author disclosure: No relevant financial affiliations.
Urticaria commonly presents with intensely pruritic wheals, sometimes with edema of the subcutaneous or interstitial tissue. It has a lifetime prevalence of about 20%. Although often self-limited and benign, it can cause significant discomfort, continue for months to years, and uncommonly represent a serious systemic disease or life-threatening allergic reaction. Urticaria is caused by immunoglobulin E- and non–immunoglobulin E-mediated release of histamine and other inflammatory mediators from mast cells and basophils. Diagnosis is made clinically; anaphylaxis must be ruled out. Chronic urticaria is idiopathic in 80% to 90% of cases. Only a limited nonspecific laboratory workup should be considered unless elements of the history or physical examination suggest specific underlying conditions. The mainstay of treatment is avoidance of triggers, if identified. The first-line pharmacotherapy is second-generation H1 antihistamines, which can be titrated to greater than standard doses. First-generation H1 antihistamines, H2 antihistamines, leukotriene receptor antagonists, high-potency antihistamines, and brief corticosteroid bursts may be used as adjunctive treatment. In refractory chronic urticaria, patients can be referred to subspecialists for additional treatments, such as omalizumab or cyclosporine. More than one-half of patients with chronic urticaria will have resolution or improvement of symptoms within a year.
Urticaria is a common dermatologic condition that typically presents with intensely pruritic, well-circumscribed, raised wheals ranging from several millimeters to several centimeters or larger in size. Urticaria can occur with angioedema, which is localized nonpitting edema of the subcutaneous or interstitial tissue that may be painful and warm. The intense pruritus can cause significant impairment in daily functioning and disrupt sleep.1 Typically otherwise benign and self-limited, urticaria can be a symptom of life-threatening anaphylaxis or, rarely, indicate significant underlying disease.
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| It is important to rule out underlying anaphylaxis in patients presenting with urticaria. | C | 2, 4, 9 | Evaluate vital signs and symptoms involving other organ systems such as pulmonary, cardiovascular, neurologic, or gastrointestinal. |
| An extensive laboratory workup for urticaria is not generally recommended. Additional testing can be performed if the presentation suggests underlying causes requiring confirmation. | C | 2, 4, 9, 16 | Complete blood count with differential, erythrocyte sedimentation rate or C-reactive protein, thyroid-stimulating hormone, urinalysis, and liver function tests can be considered. |
| Second-generation H1 antihistamines are safe and effective symptomatic therapy for urticaria. | A | 2, 4, 9, 19, 20 | Second-generation H1 antihistamines are recommended over older antihistamines because of adverse effect profiles. All H1 antihistamines appear to be effective. |
| If needed to control symptoms of urticaria, second-generation H1 antihistamines can be titrated to two to four times the normal dose. | C | 2, 4, 9 | A higher risk of adverse effects is present with higher doses. Limited effectiveness data are available. |
| A short course of systemic corticosteroids may help control severe cases of urticaria. | C | 2, 4, 9 | Few clinical data support this recommendation, but it is widely practiced. |
| Other medications such as first-generation H1 antihistamines, H2 antihistamines, and leukotriene receptor antagonists may be added to control symptoms of chronic urticaria. | B | 2, 4, 9 | Several studies have produced varying results, but these are generally safe medications with some evidence of benefit. |
| Recommendation | Sponsoring organization |
|---|---|
| Do not routinely do diagnostic testing in patients with chronic urticaria. | American Academy of Allergy, Asthma, and Immunology |
| Do not rely on antihistamines as first-line treatment in severe allergic reactions. | American Academy of Allergy, Asthma, and Immunology |
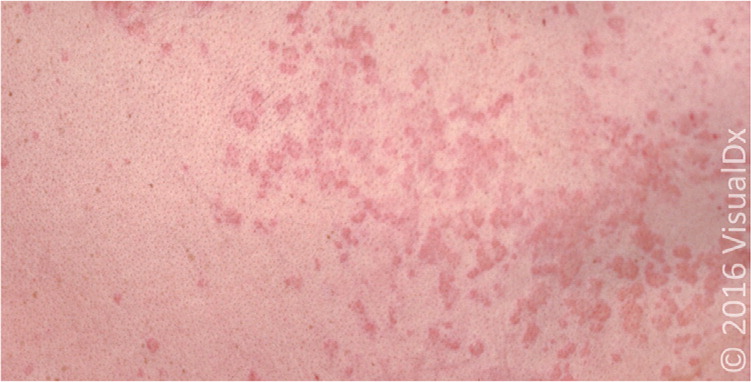
Urticaria can appear on any part of the skin. The wheals can be pale to brightly erythematous in color, often with surrounding erythema. The lesions are round, polymorphic, or serpiginous, and can rapidly grow and coalesce (Figures 1 through 3). Angioedema presents primarily in the face, lips, mouth, upper airway, genitalia, and extremities. The onset of symptoms for urticaria or angioedema is rapid, usually occurring over minutes. Individual urticarial lesions typically resolve in one to 24 hours without treatment, although additional wheals can erupt in new crops. Angioedema may take days to resolve.2


Urticaria, with or without angioedema, can be classified as acute or chronic. Urticaria that recurs within a period of less than six weeks is acute. Recurring chronic urticaria lasts longer than six weeks. Urticaria can present in persons of any age, with a lifetime prevalence of approximately 20%. Chronic urticaria has a lifetime prevalence of approximately 0.5% to 5%.3,4
Etiology
Urticaria and angioedema have similar underlying pathophysiologic mechanisms: histamine and other mediators released from mast cells and basophils. If the release occurs in the dermis, it results in urticaria, whereas if the release occurs in the deeper dermis and subcutaneous tissues, it results in angioedema. Immunoglobulin E (IgE) often mediates this release, but non-IgE and nonimmunologic mast cell activation also can occur. Proteases from aeroallergens and activation of the complement system have been proposed as examples of non-IgE triggers.5 There may be a serologic autoimmune component in a subset of patients with chronic urticaria, including antibodies to IgE and the high-affinity IgE receptor. However, the clinical significance of these autoantibodies is unclear.4,6 Anti-IgE antibodies can also be found in atopic dermatitis and several autoimmune diseases.
There are a number of identified causes of urticaria (Table 1).4,7,8 Common causes include allergens (Figure 4), food pseudoallergens (foods that contain histamine or salicylates, or cause the release of histamine directly), insect envenomation, medications, and infections.2,4,7,9 Infections are the most common cause of urticaria in children.10 The infectious agents commonly associated with urticaria include various viruses (e.g., rhinovirus, rotavirus, Epstein-Barr, hepatitis A, hepatitis B, hepatitis C, herpes simplex, human immunodeficiency virus), bacteria (e.g., urinary tract infections, streptococcus, mycoplasma, Helicobacter pylori), and parasites. Medications, notably beta-lactam antibiotics, typically cause urticaria via allergic reactions, although some medications (e.g., aspirin, nonsteroidal anti-inflammatory drugs [NSAIDs], vancomycin, opiates) can also trigger urticaria through direct mast cell degranulation.
| Immunoglobulin E (IgE) mediated |
| Aeroallergens |
| Contact allergen |
| Food allergens |
| Insect venom |
| Medications |
| Parasitic infections |
| Non-IgE immunologically mediated |
| Aeroallergens (proteases) |
| Autoimmune disease |
| Bacterial infections |
| Cryoglobulinemia |
| Fungal infections |
| Lymphoma |
| Vasculitis |
| Viral infections |
| Nonimmunologically mediated |
| Contact allergen |
| Elevation of core body temperature |
| Food pseudoallergens |
| Light |
| Mastocytosis |
| Medications (direct mast cell degranulation) |
| Physical stimuli (cold, heat, pressure, vibration) |
| Water |

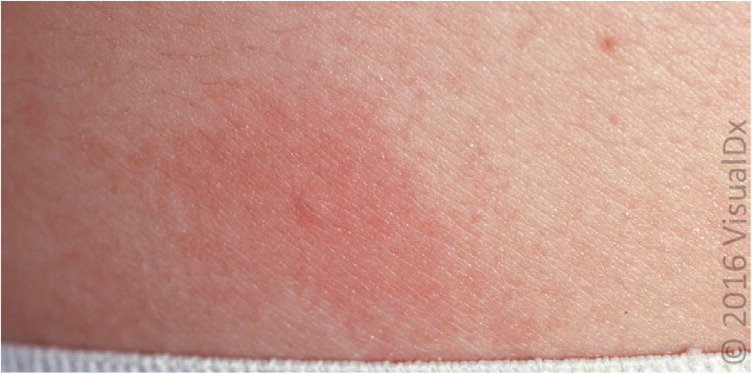
In some patients, physical stimuli, including pressure, cold (Figure 5), heat, and the raising of the core body temperature (cholinergic urticaria; Figure 6), cause urticaria that tends to be chronic.11 Systemic disease is an uncommon cause of urticaria. Illnesses that have been associated with urticaria or angioedema include Hashimoto thyroiditis, mastocytosis, systemic lupus erythematosus, Sjögren syndrome, rheumatoid arthritis, vasculitis (Figures 7 and 8), celiac disease, and lymphoma.12 Causes of acute urticaria often can be identified during the patient history, although 80% to 90% of chronic urticaria cases are idiopathic.4,13



Evaluation
The diagnosis of urticaria is usually clinical. The first step in evaluating urticaria and angioedema is a history and physical examination to characterize the lesions and help identify causes. History elements that should be elicited include onset, timing (e.g., with the menstrual cycle, if an association is suspected), location, and severity of symptoms; associated symptoms, which may suggest anaphylaxis; and potential environmental triggers. Other important parts of the history include medication and supplement use, (especially new or recently changed dosages), allergies, recent infections, travel history, family history of urticaria and angioedema, and complete review of systems to identify possible causes and symptoms of systemic illnesses. Sexual history, illicit drug use history, and transfusion history may provide important information about the risk of infectious causes, such as viral hepatitis and human immunodeficiency virus.
The physical examination should include vital signs, identification and characterization of current lesions and their complete extent, testing for dermatographism (i.e., urticaria that appears in the pattern of localized pressure elicited by stroking with the blunt end of a pen or tongue blade), and cardiopulmonary examination to help rule out anaphylaxis and infectious causes. Examination of the eyes, ears, nose, throat, lymph nodes, abdomen, and musculoskeletal system may help identify underlying causes. Table 2 lists clinical clues from the history and physical examination that suggest certain etiologies for urticaria.4,7,8,14,15
| Clinical clue | Possible etiology |
|---|---|
| Abdominal pain, dizziness, hypotension, large erythematous patches, shortness of breath, stridor, tachycardia | Anaphylaxis |
| Dermatographism, physical stimuli | Physical urticaria |
| Food ingestion temporally related to symptoms | Food allergy |
| High-risk sexual behavior or illicit drug use history | Hepatitis B or C (cryoglobulinemia) virus, human immunodeficiency virus |
| Infectious exposure, symptoms of upper respiratory tract or urinary tract infections | Infection |
| Joint pain, uveitis, fever, systemic symptoms | Autoimmune disease |
| Medication use or change | Medication allergy or direct mast cell degranulation |
| Pregnancy | Pruritic urticarial papules and plaques of pregnancy |
| Premenstrual flare-up | Autoimmune progesterone dermatitis |
| Smaller wheals (1 to 3 mm); burning or itching; brought on by heat, exercise, or stress | Cholinergic urticaria |
| Thyromegaly, weight gain, cold intolerance | Hypothyroidism |
| Travel | Parasitic or other infection |
| Weight loss (unintentional), fevers, night sweats | Lymphoma |
| Wheals lasting longer than 24 hours, nonblanching papules, burning or other discomfort, residual hyperpigmentation, fevers, arthralgias | Urticarial vasculitis (Figures 7 and 8) |
It is critical to rule out anaphylaxis, which has findings or symptoms involving other organ systems beyond the skin, such as the pulmonary (wheezing, stridor), cardiovascular (tachycardia, hypotension), gastrointestinal (diarrhea, vomiting, abdominal pain), or nervous system (dizziness).2,4,9 Several dermatologic conditions can be confused with urticaria. Elements of the history and physical examination can help distinguish among these conditions (Table 3).4,7,8,15
| Condition | Distinguishing characteristics |
|---|---|
| Arthropod bites | Lesions lasting several days, insect exposure history |
| Atopic dermatitis | Maculopapular, scaling, characteristic distribution |
| Bullous pemphigoid | Lesions lasting more than 24 hours, blistering, Nikolsky sign (light friction causes erosion or vesicle) |
| Contact dermatitis | Indistinct margins, papular, persistent lesions, epidermal component present |
| Erythema multiforme | Lesions lasting several days, iris-shaped papules, target appearance, may have fever |
| Fixed-drug reactions | Offending drug exposure, not pruritic, often bullous, hyperpigmentation |
| Henoch-Schönlein purpura | Lower extremity distribution, purpuric lesions, systemic symptoms |
| Mastocytoma | Yellow to orange pigmentation, Darier sign (a wheal and flare-up reaction produced by stroking the lesion), flushing, bullae, occurs most commonly in children |
| Mastocytosis, diffuse cutaneous | Normal to yellow-brown skin color, diffuse thickening, bullae |
| Morbilliform drug reactions | Maculopapular, associated with medication use |
| Pityriasis rosea | Lesions lasting weeks, herald patch, Christmas tree pattern, often not pruritic |
| Urticaria pigmentosa | Smaller lesions (1 to 3 mm), orange to brown pigmentation, Darier sign (a wheal and flare-up reaction produced by stroking the lesion) |
| Viral exanthem | Not pruritic, prodrome, fever, maculopapular lesions, individual lesions lasting days |
Laboratory workup in the absence of indications of an underlying cause is not necessary.4,16 If the history or physical examination suggests a specific cause or underlying disease, targeted testing is appropriate.2,4,9,16 For example, presentation that suggests urticarial vasculitis should prompt a skin biopsy, whereas if the history suggests an allergic trigger, allergy testing may be useful after resolution of symptoms. With chronic urticaria, or in acute cases if there are patient or parental concerns, a limited nonspecific workup including a complete blood count with differential, erythrocyte sedimentation rate and/or C-reactive protein testing, liver enzymes, and thyroid-stimulating hormone measurement can be considered to rule out underlying causes. When the history suggests a physical urticaria, challenge testing with standardized physical stimuli can confirm the diagnosis.11,17 Allergy testing is not recommended unless there is specific indication of an allergic cause.4
General Principles of Treatment
Methods of treatment for urticaria are the same for adults and children. The mainstay of treatment is avoidance of identified triggers. It is also recommended that patients avoid using aspirin, alcohol, and NSAIDs, as well as avoid wearing tight clothing, because these may worsen symptoms. If trigger avoidance is impossible, no trigger is identified, or symptom relief is needed despite trigger avoidance, H1-antihistamines are first-line pharmacotherapy. Second-generation H1 antihistamines such as loratadine (Claritin), desloratadine (Clarinex), fexofenadine (Allegra), cetirizine (Zyrtec), and levocetirizine (Xyzal) are relatively nonsedating at standard dosages and are dosed once per day.
First-generation H1 antihistamines, such as diphenhydramine (Benadryl), hydroxyzine, chlorpheniramine, and cyproheptadine, are faster acting and, in some cases, have parenteral forms. However, they require more frequent dosing and have more adverse effects, including sedation, confusion, dizziness, impaired concentration, and decreased psychomotor performance. Because of anticholinergic adverse effects, first-generation H1 antihistamines should be used with caution in older patients. Individual responses to a given antihistamine vary, and there is no strong evidence that a particular antihistamine is superior. Potential adverse effects should be discussed with patients before initiating therapy.
TREATMENT OF ACUTE URTICARIA AND ANGIOEDEMA
If symptoms are not sufficiently controlled with second-generation H1 antihistamines, H2 antihistamines such as cimetidine (Tagamet), famotidine (Pepcid), and ranitidine (Zantac) may be added.18 In severe cases, corticosteroids such as prednisone or prednisolone (0.5 to 1 mg per kg per day) may be added for three to 10 days to control symptoms.2,4,9,19
If systemic symptoms are suggested, especially when an identified trigger is associated with anaphylaxis (e.g., insect envenomation, certain foods), it may be prudent to prescribe epinephrine autoinjectors in sufficient numbers so that the patient will have one for home, one for work or school, and one for the car, as appropriate. Patients should follow up in two to six weeks to evaluate treatment success and tolerance.
Treatment of acute angioedema is largely the same as treatment for urticaria, although corticosteroids may be more commonly recommended.19 However, angioedema of the larynx and massive angioedema of the tongue are medical emergencies because of the risk of airway obstruction, and they require intramuscular epinephrine and airway management. Patients with angioedema that previously threatened airway compromise should be prescribed epinephrine autoinjectors.
TREATMENT OF CHRONIC URTICARIA
Most of the data on treatment of urticaria involve chronic cases. Current guidelines suggest a stepwise approach to treating chronic idiopathic urticaria2,9 (Figure 94 ). As with acute urticaria, the first step is second-generation H1 antihistamines.2,4,9,20,21 For improved symptom control, the medication should be dosed daily, rather than on an as-needed basis.22 Although there are some differences among published guidelines on the specifics of the subsequent steps,2,4,9 the American Academy of Allergy, Asthma, and Immunology and the American College of Allergy, Asthma, and Immunology recommend that if first-line treatment is insufficient, the second step is implementation of one or more of the following additional strategies: the second-generation H1 antihistamine can be titrated up to two to four times the usual dose23; a different second-generation H1 antihistamine can be added; first-generation H1 antihistamines may be added at nighttime; H2 antihistamines may be added18; and leukotriene receptor antagonists, such as montelukast (Singulair) and zafirlukast (Accolate), can also be added, especially in patients with NSAID intolerance or cold urticaria.24
If symptomatic control is still not achieved, the third step is addition and titration of high-potency antihistamines as tolerated, such as hydroxyzine or the tricyclic antidepressant doxepin (possesses markedly more antihistaminic effect than diphenhydramine). The fourth step is referral to a subspecialist for use of immunomodulatory agents. There are a number of such agents, but the data on the effectiveness in chronic urticaria for most are weak at best.25,26 The two agents with the most robust data are omalizumab (Xolair) and cyclosporine (Sandimmune).2,4,9 For controlling flare-ups in chronic urticaria, a three- to 10-day burst of corticosteroids (prednisone or prednisolone up to 1 mg per kg per day) is sometimes used; long-term use is not recommended because of adverse effects. Potent topical corticosteroids may have a benefit in localized delayed-pressure urticaria.27
Once symptoms are adequately controlled, physicians should consider stepping down treatment sequentially. Empiric elimination diets are not recommended. If an underlying cause of chronic urticaria is identified, the condition should be treated or the patient referred to an appropriate subspecialist.
Prognosis
Acute urticaria is typically self-limited and resolves with proper avoidance of triggers. With chronic urticaria, a prospective cohort study found that 35% of patients are symptom free within one year, with another 29% having some reduction of symptoms. Spontaneous remission occurred within three years in 48% of the cases of idiopathic chronic urticaria, but only 16% of the cases of physical urticaria.28 Another prospective study in children found remission rates at one, three, and five years to be 18%, 54%, and 68%, respectively.29 Patients may experience repeated episodes throughout their lives.
Data Sources: A search was conducted in PubMed Clinical Queries using urticaria with each category and systematic review. Also searched were the Agency for Healthcare Research and Quality Evidence Reports, Cochrane Database of Systematic Reviews (complete reviews), Dynamed, Essential Evidence Plus, Institute for Clinical Systems Improvement, National Guideline Clearinghouse, and UpToDate. Search dates: February to May 2016, and January 2017.
