
Am Fam Physician. 2020;101(10):590-598
Author disclosure: Dr. Bhardwaj does not have a formal relationship with any pharmaceutical company to disclose. The author and a public database revealed a food and beverage listing for crisaborole, but this was not a direct payment. Dr. Frazier has no financial affiliations to disclose.
Atopic dermatitis (atopic eczema) is a chronic relapsing and remitting inflammatory skin disease affecting one in 10 people in their lifetime. Atopic dermatitis is caused by a complex interaction of immune dysregulation, epidermal gene mutations, and environmental factors that disrupts the epidermis causing intensely pruritic skin lesions. Repeated scratching triggers a self-perpetuating itch-scratch cycle, which can have a significant impact on the patient's quality of life. The American Academy of Dermatology has created simple diagnostic criteria based on symptoms and physical examination findings. Maintenance therapy consists of liberal use of emollients and daily bathing with soap-free cleansers. Use of topical corticosteroids is the first-line treatment for atopic dermatitis flare-ups. Pimecrolimus and tacrolimus are topical calcineurin inhibitors that can be used in conjunction with topical corticosteroids as first-line treatment. Ultraviolet phototherapy is a safe and effective treatment for moderate to severe atopic dermatitis when first-line treatments are not adequate. Antistaphylococcal antibiotics are effective in treating secondary skin infections. Oral antihistamines are not recommended because they do not reduce pruritus. Evidence is lacking to support the use of integrative medicine in the treatment of atopic dermatitis. Newer medications approved by the U.S. Food and Drug Administration, such as crisaborole and dupilumab, are effective in treating atopic dermatitis but are currently cost prohibitive for most patients.
Atopic dermatitis, or atopic eczema, is a chronic relapsing and remitting inflammatory skin disease with a 10% lifetime prevalence.1 The disease is characterized primarily by scaly, pruritic, erythematous lesions located on flexural surfaces. Atopic dermatitis affects up to 12% of children and 7.2% of adults, leading to high health care use.2 Atopic dermatitis typically starts in childhood, with 60% of patients developing atopic dermatitis before one year of age and 90% by five years of age.3 Compared with children who do not have atopic dermatitis, those who have the condition are more likely to develop food and environmental allergies (15% vs. 4%), asthma (25% vs. 12%), and allergic rhinitis (34% vs. 14%).4 Patients with atopic dermatitis are also more likely to develop ear infections (27% vs. 22%), streptococcal pharyngitis (8% vs. 3%), and urinary tract infections (8% vs. 3%).5
| Recommendation | Sponsoring organization |
|---|---|
| Do not use skin prick tests or blood tests such as the radioallergosorbent test for the routine evaluation of eczema. | American Academy of Dermatology |
| Do not use oral antibiotics for treatment of atopic dermatitis unless there is clinical evidence of infection. | American Academy of Dermatology |
| Do not use systemic (oral or injected) corticosteroids as a long-term treatment for atopic dermatitis. | American Academy of Dermatology |
Pathophysiology
The pathogenesis of atopic dermatitis is multifactorial, involving genetic, immunologic, and environmental factors that disrupt the epidermis.6 The two major risk factors consistently implicated in the development of atopic dermatitis are family history of atopy and mutations in the filaggrin (FLG) gene.7 The FLG gene allows for the formation of profilaggrin, which is further broken down into filaggrin monomers. Lack of these monomers compromises the epidermal barrier, allowing allergens, irritants, and bacteria to trigger a hyperimmune response.3 Increased interleukin-4 and interleukin-13 expression further drives the T-helper 2 immune response, leading to skin barrier impairment.8
Clinical Presentation and Differential Diagnosis
Pruritus, the most common and burdensome symptom of atopic dermatitis, is usually associated with erythematous, scaly lesions of varying morphology. Repeated scratching triggers a self-perpetuating itch-scratch cycle, which can have a significant impact on the patient's quality of life.
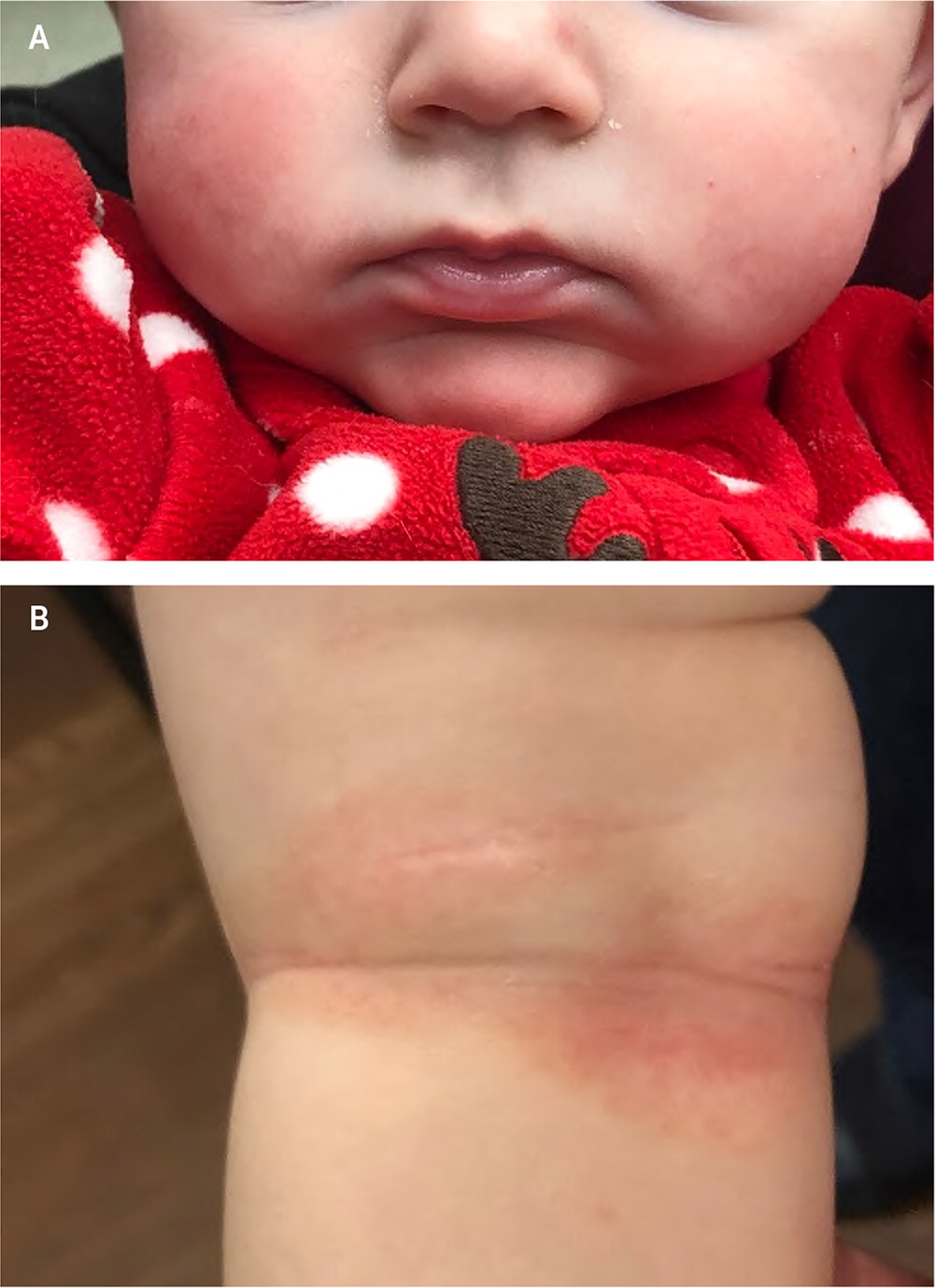
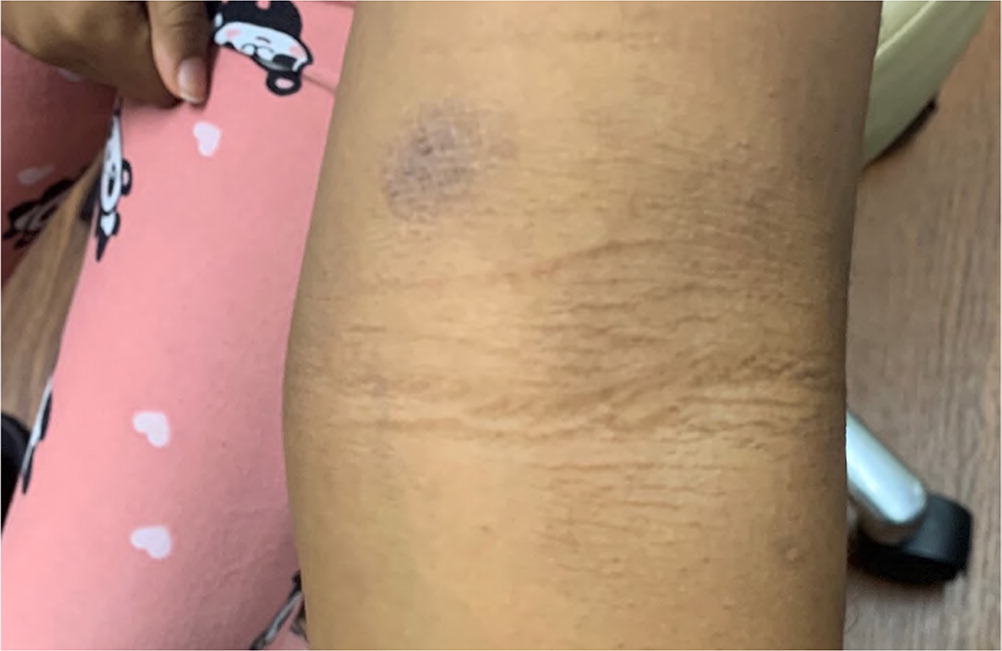
Atopic dermatitis symptomatology and distribution depend on the patient's age at presentation.9 Atopic dermatitis typically presents during the first year of life with erythematous papules, patches, or plaques on the face (especially the cheeks), scalp, trunk, and extremities (Figure 1). Older children typically present with patches on the flexural surfaces (Figure 2). Adults may present with dry, scaly patches on the extremities (Figure 3).

Diagnosis and Classification
Because the presentation of atopic dermatitis is diverse, the differential diagnosis is extensive (Table 1). Atopic dermatitis is a clinical diagnosis with no definitive laboratory test. Approximately 80% of patients with atopic dermatitis are diagnosed and treated in the primary care setting.10 The American Academy of Dermatology (AAD) has streamlined the diagnosis using previously validated diagnostic criteria (Table 2).3 The AAD criteria differentiate essential features that must be present for diagnosis, such as pruritus; important features that support the diagnosis, such as early age at onset; and associated features that suggest the diagnosis but are nonspecific, such as lichenification.
| Diagnosis | Morphology* | Age | Etiology | Other features |
|---|---|---|---|---|
| Contact dermatitis | Erythematous vesicles | Affects all ages | Hypersensitivity reaction | Rash occurs at site of exposure |
| Cutaneous T-cell lymphoma | Erythematous, dry patches | Rare in children | Unknown | Rash develops slowly |
| Dermatitis herpetiformis | Symmetrical vesicles and papules | Rare in children | Autoimmune | Association with gluten sensitivity |
| Impetigo | Honey-colored crusts | Common in children | Bacterial | Very contagious |
| Lichen simplex chronicus | Well-circumscribed, thick scales | Rare in children | Chronic scratching | Association with stress and anxiety |
| Molluscum contagiosum | Flesh-colored papules in clusters | Common in children | Viral | Typically resolves within months |
| Nummular eczema | Annular erythematous patches | Rare in children | Unknown | Patches can last weeks to months |
| Psoriasis | Erythematous patches with silvery scale | Rare in children | Immune-mediated | Can have nail involvement |
| Scabies | Linear erythematous papules | Affects all ages | Parasitic | Intense itching at night |
| Seborrheic dermatitis | Yellow, greasy scales | Affects all ages | Unknown | Scalp and face distribution |
| Tinea corporis | Erythematous, annular patches with raised scaly borders | Common in children | Fungal | Common in body folds |
| Urticaria | Erythematous papules or plaques | Uncommon in children | Immune-mediated | Usually resolves within 24 hours |
| Viral exanthems | Diffuse erythematous macules and papules | Common in children | Viral | Resolves after illness |
| Essential features: must be present for diagnosis Chronic or relapsing history Eczema (acute, subacute, chronic) Pruritus Typical morphology and age-specific patterns* |
| Important features: support the diagnosis (observed in most cases) Atopy (personal or family history) Early age at onset Immunoglobulin E reactivity Xerosis |
| Associated features: suggestive of the diagnosis but nonspecific Atypical vascular responses (facial pallor, white dermographism) Keratosis pilaris, pityriasis alba, hyperlinear palms, or ichthyosis Ocular or periorbital changes Perifollicular accentuation, lichenification, or prurigo lesions |
The Scoring Atopic Dermatitis index (http://scorad.corti.li) is the most widely used validated clinical tool to classify atopic dermatitis severity based on the affected body area and intensity of lesion characteristics.11 Other validated tools include the Eczema Area and Severity Index; the Investigator Global Assessment scale; and the Six Area, Six Sign Atopic Dermatitis severity score.
Complications
Infection is the most common complication of atopic dermatitis and is primarily due to the disruption of the epidermis and immune dysregulation caused by FLG gene mutations.6 Secondary bacterial infections are typically caused by Staphylococcus aureus and beta-hemolytic streptococcus. Protracted scratching can result in postinflammatory scar formation and lichenification.
Management
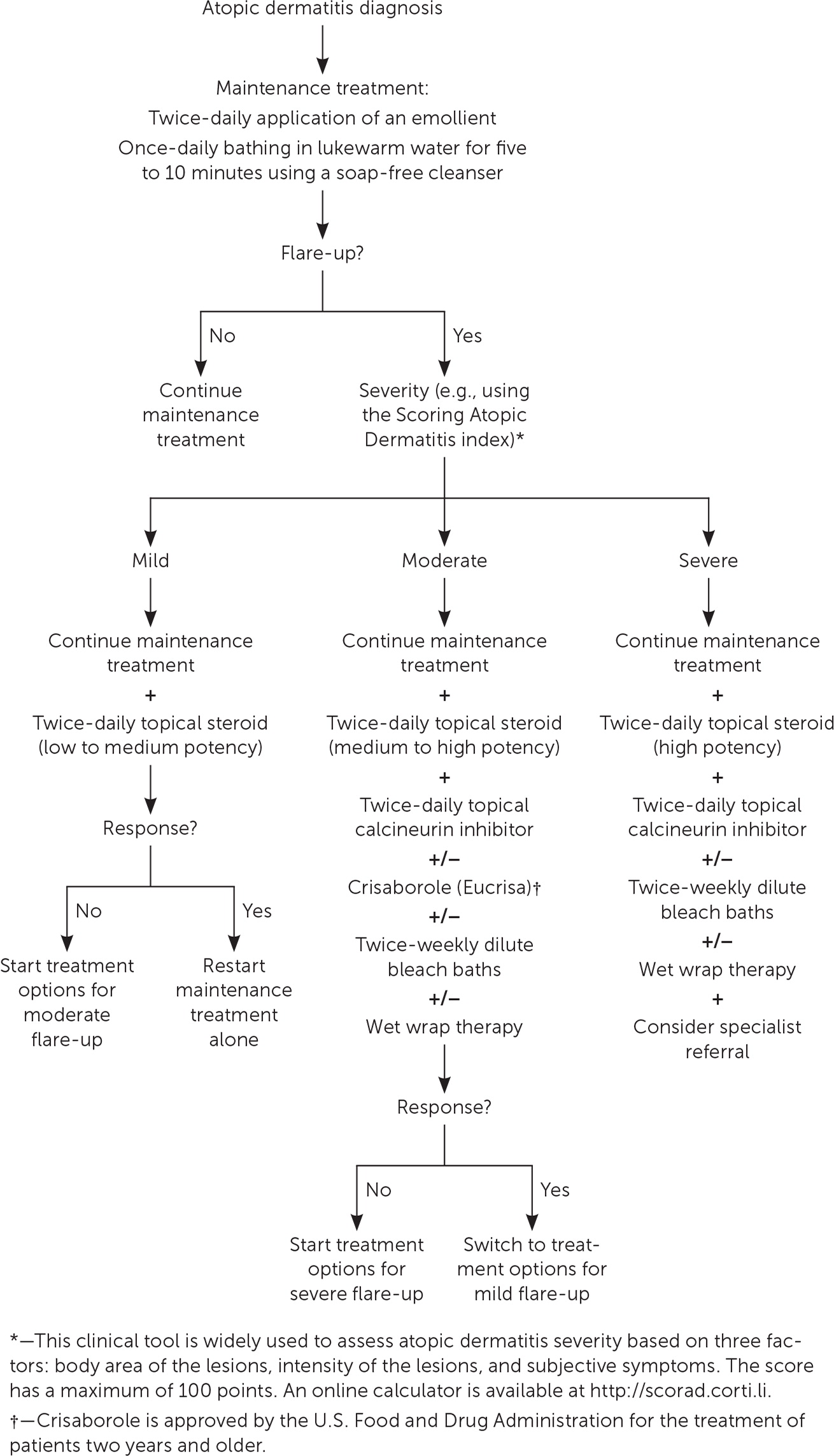
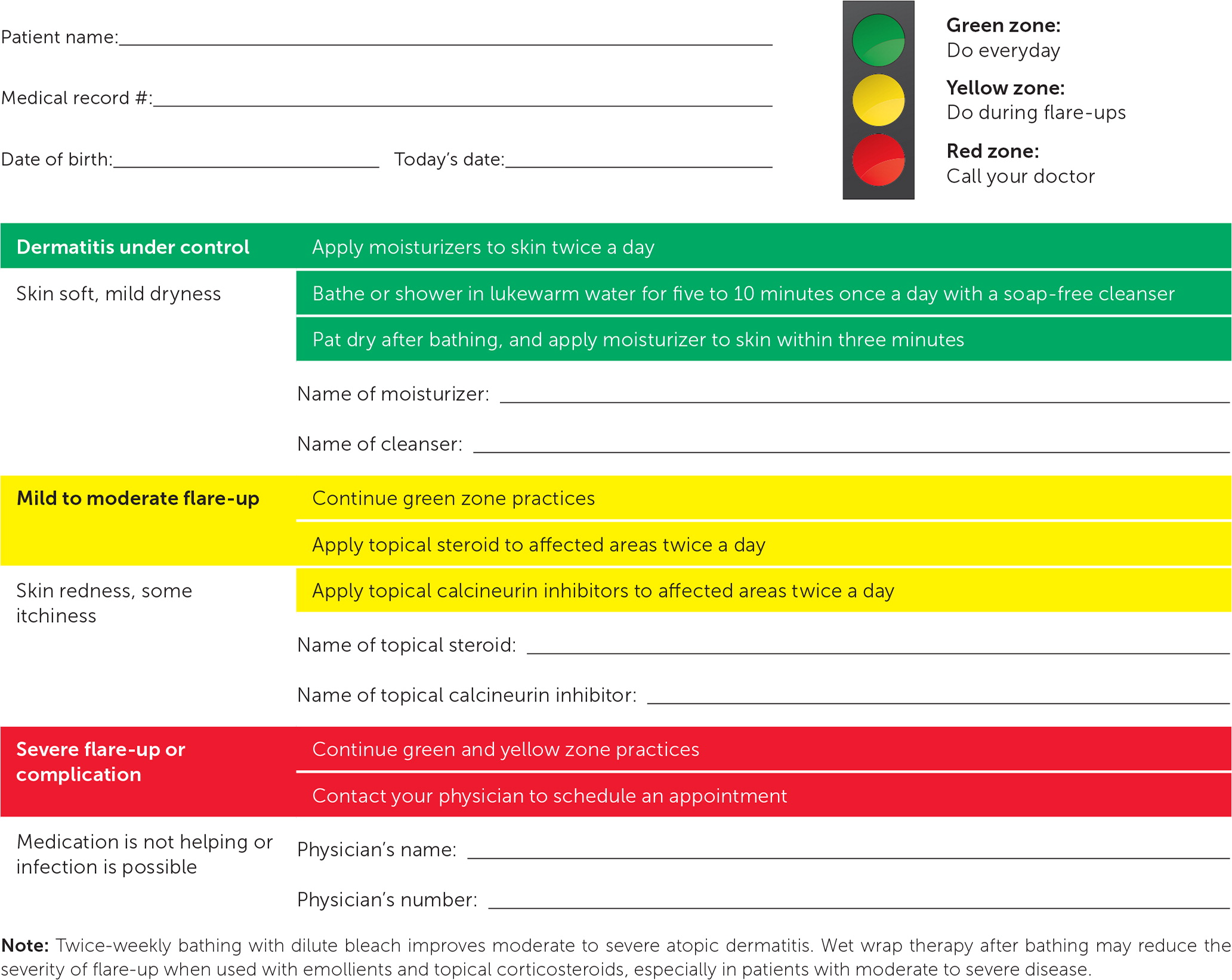
Figure 4 is an algorithm for the treatment of atopic dermatitis. Indications for specialist referral are listed in Table 3.12,13 Testing for food and environmental allergies is not recommended because of the high rate of false positives leading to unnecessary food avoidance.14 Using an atopic dermatitis action plan (Figure 5), which outlines specific treatments during the maintenance and flare-up phases, improves treatment adherence.15 Patient and family education on atopic dermatitis reduces disease severity and improves quality of life.16
| Candidates for allergen-specific immunotherapy* Consideration for systemic immunosuppressive therapy Poor disease control with appropriate first-line treatments Severe or recurrent skin infections (viral or bacterial) Significant psychosocial problems due to atopic dermatitis Uncertain diagnosis Uncontrolled facial atopic dermatitis |
EMOLLIENTS
Liberal application of fragrance-free emollients (moisturizers) is an essential part of daily prevention and treatment of atopic dermatitis regardless of disease severity.17 Emollients help retain and replenish epidermal moisture, decrease disease severity, and prolong the interval between flare-ups, and they should be used as the primary therapy for flare-ups and maintenance.18 Emollients also significantly decrease the need for prescription medications in the treatment of atopic dermatitis.19
Emollients with a high lipid (oil) content and low water content are recommended because of their effectiveness at retaining skin moisture. Ointments have the highest ratio of lipids, followed by creams and then lotions. Trials have not demonstrated a superior emollient among the dozens of over-the-counter and prescription options.19 Therefore, the choice of emollient should be based on individual patient preference. Research has not defined the optimal amount or frequency of use, but emollients should generally be applied once or twice daily.20 Several randomized controlled trials (RCTs) have demonstrated that emollients can be used as primary prevention in infants at risk of developing atopic dermatitis, specifically those with a first-degree relative who has atopy.21–23
Prescription emollient devices are a newer class of topical agents approved by the U.S. Food and Drug Administration (FDA) that replenish skin moisture by specifically targeting the skin barrier dysfunction.17 These agents have specific ratios of lipids to water that mimic the natural composition of the skin layers. There is no difference in effectiveness between over-the-counter emollients and prescription emollient devices.24
BATHING PRACTICES
Regular bathing helps hydrate and cleanse the skin by removing scales, crusts, bacteria, allergens, and irritants.25 In general, once-daily bathing with lukewarm water that is limited to five to 10 minutes is recommended.17,25 Patients should use soap-free, dye-free, fragrance-free, and hyporeactive cleansers; pat dry wet skin; and apply emollients within three minutes of bathing to help seal in moisture.
Twice-weekly bathing with dilute bleach improves moderate to severe atopic dermatitis because of bleach's antiseptic and antistaphylococcal properties.26 A common recipe for bleach baths is ½ cup of regular 6% bleach to 40 gallons of water. Wet wrap therapy after bathing may reduce the severity of flare-ups when used with emollients and topical corticosteroids, especially in patients with moderate to severe disease.27
TOPICAL CORTICOSTEROIDS
| Potency | Class | Corticosteroid | Preparation | Cost of generic* |
|---|---|---|---|---|
| Ultra high | I | Clobetasol 0.05% | Ointment, cream, lotion, gel, foam, solution | $50 for 60-g tube |
| High | II | Fluocinonide 0.05% | Ointment, cream, gel, solution | $40 for 60-g tube |
| Medium to high | III | Betamethasone valerate 0.1% | Ointment, cream, lotion, foam | $20 for 45-g tube |
| Medium | IV | Triamcinolone acetonide 0.1% | Ointment, cream, lotion | $10 for 30-g tube |
| Medium to low | V | Fluticasone propionate 0.005% | Ointment, cream, lotion | $20 for 60-g tube of cream |
| Low | VI | Desonide 0.05% | Ointment, cream, lotion | $55 for 60-g tube |
| Very low | VII | Hydrocortisone 2.5% | Ointment, cream, lotion | $10 for 28.4-g tube |
Topical steroids should be applied twice daily until the lesions are significantly improved or less thick. Duration of topical steroid therapy is guided by clinical improvement but is typically two weeks or less. To minimize adverse effects, the lowest possible potency topical steroid should be used for the shortest possible period to maintain good symptom control. Research suggests using a proactive approach to reducing flare-ups with once- or twice-weekly application of topical steroids to specific skin areas that have been repeatedly affected.30
Because of potential adverse effects, primarily skin atrophy, low-potency topical steroids are recommended when treating atopic dermatitis involving the face, neck, axillae, groin, and flexor surfaces. During severe flare-ups, use of mid- or higher-potency topical steroids for up to two weeks may be appropriate to attain rapid symptom control.31,32
There is no universal standard on quantifying the optimal amount of topical steroid that should be used with each application. Spreading an adult fingertip's worth of topical steroid across an area equal to two adult palms is recommended.17
Although topical steroids have a good safety profile overall, possible adverse effects include skin atrophy and discoloration, purpura, telangiectasia, striae, hypopigmentation, and acneiform eruptions.17 Many of these adverse effects resolve after topical steroid discontinuation, but it may take months. Topical steroid–induced suppression of the hypothalamic-pituitary-adrenal axis is uncommon with continuous mild or moderate topical steroid use. If there is a concern, a cortisol stimulation test can check for appropriate adrenal response.33
TOPICAL CALCINEURIN INHIBITORS
Topical calcineurin inhibitors are steroid-sparing immunomodulators used to treat atopic dermatitis in patients two years and older. Although traditionally used as second-line treatment for moderate to severe atopic dermatitis, they may be used as a first-line therapy in conjunction with topical steroids, especially in patients with steroid phobia (corticophobia), or facial or flexural lesions.30,34 Topical calcineurin inhibitors are recommended for short- or long-term use and for maintenance therapy. The two available topical calcineurin inhibitors are tacrolimus (Protopic) and pimecrolimus (Elidel). A meta-analysis of RCTs showed twice-weekly application of either medication increased the time between flare-ups and the total number of disease-free days.35
Pimecrolimus is recommended for mild to moderate atopic dermatitis, whereas tacrolimus is indicated for moderate to severe disease. Overall, tacrolimus is more effective than pimecrolimus, but both reduce inflammation and pruritus.36 A proactive maintenance approach of using tacrolimus twice weekly on areas prone to flare-ups reduces the rate of flare-ups and percentage of treatment days, and increases the time between flare-ups.37
Unlike topical steroids, topical calcineurin inhibitors do not cause skin atrophy and can be safely applied to areas with thinner skin, such as the face (including eyelids), neck, and groin. Localized reactions, including burning, stinging, and pruritus, are the most common adverse effects.38 Topical calcineurin inhibitors include an FDA boxed warning because of the possible association between the medications and malignancies, despite no firm evidence that there is a link.37
ULTRAVIOLET PHOTOTHERAPY AND SYSTEMIC IMMUNOMODULATORS
Narrow band ultraviolet B phototherapy is an effective second-line treatment for moderate to severe atopic dermatitis.28 Phototherapy reduces cutaneous inflammation with minimal adverse effects. Short courses of ultraviolet A phototherapy, alone and with oral psoralen, can be safely used to treat flare-ups.
Systemic immunomodulators, including cyclosporine (Sandimmune) and azathioprine (Imuran), are off-label options if standard therapy is ineffective. Systemic steroid use should be limited to severe flare-ups as short-term bridge therapy to other steroid-sparing options.28
ANTIBIOTICS
Patients with atopic dermatitis are susceptible to skin infections because of the disruption of the epidermis. Ninety percent of patients with atopic dermatitis are colonized with S. aureus, which increases their risk of cutaneous infections.26 An RCT evaluating intranasal mupirocin (Bactroban) combined with bleach baths showed an improvement in disease severity over three months.26 There is no high-quality evidence supporting prophylactic use of oral antibiotics. They should be used only to treat secondary bacterial infections.28,39,40
ANTIHISTAMINES
Oral antihistamines are not routinely recommended for atopic dermatitis, because there is no evidence that they reduce pruritus. Patients with severe sleep disturbance due to pruritus can be offered a short-term, intermittent course of an oral sedating antihistamine such as diphenhydramine (Benadryl) or hydroxyzine.17 Topical antihistamines are not recommended because of the risk of contact dermatitis.17
INTEGRATIVE MEDICINE THERAPIES
Evidence supporting popular over-the-counter supplements, including evening primrose oil, oral borage oil, probiotics, and St. John's wort, as effective treatments for atopic dermatitis is lacking.14
NEWER TREATMENT OPTIONS
Crisaborole (Eucrisa) is a topical, steroid-sparing phosphodiesterase-4 inhibitor that was FDA-approved in 2016 to treat mild to moderate atopic dermatitis in patients two years and older. A 2019 systematic review and meta-analysis showed that twice-daily application of crisaborole resolves lesions faster than topical controls.41 However, at $700 for a one-month supply (60-g tube), this medication is cost prohibitive for most patients.42
Dupilumab (Dupixent) is an injectable monoclonal antibody that was FDA-approved in 2017 to treat moderate to severe atopic dermatitis in patients 12 years and older who had an inadequate response or could not tolerate standard therapy.43 Dupilumab decreases inflammatory response and skin barrier impairment by blocking interleukin-4 and interleukin-13 expression.8 Two identical randomized, placebo-controlled, phase III studies showed that dupilumab improves lesion resolution, pruritus, sleep quality, and quality of life compared with placebo.44 However, a one-month supply of dupilumab costs $3,000.42
TREATMENT ADHERENCE
Poor adherence to treatment is a major factor affecting treatment outcomes in patients with atopic dermatitis. Poor adherence is associated with complex treatment regimens, financial burden, lack of knowledge, infrequent follow-up, and steroid phobia. Atopic dermatitis action plans, patient education, and frequent follow-up visits improve treatment adherence.45,46
This article updates previous articles on this topic by Berke, et al.12 ; Buys47 ; and Correale, et al.48
Data Sources: We searched PubMed using the key terms atopic dermatitis and eczema. We reviewed Essential Evidence Plus and the Cochrane database. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We reviewed the American Academy of Dermatology guidelines. Search dates: June to October 2019, and February 21, 2020.
