
A more recent article on chronic rhinosinusitis is available.
Am Fam Physician. 2017;96(8):500-506
Patient information: See related handout on chronic rhinosinusitis, written by the author of this article.
Author disclosure: No relevant financial affiliations.
Chronic rhinosinusitis is an inflammatory disease of the paranasal sinuses that occurs in 1% to 5% of the U.S. population. It may significantly decrease quality of life. Chronic rhinosinusitis is defined by the presence of at least two out of four cardinal symptoms (i.e., facial pain/pressure, hyposmia/anosmia, nasal drainage, and nasal obstruction) for at least 12 consecutive weeks, in addition to objective evidence. Objective evidence of chronic rhinosinusitis may be obtained on physical examination (anterior rhinoscopy, endoscopy) or radiography, preferably from sinus computed tomography. Treatment is directed at enhancing mucociliary clearance, improving sinus drainage/outflow, eradicating local infection and inflammation, and improving access for topical medications. First-line treatment is nasal saline irrigation and intranasal corticosteroid sprays. There may be a role for antibiotics in patients with evidence of an active, superimposed acute sinus infection. If medical management fails, endoscopic sinus surgery may be effective. Patients not responding to first-line medical therapy should be referred to an otolaryngologist, and selected patients with a history suggestive of other comorbidities (e.g., vasculitides, granulomatous diseases, cystic fibrosis, immunodeficiency) may also benefit from referral to an allergist or pulmonologist.
Chronic rhinosinusitis is an inflammatory condition of the paranasal sinuses that most often causes chronic sinonasal symptoms. In the United States, chronic rhinosinusitis has an estimated prevalence of 1% to 5%. It is a readily treatable disease that is responsible for direct and indirect health care expenses totaling billions of dollars every year in the United States.1,2 Because the pathophysiology of chronic rhinosinusitis in children is distinct from that in adults, and the medical and surgical approach differs significantly between children and adults,3 this review focuses on adult chronic rhinosinusitis.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The diagnosis of chronic rhinosinusitis is based on the presence of at least two out of four cardinal symptoms for at least 12 weeks, in addition to objective evidence on physical examination or radiography. | C | 18 |
| Non–contrast-enhanced computed tomography is the imaging study of choice to confirm the diagnosis of chronic rhinosinusitis. | C | 19, 20 |
| Nasal saline irrigations improve sinonasal symptoms in patients with chronic rhinosinusitis. | A | 25–27 |
| Intranasal corticosteroid sprays improve sinonasal symptoms in patients with chronic rhinosinusitis. | A | 33, 35, 36 |
| Short courses (up to three weeks) of oral corticosteroids, alone or as an adjunct to standard maintenance therapy, improve sinonasal symptoms in the short term in patients with chronic rhinosinusitis and polyps. | A | 45, 46 |
| Oral antibiotics, given for up to three weeks, may be considered as a treatment option for acute exacerbations of chronic rhinosinusitis. | C | 31, 32 |
| Recommendation | Sponsoring organization |
|---|---|
| Do not order more than one CT scan of the paranasal sinuses within 90 days to evaluate uncomplicated chronic rhinosinusitis when the paranasal sinus CT obtained is of adequate quality and resolution to be interpreted by the clinician and used for clinical decision making and/or surgical planning. | American Academy of Otolaryngology–Head and Neck Surgery Foundation |
Orbital and intracranial complications are the most serious sequelae of chronic rhinosinusitis but are extremely rare, usually arising in patients with superimposed acute sinusitis. Orbital complications include periorbital cellulitis, orbital cellulitis, and orbital abscess. Intracranial complications include cavernous sinus thrombosis, meningitis, and epidural abscess.4
Chronic rhinosinusitis may also exacerbate comorbid pulmonary diseases. Bacterial flora from the paranasal sinuses of patients with cystic fibrosis, who almost always develop chronic rhinosinusitis, can serve as a reservoir for seeding pulmonary infections.5 In persons with asthma, comorbid chronic rhinosinusitis is associated with poor asthma control, as well as more asthma-related emergency department visits and systemic corticosteroid use.6–8 The greatest impact of chronic rhinosinusitis is decreased quality of life through burdensome chronic sinonasal symptoms and acute exacerbations.9,10
Comorbid Conditions
There is increasing evidence that chronic rhinosinusitis is an inflammatory disease and not an infectious process.11,12 Consistent with its underlying inflammatory etiologies, chronic rhinosinusitis is associated with other inflammatory diseases such as allergic rhinitis and asthma.13–15 Moreover, specific inflammatory and immunodeficiency conditions may rarely cause chronic rhinosinusitis, although symptoms that are not typical of chronic rhinosinusitis may also be present.16 For example, granulomatous diseases such as vasculitis and sarcoidosis can cause chronic rhinosinusitis and nasal symptoms such as nasal crusting and epistaxis. Notably, chronic sinonasal symptoms are the most common presentation of several forms of vasculitis, including granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis.17 Patients with chronic, recurrent sinus infections due to immunodeficiency and poor mucociliary clearance (e.g., cystic fibrosis, primary ciliary dyskinesia) may develop concurrent chronic rhinosinusitis.16
Diagnosis
HISTORY AND PHYSICAL EXAMINATION
Chronic rhinosinusitis is diagnosed clinically with a physical examination and focused sinonasal history, including chronic rhinosinusitis–associated comorbidities and a pertinent family history. Clinical consensus guidelines from the American Academy of Otolaryngology–Head and Neck Surgery define chronic rhinosinusitis as the presence of at least two out of four cardinal symptoms (i.e., facial pain/pressure, hyposmia/anosmia, nasal obstruction, and nasal drainage) for at least 12 consecutive weeks, in addition to objective evidence on physical examination (anterior rhinoscopy or endoscopy) or radiography, such as computed tomography (CT; Table 1).18 Objective evidence of chronic rhinosinusitis was added as a diagnostic criterion because although the presence of symptoms is sensitive for diagnosis of chronic rhinosinusitis, it is not specific.18 Of the four cardinal symptoms used for diagnosis, nasal obstruction is most common (81% to 95% of patients), followed by facial pressure (70% to 85%), discolored nasal drainage (51% to 83%), and hyposmia (61% to 69%).18
|
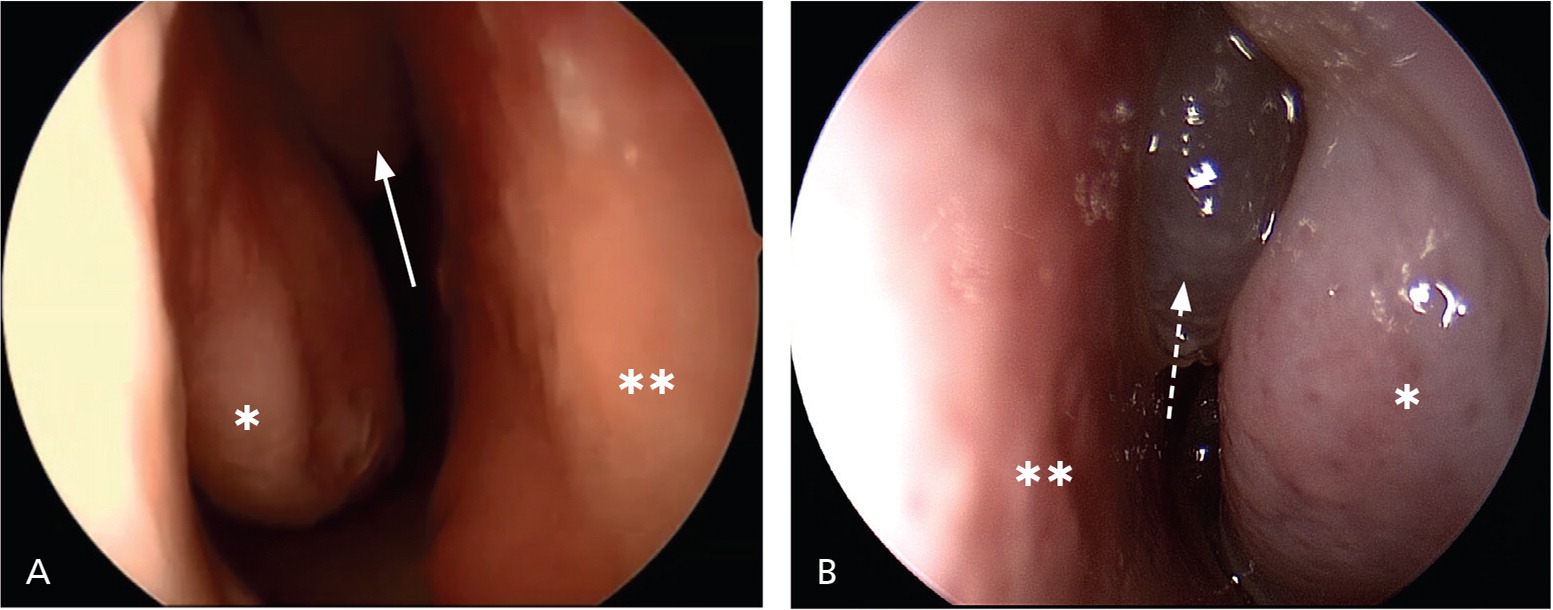
Physical examination is necessary to establish objective evidence of the diagnosis and should include inspection of the nasal cavity using anterior rhinoscopy and nasal endoscopy when available18 (Figure 1A). In the primary care setting, anterior rhinoscopy is easily performed with an otoscope or a nasal speculum and a headlight. The presence of nasal drainage, particularly mucopurulent drainage, should be assessed using anterior rhinoscopy. Patency of the nasal airway should also be evaluated by assessing for septal deviation and inferior or middle turbinate enlargement; polyps (Figure 1B) or other masses should be ruled out.18 When in doubt, patients should be referred to an otolaryngologist for nasal endoscopy. This procedure has the added benefits of magnification, better anatomic assessment of the nasal cavity and structures, and improved visualization of mucopurulence or polyps arising specifically from the paranasal sinuses.
IMAGING
Imaging may also be used to identify objective evidence of chronic rhinosinusitis. Sinus plain film radiography is no longer recommended for evaluation of the paranasal sinuses because of poor accuracy.19,20 Non–contrast-enhanced CT is the imaging study of choice to evaluate the paranasal sinuses in the diagnosis of chronic rhinosinusitis19,20 (Figure 2). Sinus CT is safe—the average radiation from a scan is equivalent to four months of typical background radiation exposure from living on Earth (less than 1 mSv).19,21
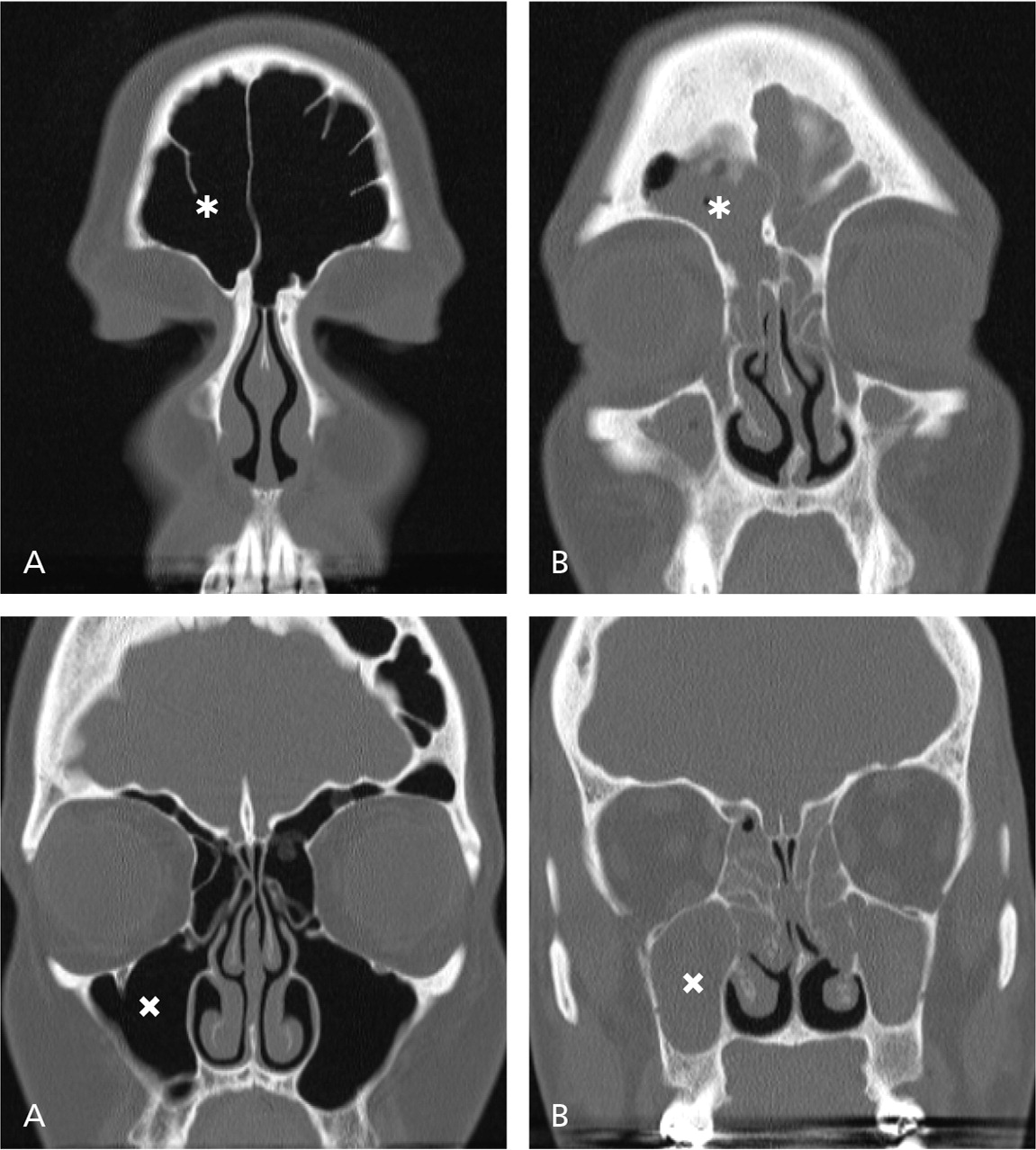
Imaging studies, including sinus CT, should be performed only in patients with at least two subjective criteria for chronic rhinosinusitis because there is a high false-positive rate for the detection of sinonasal abnormalities.22 For example, mucosal thickening within the paranasal sinuses may be a result of a viral upper respiratory infection that may be visible on radiography for weeks.
Sinus CT can be useful in the primary care setting in lieu of endoscopy.19,21 In symptomatic patients, sinus CT can definitively rule out or confirm chronic rhinosinusitis, allowing for prompt treatment. Additionally, economic modeling has suggested that up-front sinus CT ordered by primary care physicians is cost-effective by providing timely management and referral.23,24 If the patient is referred to an otolaryngologist for surgical intervention, repeat imaging can be avoided with a few simple ordering specifications that are consistent with image guidance systems commonly used by otolaryngologists (Table 2).
| Obtain scans axially with no (zero-degree) gantry tilt |
| Include all of the forehead and extend to the maxillary teeth, also including the ears and tip of the nose |
| Maintain a maximum slice thickness of 1 mm |
| Get contiguous, nonoverlapping slices |
| Save in an uncompressed DICOM format |
SPECIAL DIAGNOSTIC CONSIDERATIONS
Unilateral symptoms or physical examination findings, including nasal drainage, polypoid nasal masses, or facial pain, should prompt consideration of etiologies other than chronic rhinosinusitis, such as neoplasms.18 Early referral to an otolaryngologist for endoscopic evaluation is beneficial in these patients. Double vision and decreased vision, periorbital edema/cellulitis, ophthalmoplegia, and meningismus suggest orbital or intracranial complications of sinusitis and should prompt immediate workup, evaluation, and treatment.18
Treatment
The goals of treatment in patients with chronic rhinosinusitis are to manage symptoms and improve or maintain quality of life. Treatment is directed at enhancing mucociliary clearance, improving sinus drainage/outflow, eradicating local infection and inflammation, and improving access for topical medications.18 Treatment consists of medical management, and endoscopic sinus surgery if appropriate medical management is unsuccessful.18
Many patients with chronic rhinosinusitis have allergies, asthma, and other less common comorbidities (e.g., vasculitides, granulomatous diseases, cystic fibrosis, immunodeficiency) that directly contribute to chronic rhinosinusitis.18 Odontogenic infections may also contribute to chronic rhinosinusitis. Therefore, patients not responding to first-line medical therapy should be referred to an otolaryngologist, and patients with a history of (or suggestive of) these comorbidities may also benefit from referral to an allergist or pulmonologist.
NASAL SALINE IRRIGATION
Multiple studies have demonstrated that at least daily saline irrigations reduce symptoms and improve quality of life in patients with chronic rhinosinusitis.25–27 Low-pressure, high-volume (240 mL) saline irrigation may significantly reduce sinonasal symptoms in 50% of patients (number needed to treat = 2) and is superior to nasal saline spray in reducing sinonasal symptoms (absolute risk reduction = 0.2; number needed to treat = 5).25–27
Although isotonic and hypertonic saline irrigations were shown to be equally effective in randomized controlled trials (RCTs),28,29 at least one study showed that hypertonic saline irrigations led to greater burning or patient discomfort.30 Currently, isotonic saline irrigations are recommended as a component of standard medical therapy for chronic rhinosinusitis.31,32 Saline irrigations are ideally used in combination with an intranasal corticosteroid spray, based on small unblinded studies and the low adverse effect profile of saline,26,27 as well as expert opinion on complementary dominant mechanisms of action for saline and corticosteroids (improving mucociliary clearance vs. anti-inflammatory effects, respectively).31,32
TOPICAL INTRANASAL CORTICOSTEROIDS
Many RCTs have demonstrated that intranasal corticosteroid sprays improve sinonasal symptoms and endoscopic findings in chronic rhinosinusitis.32 There is no evidence to suggest that any spray is superior or that increased dosing provides greater effectiveness.33 Intranasal corticosteroid sprays should be used by bending the head forward to look at the floor and spraying laterally (away from the nasal septum). The patient should not sniff too hard after spraying.18
Nonstandard mechanisms for topical delivery of intranasal steroids, most commonly corticosteroid nasal irrigations, have been developed to improve sinus penetration, which is reportedly poor with sprays.34 Although these nonstandard mechanisms are used in subspecialty practices, there are no clinical trials to support their off-label use, and full adverse effect profiles are yet to be determined.
ANTIBIOTICS
The role of antibiotics for treatment of chronic rhinosinusitis is unclear, and there is scant evidence to support their use.37,38 Antibiotic therapy for chronic rhinosinusitis can be short-term (up to three weeks) and long-term. In patients with chronic rhinosinusitis and evidence of an infection (e.g., mucopurulent drainage on endoscopy), expert opinion suggests short-term antibiotic therapy guided by endoscopic culture of fluid obtained via nasal endoscopy.37,38
Long-term use of macrolide antibiotics, which are known to have anti-inflammatory properties, to treat chronic rhinosinusitis has been reported.39,40 However, a recent Cochrane review of five RCTs with 293 patients found little evidence to support the benefit of long-term antibiotics in the treatment of chronic rhinosinusitis and concluded that higher-quality studies are needed.37 Additionally, the possibility of adverse events, such as Clostridium difficile colitis, must also be considered.
ORAL CORTICOSTEROIDS
Multiple RCTs have shown that short courses (up to three weeks) of oral corticosteroids, alone or as an adjunct to standard maintenance therapy, improve sinonasal symptoms and endoscopic findings in the short term for patients with polyps.41–44 Two Cochrane reviews showed no long-term benefit for short courses of oral corticosteroids but reported short-term improvement in sinonasal symptoms and quality of life in patients with chronic rhinosinusitis and nasal polyps.45,46 Thus, oral corticosteroids are an option for short-term improvement of severe symptoms in patients with polyps already on maintenance therapy (nasal saline irrigation and intranasal corticosteroid spray).
Oral corticosteroids should be used only after weighing the possible benefits and harms of therapy.32 Adverse effects of oral corticosteroid use, including avascular necrosis, should be discussed with patients before prescribing.
SURGICAL MANAGEMENT
Endoscopic sinus surgery is an effective treatment of chronic rhinosinusitis when appropriate medical therapy is ineffective. The goals of endoscopic sinus surgery in the treatment of chronic rhinosinusitis are to provide ventilation and drainage of the paranasal sinuses and to enlarge the paranasal sinuses to create greater access for topical medications.32 Although there are no RCTs on surgery for chronic rhinosinusitis, one multicenter prospective cohort study showed that endoscopic sinus surgery leads to greater improvement of sinonasal symptoms and endoscopic findings than continued medical therapy in patients with refractory chronic rhinosinusitis.47 It is important to note that although endoscopic sinus surgery improves symptoms and quality of life, it does not cure the condition, and patients will require medical therapy postoperatively to maintain these improvements.
ACUTE EXACERBATIONS
Like asthma, the natural history of chronic rhinosinusitis includes acute exacerbations.18 Unlike asthma, there is no consensus about what represents an acute exacerbation. Instead, the diagnosis of chronic rhinosinusitis exacerbations is patient-driven and often described in the literature as, for example, sudden worsening of symptoms with return to baseline after treatment.31
Expert opinion suggests that acute exacerbations of chronic rhinosinusitis may be treated using observation, antibiotics, and/or a tapered course of corticosteroids.31 The only RCT of the treatment of chronic rhinosinusitis exacerbations found no evidence of improved sinonasal symptoms after two weeks of antibiotic use compared with placebo.48 This is analogous to an RCT of antibiotics for acute rhinosinusitis, which showed that although antibiotic therapy accelerated the resolution of symptoms, the antibiotic and placebo groups had the same degree of improvement after 10 days.49 Antibiotics and/or oral corticosteroids may therefore accelerate the resolution of chronic rhinosinusitis exacerbations, but it is unclear if they have any other benefit over observation alone.
Data Sources: PubMed and the Cochrane Database of Systematic Reviews were searched for cohort studies, RCTs, meta-analyses, systematic reviews, and clinical consensus guideline statements. Search terms included chronic rhinosinusitis, corticosteroids, antibiotics, treatment, and endoscopic sinus surgery. For additional primary literature sources, we also searched Essential Evidence Plus and references of consensus guidelines and practice parameters published between 2012 and 2016 by the American Academy of Otolaryngology–Head and Neck Surgery, the American Rhinologic Society, and the European Rhinologic Society. Search dates: October to December 2016.
