
Am Fam Physician. 2019;99(7):426-434
Related Practice Guideline: Mild TBI in Children: Guidance from the CDC for Diagnosis and Treatment
Author disclosure: No relevant financial affiliations.
Mild traumatic brain injury, also known as concussion, is common in adults and youth and is a major health concern. Concussion is caused by direct or indirect external trauma to the head resulting in shear stress to brain tissue from rotational or angular forces. Concussion can affect a variety of clinical domains: physical, cognitive, and emotional or behavioral. Signs and symptoms are nonspecific; therefore, a temporal relationship between an appropriate mechanism of injury and symptom onset must be determined. Headache is the most common symptom. Initial evaluation involves eliminating concern for cervical spine injury and more serious traumatic brain injury before diagnosis is established. Tools to aid diagnosis and monitor recovery include symptom checklists, neuropsychological tests, postural stability tests, and sideline assessment tools. If concussion is suspected in an athlete, the athlete should not return to play until medically cleared. Brief cognitive and physical rest are key components of initial management. Initial management also involves patient education and reassurance and symptom management. Individuals recover from concussion differently; therefore, rigid guidelines have been abandoned in favor of an individualized approach. As symptoms resolve, patients may gradually return to activity as tolerated. Those with risk factors, such as more severe symptoms immediately after injury, may require longer recovery periods. There is limited research in the younger population; however, given concern for potential consequences of injury to the developing brain, a more conservative approach to management is warranted.
Mild traumatic brain injury, also known as concussion, accounts for 80% to 90% of traumatic brain injuries and is recognized as a major national health concern.1–7 Whereas 2.8 million traumatic brain injuries were reported in 2013,8 estimates suggest up to 3.8 million occur annually.4,7,9 Concussion diagnosis and management can be challenging, complicated by the lack of a universal definition.2,6,10 No single objective measure or combination of measures for diagnosis and no definitive evidence-based treatments exist. Return-to-activity and return-to-play decisions are limited by a shortage of prospective data.6 Physicians must rely on expert guidelines and available assessment tools with clinical judgment for diagnosis and treatment.2,5,6
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Athletes should not return to play until symptoms of concussion are completely resolved and they are cleared by a health care professional. | C | 2, 4–6, 13, 33 |
| Imaging should be used only to eliminate concerns of more significant injuries and not for evaluation of uncomplicated concussion. | C | 2, 4–7, 10, 12, 13 |
| Early patient education and reassurance are a cornerstone of concussion management. | C | 5, 10, 12 |
| Initial management of concussion includes brief cognitive and physical rest. The degree and duration of rest are not well defined, but most guidelines recommend at least 24 to 48 hours. | C | 2, 5, 6, 12, 27, 28 |
| No medications are available specifically for concussion. Treatment focuses on symptom management with the same medications used in patients without a concussion. | C | 6, 7, 10, 12 |
| An individualized approach to the gradual return to activity after concussion is favored over rigid guidelines, and most algorithms allow for patients to progress at various rates. | C | 2, 5, 6, 10, 12–13 |
| After an initial brief rest period, individuals with concussion should be encouraged to gradually return to normal daily routines, such as school, work, and leisure activities, as tolerated. | C | 6, 10, 12, 14, 30–33 |
| A more conservative approach, including waiting longer for return to activity/return to play and more frequent follow-up, is recommended for children and adolescents with concussions. | C | 4, 5, 7, 13, 28 |
| Children and adolescents should not return to play in sport until they have successfully tolerated returning to school. | C | 5, 6 |
| Protective gear should be worn to prevent overall head and dental injuries, but this has not been clearly shown to reduce the incidence of concussion in most sports. | C | 4–7 |
| Recommendations | Sponsoring organization |
|---|---|
| Computed tomography scans are not necessary in the evaluation of minor head injuries. | American Academy of Pediatrics |
| Do not routinely perform computed tomography in children with minor head injuries. | American Association of Neurologic Surgeons and Congress of Neurologic Surgeons |
Definition, Signs, and Symptoms
Whereas no universal diagnostic criteria for concussion exist, there are commonalities across definitions. The most recent and commonly cited definition,6,11 although primarily derived from research in the sports world, applies to all mechanisms of injury (Table 16). Briefly, a concussion is a brain injury caused by a direct or indirect external mechanism with a clear temporal link to onset of symptoms.2,12 However, other medical conditions (e.g., heat illness, exertional migraines), including preexisting conditions, cause similar symptoms as concussion and must be excluded.2,5,6,10,12,13
| Sports-related concussion is a traumatic brain injury induced by biomechanical forces. | |
| Several common features help to clinically define the nature of a sports-related concussion: | |
| Direct blow to the head, face, neck, or elsewhere on the body with an impulsive force transmitted to the head | |
| Rapid onset of short-lived impairment of neurologic function that resolves spontaneously; however, signs and symptoms sometimes evolve over minutes to hours | |
| Neuropathologic changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury; no abnormality is visible on standard structural neuroimaging studies | |
| Range of clinical signs and symptoms that may involve loss of consciousness; resolution of the clinical and cognitive features typically follows a sequential course; however, in some cases, symptoms may be prolonged | |
| The clinical signs and symptoms cannot be explained by substance use (i.e., alcohol, illicit drugs, medications), other injuries (e.g., cervical injuries, peripheral vestibular dysfunction), or other comorbidities (e.g., psychological factors, coexisting medical conditions) | |
Concussion affects multiple clinical domains: physical, cognitive, and emotional or behavioral. Common signs and symptoms are listed in Table 2.7 Headache is the most common postconcussion symptom, with a prevalence of 86% to 96%.7,13 Dizziness, balance disturbances, and confusion or disorientation are also common.7,13 Whereas loss of consciousness and amnesia were once considered the hallmarks of concussion, neither is required for diagnosis.2,6
| Affective/emotional | Sleep |
| Anxiety/nervousness*† | Decreased sleep† |
| Clinginess | Difficuty initiating sleep† |
| Depression† | Drowsiness*† |
| Emotional lability | Increased sleep*† |
| Irritability*† | Somatic/physical |
| Personality changes | Blurred vision* |
| Sadness | Convulsions |
| Cognitive | Dizziness/poor balance*‡ |
| Amnesia | Fatigue*† |
| Confusion‡ | Headache*‡ |
| Delayed physical reactions | Light-headedness† |
| Delayed verbal responses | Light sensitivity*† |
| Difficulty concentrating*† | Nausea*‡ |
| Difficulty remembering*† | Noise sensitivity* |
| Disorientation*† | Numbness/tingling |
| Feeling in a fog* | Tinnitus† |
| Feeling slowed down* | Vomiting‡ |
| Feeling stunned | |
| Inability to focus | |
| Loss of consciousness | |
| Slurred speech | |
| Vacant stare |
Pathophysiology and Natural Course
MECHANISM OF INJURY
Falls are the leading cause of concussions in adults and children, followed by being struck by an object or against an object and motor vehicle crashes.8 Estimates suggest that greater than 25% of concussions occur during sporting activities.9 In athletic settings, females are more prone to concussion.4,6 Males are more likely to be injured through player-to-player contact, whereas females are more likely to be injured through contact with the playing surface or equipment.7
PATHOPHYSIOLOGY
Concussion results from rotational and angular forces to the brain.7,13 Shear forces disrupt neural membranes, allowing potassium efflux into the extracellular space, causing increases of calcium and excitatory amino acids, followed by further potassium efflux and subsequent suppression of neuron activity.7,12,13 As sodium-potassium pumps restore balance, a concomitant decrease in cerebral blood flow can result in an energy crisis.7,12,13 Disruptions of autonomic regulation can persist for several weeks, during which time the brain may be vulnerable to further injury.7
RECOVERY
Symptoms of concussion typically present immediately after injury but can be delayed by minutes to hours2,4,6; therefore, serial monitoring should occur after a potential concussion. Symptoms often resolve within 72 hours. Sports-related research reports that most adults (85% to 90%) fully recover within two weeks and children (70% to 80%) within one to three months.5,6,14 Other literature suggests most adults recover within three months, with up to one-third experiencing prolonged symptoms.12
Factors predictive of recovery are poorly defined. Traditional markers (e.g., loss of consciousness, amnesia) do not have a clear association with prolonged recovery.6 The most consistent predictor of prolonged recovery is more severe symptoms immediately following injury.6 Other likely predictors include persistent neurocognitive impairment and history of prior concussion.4 Specific acute symptoms may also predict prolonged recovery: fatigue/fogginess and immediate or early onset of headache, amnesia, disorientation, or mental status changes.4,6
Assessment Tools
None of the numerous assessment tools for diagnosis and management of concussion (eTable A) are exclusively effective.3,4 Combining tools increases sensitivity and specificity.4,6 Although the optimal combination is unknown, multidimensional tools are recommended based on expert consensus.2,4,6 Comparing results of post-injury assessments with those of preinjury baseline testing is often conducted in athletes, although it is not mandatory.6 In younger children, baseline testing is not recommended because of significant variability over time and questionable prognostic value.5
| Tools | Comments |
|---|---|
| Common hospital assessment tools | |
| Acute Concussion Evaluation Acute Concussion Evaluation Care Plan Standardized Assessment of Concussion | Numerous validated tools are available. The Acute Concussion Evaluation was developed by the Centers for Disease Control and Prevention to assist with diagnosis, follow-up planning, and coding. Validated versions are available for the emergency department and physician's office. The Acute Concussion Evaluation Care Plan includes return-to-school and return-to-work versions. The emergency department version of the Standardized Assessment of Concussion is validated for use in adults. |
| Neuropsychological tests | |
Written
| These tests are designed to identify subtle cognitive deficits. Written tests are labor intensive and must be interpreted but provide the most in-depth information, whereas computer-based tests can be administered rapidly and to multiple patients simultaneously but are best used as screening tools. The elements best suited to identify concussion include memory, reaction time, and cognitive processing speed. Results are affected by psychiatric disorders, physical symptoms, preexisting conditions, cultural factors, and motivation/effort. Comparisons to baseline data may be helpful but are not necessary. The tests are not validated, and no data demonstrate that they affect outcomes when used to guide return to play. Baseline data are limited in those younger than 12 years; baseline measurements are not recommended in younger children because of significant variability over time. |
Computer-based
| |
| Postural stability testing | |
| Balance Error Scoring System Modified Balance Error Scoring System Sensory Organization Test Vestibular/Ocular Motor Screening | This testing has low to moderate accuracy (limited sensitivity yet strong specificity) for concussion diagnosis. There are limited data regarding its use in monitoring recovery. The Sensory Organization Test is the most sophisticated test, but it is not portable. The Balance Error Scoring System is inexpensive, portable (requiring only a foam block), and easy to administer on the sideline of a sporting event. The Balance Error Scoring System is embedded and described in the SCAT5. Instability usually lasts three to five days after concussion occurs. The Vestibular/Ocular Motor Screening test integrates vision, balance, and motion using ocular activity evaluation (smooth pursuit, rapid eye motion, convergence, reflex, and motion sensitivity) combined with symptom provocation during testing. It uses simple tools (tape measure, metronome, small handheld target) for rapid administration within five to 10 minutes. |
| Sideline assessment tools | |
| Child SCAT5 SCAT5 Standardized Assessment of Concussion | These use a single, simple tool to assess a variety of domains in the initial concussion assessment; use for monitoring recovery is limited. Standardized Assessment of Concussion can be used immediately after injury to evaluate orientation, memory, concentration, and delayed recall. It is validated as a sideline tool for junior high ages and older. The emergency department version is validated in adults. SCAT5 combines multiple assessment tools: symptom checklist, concentration and memory tasks, Maddocks questions,* the Standardized Assessment of Concussion, the Balance Error Scoring System, and the Glasgow Coma Scale. It is validated for the initial concussion assessment in people 13 years and older. It has questionable utility after three to five days. Child SCAT5 is designed for children five to 12 years of age and incorporates simpler questions and assessments than the SCAT5, as well as a parent co-report; it is not yet validated. The SCAT5 series is widely used and includes the most comprehensive sideline tools available. |
| Symptom checklists | |
| Concussion Resolution Index Concussion Symptom Inventory Graded Symptom Checklist Head Injury Scale McGill Abbreviated Concussion Evaluation Neurobehavioral Symptoms Inventory Postconcussion Symptom Scale Rivermead Postconcussion Questionnaire | These are the most widely used type of concussion assessment tool and are helpful for initial diagnosis and monitoring recovery. They are quick, easy, cost-effective tools with good sensitivity and allow athletes to self-report symptoms. Physicians should be aware when using symptom checklists that symptoms may be delayed, may not be reported, or were already present at baseline. Most checklists were developed through clinical judgment; the Concussion Symptom Inventory is the only empirically derived checklist. The SCAT5 and Acute Concussion Evaluation series have embedded checklists. |
SYMPTOM CHECKLISTS
Symptom checklists are useful for diagnosis and monitoring recovery. Checklists allow individuals to self-report symptoms, and they aid clinical decision-making throughout recovery.2,6 Many self-report checklists with commonalities across measures are available, but none have been identified as the preferred choice.4,6,10
NEUROPSYCHOLOGICAL TESTS
Neuropsychological tests identify cognitive deficits,4 but they are not well validated for concussion.4,7,13 Such tests, however, may assist with return-to-activity or return-to-play decision-making and in evaluating individuals with prolonged symptoms.6 There is no consensus as to which neuropsychological tests are best, but those assessing attention, memory, and reaction time are the most sensitive for postconcussion sequelae.4
POSTURAL STABILITY TESTING
SPORTS SIDELINE ASSESSMENT TOOLS
Sideline tools are designed for use by clinicians and nonlicensed personnel. Common tools include the Standardized Assessment of Concussion and the Sport Concussion Assessment Tool 5 (SCAT5). These tools incorporate several assessment methods into a single instrument. The Standardized Assessment of Concussion is validated for junior high ages and older, with emergency department versions being validated only in adult populations.7 The SCAT5 is intended for athletes 13 years and older.5,6 It is validated for use during the acute injury phase, although it has questionable utility three to five days postinjury.6 However, the incorporated symptom checklist may be useful for monitoring recovery.6 The Child SCAT5 is designed for children five to 12 years of age and incorporates simpler questions and assessments than the SCAT5, as well as a parent co-report, although it is not yet validated.5,6 The tests in the SCAT5 series are widely used and are the most comprehensive sideline assessment tools available.
HOSPITAL ASSESSMENT TOOLS
Numerous tools are validated for clinical use.2 Although a hospital version of the SCAT5 is not available, current versions can be modified for use in a hospital setting.6 The Centers for Disease Control and Prevention developed various versions of the Acute Concussion Evaluation for use in hospital, clinical, and emergency settings.15 The SCAT5 and Acute Concussion Evaluation series are available online (SCAT5: https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097506SCAT5.full.pdf; Child SCAT5: https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097492childscat5.full.pdf; Acute Concussion Evaluation forms for health care professionals: https://www.cdc.gov/headsup/providers/tools.html; and Acute Concussion Evaluation Care Plan for patients: https://www.cdc.gov/headsup/providers/discharge-materials.html).
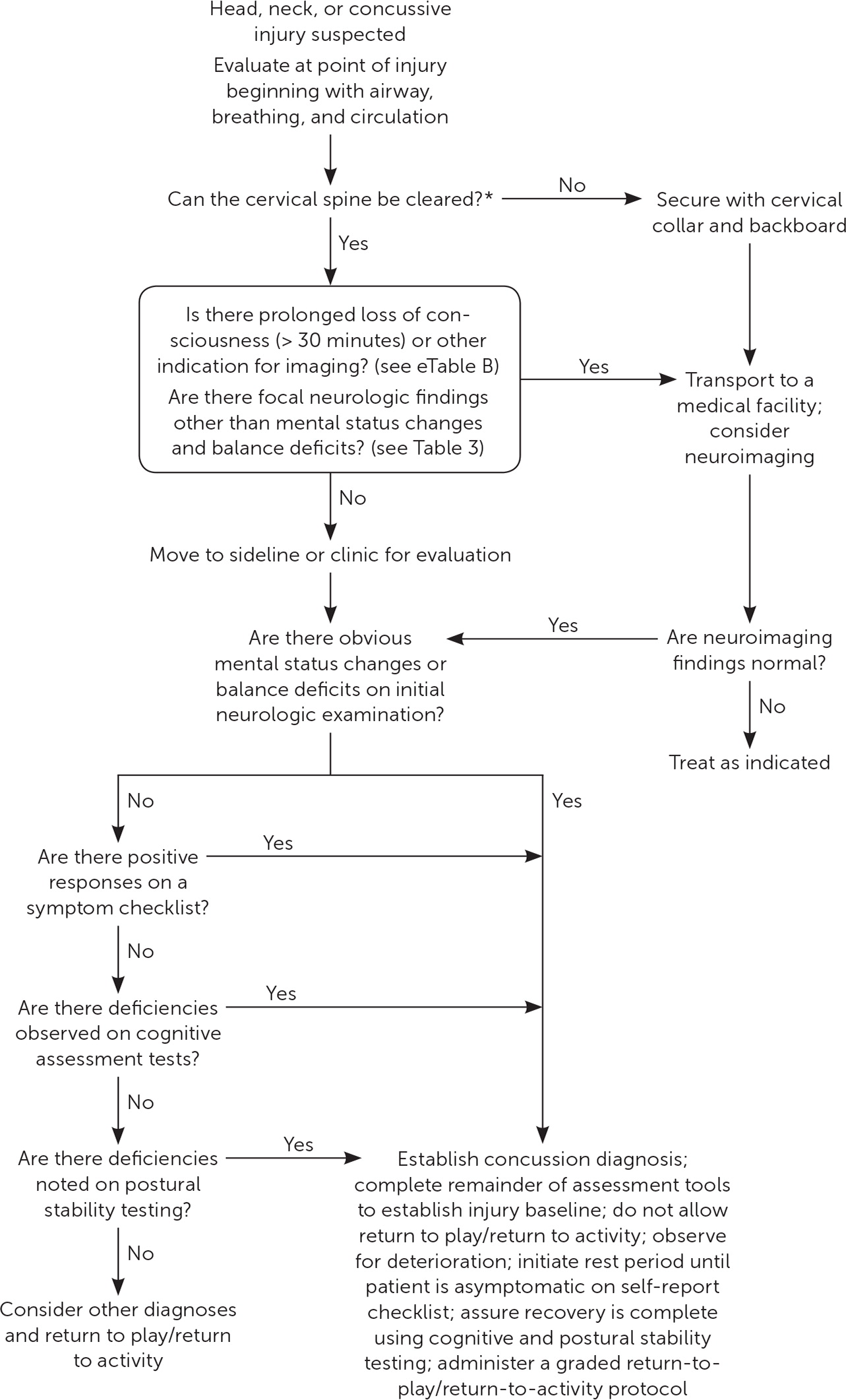
Initial Evaluation
Figure 1 is a suggested algorithm for the initial evaluation of concussion.7 For obvious head injuries, assessment begins at the time of injury to evaluate the cervical spine.2,5–7,13 In unconscious individuals, spinal injury must be assumed.7,13 The initial assessment should first determine whether any emergent medical issues that require immediate attention have occurred. Evaluation should also clarify the severity of head injury, with more severe injuries referred for a higher level of care. Signs of more severe injury include loss of consciousness for more than 30 minutes, posttraumatic amnesia for more than 24 hours, and positive neuroimaging findings (Table 37).
| Assessment* | Findings |
|---|---|
| Balance† | Positive Romberg sign, postural instability, unsteadiness |
| Cranial nerves | Difficulties with vision, unequal or fixed dilated pupils, abnormal extraocular movements, or other abnormal cranial nerve findings may be suggestive of brainstem lesion |
| Deep tendon reflexes | Hyperreflexia or presence of Babinski reflex suggest an upper motor neuron lesion |
| Finger-to-nose test | Abnormal finding suggests coordination deficit |
| Gait | Ataxic gait may suggest cerebellar dysfunction |
| Mental status‡ | Prolonged loss of consciousness (more than 30 minutes), somnolence or confusion, disorientation or posttraumatic amnesia for more than 24 hours, deficit in language and speech |
| Muscular strength | Weakness or unequal strength, decreased tone; involuntary movements may indicate basal ganglia or cerebellar injury |
| Sensory assessment of dermatomes§ | Numbness or abnormal sensation can be traced to spinal nerve root |
SPORTS SIDELINE EVALUATION
If concussion is suspected, an athlete should be removed from play and immediately evaluated by a qualified clinician.2,4–6,13 After addressing urgent medical concerns, the clinician should assess the patient using a sideline assessment tool.4 Regardless of whether concussion is diagnosed or suspected, the athlete must not return to play before receiving medical clearance.2,4–6,13
HOSPITAL OR CLINIC EVALUATION AND IMAGING
The hospital or clinic evaluation is similar to the sideline evaluation but encompasses a detailed history and neurologic examination.7 With concussion, findings are often subtle, and neurologic findings are typically normal other than mental status and balance deficits.7,13 After emergent needs are addressed, a history of head injuries should be assessed. More conservative care (e.g., waiting longer for return to activity or return to play, earlier and more frequent follow-up) may be needed in individuals who have had multiple head injuries, especially if they occurred within the past year.
Imaging is not indicated for the evaluation of uncomplicated concussion.2,4–7,10,12,13 Imaging is important in excluding moderate or severe traumatic brain injuries, skull fractures, and spinal injuries but contributes little to the management of concussion because it is a functional rather than structural injury.6,10 Computed tomography (CT) is the modality of choice.2,10 Although magnetic resonance imaging (MRI) may acutely identify cerebral contusions, MRI is more appropriate for evaluation of prolonged deficits.2 Plain radiography of the head has no role in the evaluation.7,10,14
The most commonly used imaging guidelines for patients 16 years and older with mild head injury include the Canadian CT Head Rule16 and the New Orleans Criteria.17 Both guidelines are sensitive, but the Canadian CT Head Rule has higher specificity.18–21 The Pediatric Emergency Care Applied Research Network (PECARN) pediatric head injury/trauma algorithm is validated for use in all children and adolescents through 18 years of age.5,14,22,23 The Canadian CT Head Rule and PECARN algorithm are provided in eTable B. Free calculators are available at https://www.mdcalc.com/canadian-ct-head-injury-trauma-rule and https://www.mdcalc.com/pecarn-pediatric-head-injury-trauma-algorithm. Newer imaging modalities (e.g., functional MRI) are limited to research and do not yet have clinical application.6
| Canadian CT Head Rule (online calculator: https://www.mdcalc.com/canadian-ct-head-injury-trauma-rule) | |
| For use in patients 16 years and older | |
| Inclusion criteria: mild head injury defined as a Glasgow Coma Scale score of 13 to 15 after witnessed loss of consciousness, amnesia, or disorientation | |
| Exclusion criteria: age younger than 16 years, use of anticoagulants or bleeding disorders, or seizures after injury | |
| CT is required for any one of the following: | |
| High risk of needing neurosurgical intervention (Glasgow Coma Scale score < 15 two hours after injury, suspected open or depressed skull fracture, any sign of basilar skull fracture,* two or more episodes of vomiting, or age 65 years or older) | |
| Medium risk of brain injury detection by CT (retrograde amnesia that occurs 30 minutes or more before impact or dangerous mechanism of injury†) | |
Adapted with permission from Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1394, with additional information from Żyluk A. Indications for CT scanning in minor head injuries: a review. Neurol Neurochir Pol. 2015;49(1):52–57. | |
BIOMARKERS AND ASSESSMENT DEVICES
Several assessment devices to help guide decisions about obtaining a CT scan (e.g., Banyon Brain Trauma Indicator,24 Brainscope,25 Infrascanner26; eTable B) have recently received approval from the U.S. Food and Drug Administration. Whereas popular media often portray these assessments as tests for concussion, they actually function as indicators of possible acute intracranial lesions. The clinical utility of such devices is yet to be determined.
Management
INITIAL MANAGEMENT
Management of concussion is summarized in Table 4.1–7,10,13,14 Once medically stable, the patient may be released to home care provided that the patient has a responsible caretaker and access to medical care.7 Patient education, reassurance, and written instructions of when and how to seek medical attention are required at discharge. Education regarding basic facts of concussion, in written form and reinforced verbally, and reassurance that complete recovery is expected are among the most important aspects of concussion care.5,10,12,14
| Element | Comments | |
|---|---|---|
| Education and reassurance | Early education and reassurance are a cornerstone of treatment and should be provided at initial and follow-up encounters. | |
| Concussion education should be in written form and reinforced verbally; patients should be reassured that most people with concussion fully recover. | ||
| Cognitive rest (duration: 24 to 48 hours) | Activities that require attention or concentration (e.g., text messaging, video games, television, computer use, schoolwork) or that provoke symptoms should be limited. | |
| Physical rest (duration: 24 to 48 hours) | Patients should avoid any physical activity that exacerbates symptoms (e.g., aerobic exercise, lifting weights, household chores, sexual activity). | |
| During the rest period, severe or worsening headache, persistent emesis, or seizures may suggest a need for neuroimaging. | ||
| Medications and interventions | Sunglasses can be used for photophobia, and earplugs or noise-canceling headphones can be used for phonophobia; medications can be used to alleviate other specific symptoms (e.g., nonsteroidal anti-inflammatory drugs or amitriptyline for headaches, sleep aids, anxiolytics). | |
| No pharmacologic therapies are available specifically for concussion; therefore, medications for symptom management should be used as in patients without concussion. | ||
| Avoid acute use of nonsteroidal anti-inflammatory drugs if there is potential for intracranial bleeding. | ||
| When making return-to-activity decisions, be aware that medications may mask postconcussive symptoms. | ||
| Transition back to school | Alert school personnel to the injury and encourage forgiveness of missed assignments. | |
| Reintegration should be slow and allow for scheduled breaks and additional rest periods as needed. | ||
| Assignments should be reduced, with more time given for completing assignments and tests. | ||
| Distraction-free work areas and a notetaker should be provided. | ||
| Standardized tests should not be administered during recovery. | ||
| Transition back to school usually can be completed with informal accommodations; however, a formal individualized education plan or 504 plan is sometimes needed. | ||
| Monitor the patient carefully for two to three months after concussion to assess for academic difficulties. | ||
| Gradual return to activity and return to play | Start with 24 to 48 hours of rest and add the following activities in progressive steps: | |
| Routine daily activities that do not provoke symptoms | ||
| Light routine activity or light nonimpact aerobic exercise | ||
| Light activity specific to occupation or academics; light sport-specific exercise | ||
| Moderate activity; sport-specific noncontact training drills | ||
| Intensive activity; full-contact practice | ||
| Unrestricted activity and return to play | ||
| Each step should be given 24 hours; progression to the next step should occur only if symptoms are not evoked. If any symptoms develop, the patient should immediately stop the activity and return to rest until symptoms resolve. | ||
| The protocol may resume 24 hours after symptoms resolve at the last step in which the patient was asymptomatic. | ||
| Assessing risk of prolonged recovery | Factors that may predict prolonged recovery or warrant caution for return to activity and return to play: | |
| Persistent neurocognitive impairments observed with objective testing | ||
| More severe symptoms immediately following injury | ||
| Prolonged headache | ||
| Fatigue/fogginess | ||
| Early or immediate onset of headache, amnesia, mental status changes, or disorientation after injury | ||
| History of prior concussion | ||
| Being a teenager | ||
| Comorbid conditions | ||
| Use of medications such as psychotropic drugs or anticoagulants | ||
| Aggressive style of play (for athletes, especially in contact sports) | ||
| High-risk sport (involves contact or collision) | ||
| Consider using a multidisciplinary approach: referral to physician experienced in concussion management and for formal neuropsychiatric testing; interaction with employers, teachers, coaches, and training staff. | ||
Initial management after concussion includes a brief period of rest, followed by gradual return to activity. The ideal amount or duration of rest is supported only by limited data, but most guidelines suggest at least 24 to 48 hours.2,5,6,12,27,28 Extended cognitive and physical rest were once the cornerstone of initial management; however, this approach is impractical and may lead to prolonged symptoms and feelings of anxiety and isolation.5,12 A recent study demonstrated that five days of strict rest provided no benefit over 24 to 48 hours of rest and was associated with an increase in reported symptoms.29
No pharmacologic therapies are specifically available for concussion; therefore, medications for symptom management should be used as in patients without concussion.6,7,10,12,13 Nonsteroidal anti-inflammatory drugs are commonly avoided in the first 72 hours after a concussion because of a theoretical risk of bleeding7; however, this concern has not been substantiated. Medications that mask worsening symptoms, such as high-dose analgesics, or that interfere with interpretation of mental status changes, such as sedatives, should be avoided.7
GRADED RETURN TO ACTIVITY
An individualized approach to return to activity is favored over rigid guidelines, and most algorithms allow for patients to progress at various rates.2,5,6,13 After an initial rest period of at least 24 to 48 hours, patients should be encouraged to gradually return to their normal daily routines, such as school, work, and leisure activities, as tolerated.6,10,12,14,30–33 Recent evidence suggests that gradual increase of activities that do not trigger symptoms is safe and may expedite recovery.6,12 Patients may return to unrestricted activities once they have fully recovered and are no longer taking medications that may mask symptoms.6
PROLONGED SYMPTOMS
A multidisciplinary approach should be considered for those with prolonged symptoms, including referral to a physician experienced in concussion management and for formal neuropsychiatric testing. Interaction with employers, teachers, or coaches may be necessary to ensure appropriate accommodations.
Special Considerations
CHILDREN AND ADOLESCENTS
Most concussion research applies to those 13 years and older; few assessment tools have been validated in children younger than 13 years.5,6 Data suggest that teenagers are at greater risk of prolonged recovery.5,6,14 Other risk factors for persistent symptoms include prior concussion, premorbid concussion-like symptoms, psychological or neurologic disorders, learning disabilities, Hispanic ethnicity, and lower socioeconomic status.14 Those presenting with severe or numerous symptoms after concussion may also experience persistent symptoms.6,14 Children and adolescents with these risk factors should be monitored closely 14; however, given concern for potential consequences of injury to the developing brain, conservative management is recommended in all children and adolescents.4,5,7,13,28 Recommendations for return to activity or return to play are similar to those for adults; however, guidelines recommend waiting until the child or adolescent has successfully tolerated returning to school before resuming full activity or play.5,6
MULTIPLE CONCUSSIONS
There is conflicting evidence regarding the long-term effects of multiple or repetitive concussions.6 It is established that those with previous concussions have increased vulnerability to recurrent injury and typically experience longer recovery periods.4–6,13 No specific guidelines exist regarding athletic disqualification or retirement because of recurrent concussions; however, more conservative management is recommended for those with recurrent concussions or increased sensitivity to impact.7
Prevention
The use of protective gear for preventing concussions is supported by limited evidence. Helmets and mouth guards reduce the risk of overall head and dental injuries, but neither has demonstrated a clear reduction in concussion incidence in most sports.4–7 There is evidence that changing rules in some sports, such as restricting body checking in youth hockey, may reduce concussions.4,6 Preventive education, such as the Centers for Disease Control and Prevention's Heads Up campaign (http://www.cdc.gov/HeadsUp), may enhance adherence to safety rules in sports, discourage overly aggressive playing styles, and allow for early recognition of symptoms.5 In 2009, the state of Washington enacted the Zackery Lystedt Law requiring concussion education for coaches, athletes, and parents and mandating removal of athletes from activity following suspected concussion, with clearance by a licensed clinician required to return to play. All 50 states now have similar legislation.9,13,33
Data Sources: A preliminary review was performed using Essential Evidence Plus. A PubMed search was completed in Clinical Queries using the key terms consensus statement concussion, consensus statement mild TBI, clinical practice guidelines concussion, clinical recommendations concussion, clinical recommendations mild TBI, diagnosis of concussion, diagnosis of mild TBI, evaluation of concussion, evaluation of mild TBI, management of concussion, management of mild TBI, treatment of concussion, and treatment of mild TBI. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Cochrane database, Clinical Evidence, National Guideline Clearinghouse, Agency for Healthcare Research and Quality Evidence Reports, and UpToDate. Search dates: November 13, 2017; March 26, 2018; and February 12, 2019.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army Service at large.
