
Am Fam Physician. 2021;103(5):275-285
Author disclosure: No relevant financial affiliations.
Peripheral nerves in the upper extremities are at risk of injury and entrapment because of their superficial nature and length. Injury can result from trauma, anatomic abnormalities, systemic disease, and entrapment. The extent of the injury can range from mild neurapraxia, in which the nerve experiences mild ischemia caused by compression, to severe neurotmesis, in which the nerve has full-thickness damage and full recovery may not occur. Most nerve injuries seen by family physicians will involve neurapraxia, resulting from entrapment along the anatomic course of the nerve. In the upper extremity, the brachial plexus branches into five peripheral nerves, three of which are commonly entrapped at the shoulder, elbow, and wrist. Patients with nerve injury typically present with pain, weakness, and paresthesia. A detailed history and physical examination alone are often enough to identify the injury or entrapment; advanced diagnostic testing with magnetic resonance imaging, ultrasonography, or electrodiagnostic studies can help confirm the clinical diagnosis and is indicated if conservative management is ineffective. Initial treatment is conservative, with surgical options available for refractory injuries or entrapment caused by anatomic abnormality.
Peripheral nerves in the upper extremity are at risk for injury and entrapment. Their long course from the central nervous system through the extremity puts them at risk of compromise at narrow anatomic tunnels and areas of edema and trauma. The brachial plexus branches into five peripheral nerves, three of which are commonly entrapped at the shoulder, elbow, and wrist. Epidemiology data on entrapment neuropathies are sparse. Carpal tunnel syndrome is the most common with a prevalence of 3% in the general population (15% in the workforce).1 Cubital tunnel syndrome is also relatively common, with one U.S. metropolitan area reporting a prevalence of 1.8% to 5.9%.2 Overall prevalence of peripheral neuropathies in the general population is unclear.
Pathophysiology
Mechanisms of nerve injury can include direct pressure, stretch, overuse of a joint, or microtrauma. Prolongation of these injurious mechanisms causes fibrosis, resulting in a larger degree of injury.3–5 More specifically, nerve injury is divided into three grades of increasing severity: neurapraxia, axonotmesis, and neurotmesis. Neurapraxia is injury that damages the myelin sheath but not the axon. Complete recovery is possible in days to weeks. Axonotmesis extends damage to the axon but preserves the connective tissue framework. This can lead to subsequent degeneration distal to the lesion. Because of the slow rate of axonal regeneration, recovery can take years, with complete recovery often unachievable. Neurotmesis is the total or partial disruption of the entire nerve fiber, including the connective tissue framework. Full clinical recovery is usually not achieved.6,7 How long compression must be present to cause permanent loss of conduction or fibrosis is not well defined in the literature.
History and General Examination
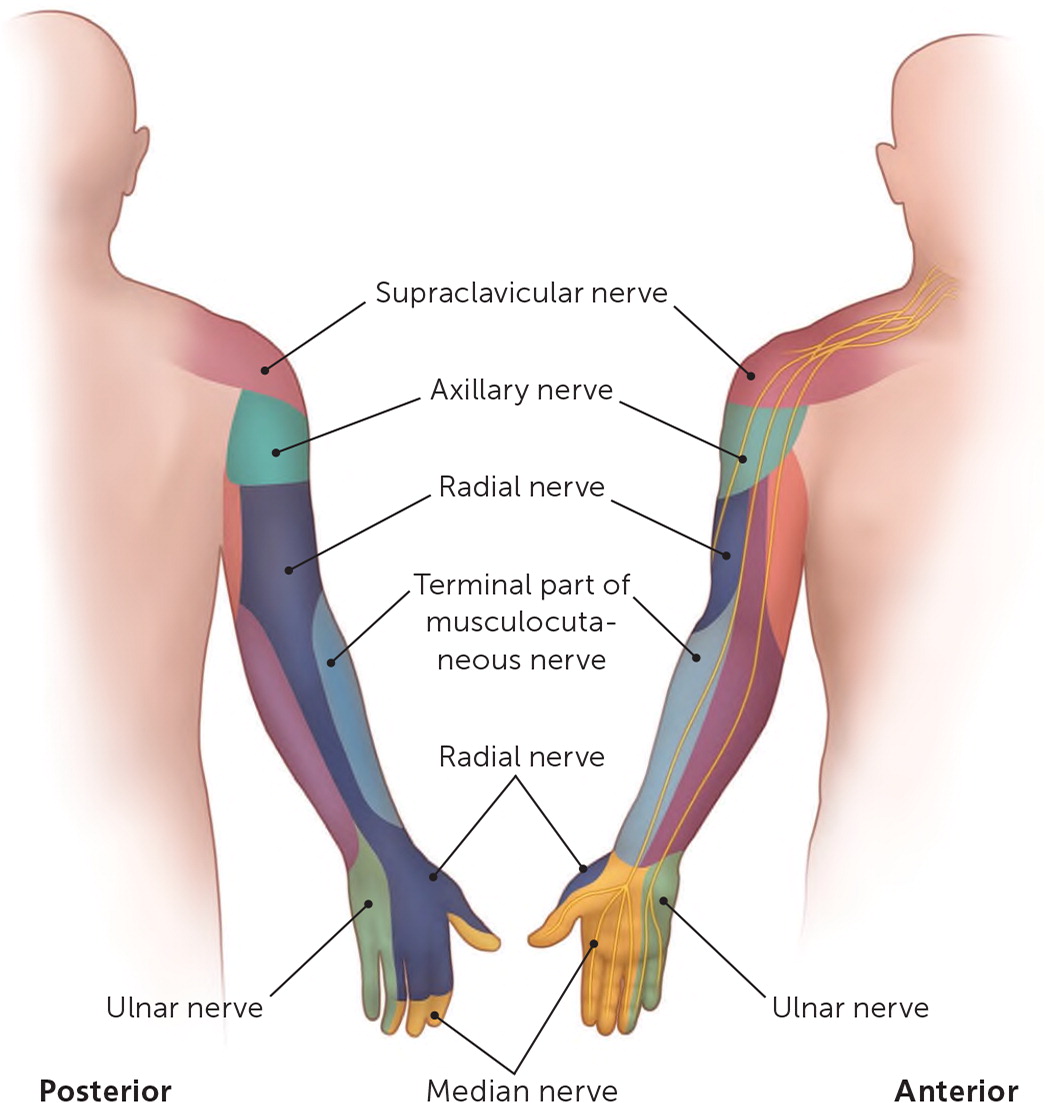
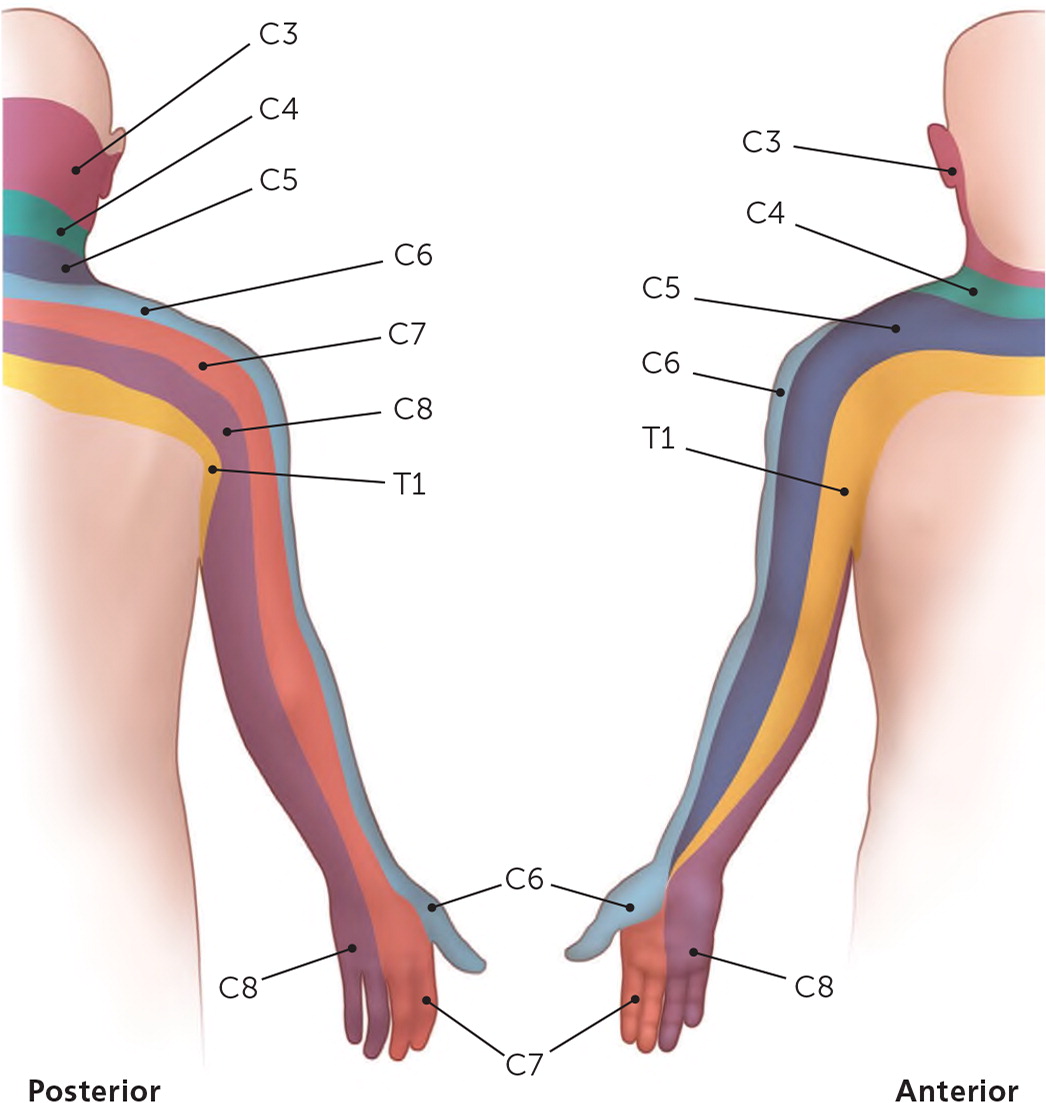
Nerve entrapment should be suspected when limb weakness, pain, or paresthesia is present and not caused by another etiology, such as systemic disease or muscle injury. History should focus on known trauma, time course, aggravating activities, and distribution of symptoms. In the absence of significant trauma, evaluation of range of motion and muscle strength is needed, and inspection, palpation, and neurologic testing of the area should be performed with assessment of the cervical spine.8 Knowledge of myotomes and dermatomes helps localize the specific nerve injured9–11 (Table 1,10,11 Figure 1,12 and Figure 212).
| Joint function | Cervical root | Muscles | Nerves |
|---|---|---|---|
| Shoulder abduction | C5 | Deltoid | Axillary |
| Elbow flexion | C5, C6 | Biceps | Musculocutaneous |
| Elbow extension | C7 | Triceps | Radial |
| Forearm pronation | C6, C7 | Pronator teres | Median |
| Forearm supination | C6 | Supinator | Radial |
| Wrist flexion | C7 | Flexor carpi radialis, flexor carpi ulnaris | Median and ulnar |
| Wrist extension | C6, C7 | Extensor carpi radialis brevis, extensor carpi radialis longus | Radial |
| Finger flexion | C8 | Flexor digitorum profundus, flexor digitorum superficialis | Ulnar and median |
| Finger extension | C7, C8 | Extensor digitorum, extensor indicis, extensor digiti minimi | Radial (posterior interosseous) |
| Thumb abduction | C7, C8 | Abductor pollicis longus | Radial (posterior interosseous) |
| Thumb flexion | C8, T1 | Flexor pollicis longus | Median (anterior interosseous) |
| Finger abduction or adduction | T1 | Intrinsic hand muscles | Ulnar |
Common Nerve Injuries and Entrapment Syndromes of the Upper Extremity
| Nerve | Characteristics | Sensory deficits | Motor deficits | Conservative therapy | Surgical indications |
|---|---|---|---|---|---|
| Axillary nerve | Lateral shoulder region paresthesia, shoulder movement weakness in all planes, difficulty with overhead activities | Lateral shoulder | Deltoid, teres minor | Physical therapy, monitoring recovery with serial examination vs. electromyography and nerve conduction studies | No electrophysiologic improvement after 3 to 4 months of conservative treatment |
| Long thoracic nerve | Scapular winging | None | Serratus anterior | Physical therapy, avoidance of aggravating activities | Penetrating trauma resulting in nerve transection, no improvement after 18 to 24 months of conservative treatment |
| Median nerve at the elbow or forearm anterior interosseous nerve branch | No pain; thumb weakness; unable to make OK sign; if patient is unable to make OK sign but has sensory deficits, consider a proximal median nerve injury | None | Flexor pollicis longus, flexor digitorum profundus | Rest, splinting, and observation | Space-occupying lesion, no improvement after 3 to 4 months of conservative treatment |
| Median nerve at the elbow (pronator syndrome) | Aching pain in the proximal volar forearm; palm, thumb, or index finger paresthesia | Thumb, index and middle fingers, and radial side of ring finger | Varied but may include weakened grip strength | Avoidance of aggravating activities, rest, trial of NSAIDs, steroid injection | Space-occupying lesion, no improvement after 3 to 4 months of conservative treatment |
| Median nerve at the wrist (carpal tunnel syndrome) | Pain in the wrist and hand, occasionally radiating to the forearm; paresthesia in the first three digits; weak grip strength due to weakness of thumb abduction and opposition resulting in difficulty with tasks such as opening doors; thenar eminence atrophy in advanced disease | Thumb, index and middle fingers, and radial side of ring finger | Abductor pollicis brevis, first or second lumbrical | Splinting, physical therapy, yoga, and acupuncture for the short term Cochrane review: nocturnal splinting more effective than placebo13 Maximal benefit of conservative treatment typically achieved around 3 months Steroid injection Cochrane review: symptomatic improvement for up to one month with steroid injection; more recent studies show up to 10 weeks of improvement and delay of surgery for up to 1 year14 | Early surgery: evidence of moderate to severe median nerve damage on electromyography Significant weakness of grip strength; thenar eminence atrophy; no improvement after 3 to 4 months of conservative treatment Cochrane review: surgical decompression is better at long-term symptom management than splinting alone; unclear if surgery is better than steroid injection, especially in those with mild symptoms15 Cochrane review: endoscopic and open techniques are equally effective; however, endoscopic recovery is shorter by 8 days16 |
| Radial nerve at the elbow (posterior interosseous nerve) | Weakness in finger extension, weakness of ulnar deviation, wrist extension can be maintained (because of sparing of extensor carpi radialis longus), pain is rare | None | Extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, extensor indicis, supinator | Rest, activity modification, splinting, stretching, NSAIDs; steroid injection can be therapeutic and diagnostic | Significant motor weakness is present, no improvement after 3 to 4 months of conservative treatment |
| Radial nerve at the elbow (superficial radial nerve) | Pain 3 cm to 4 cm distal to lateral epicondyle, often causes pain at night | Lateral forearm | None | Rest, activity modification, splinting, stretching, NSAIDs; steroid injection can be therapeutic and diagnostic | Surgery rarely required |
| Radial nerve at the spiral groove (radial neuropathy [Saturday night palsy]) | Weakness in finger and wrist extension, paresthesia of forearm and hand | Posterior forearm and dorsal hand | Brachioradialis (elbow flexion); extensor carpi radialis longus; branches distally include superficial radial nerve and posterior interosseous nerve, which can also be affected | Avoidance of repeat compression, physical therapy nearly 100% effective at 6 months based on small observational study, cock-up splint for normal hand function | Fracture of the humerus resulting in nerve compromise |
| Radial nerve at the wrist (handcuff neuropathy) | Pain and paresthesia of the hand; if motor findings are present, consider a higher radial nerve lesion | Dorsal radial hand | None | Eliminate external compression, steroid injection | Surgery rarely required, no improvement after 3 to 4 months of conservative treatment |
| Spinal accessory nerve | Weakness in shoulder abduction (> 180 degrees), scapular winging | None | Trapezius (shoulder shrug) and sternocleidomastoid | Physical therapy, avoidance of aggravating activities | Penetrating trauma resulting in nerve transection, no improvement after 18 to 24 months of conservative treatment |
| Various nerves at brachial plexus level | Transient paresthesia and weakness from neck or shoulder traveling down the arm | Varied based on affected nerves | Varied based on affected nerves | Rest, physical therapy, pain control | Evidence of anatomic abnormalities (foraminal stenosis) predisposing to repeat injury |
| Suprascapular nerve | Weakness in shoulder flexion, abduction, external rotation | Sensory to shoulder joint | Supraspinatus (shoulder abduction) and infraspinatus (external rotation of the shoulder) | Physical therapy to maintain range of motion, activity modification to limit overhead activities | Early surgery for space-occupying lesion (i.e., ganglion cyst) Systematic review of 21 studies (275 athletes) showed lower patient-reported pain as tracked by visual analog scale and a return to sport of 92% of athletes17 |
| Ulnar nerve at the elbow (cubital tunnel syndrome) | Pain, paresthesia, numbness in the fourth and fifth digits; weakness in finger abduction, thumb abduction, and thumb-index pincer; positive Tinel sign at the cubital tunnel; weak wrist flexion not due to the median nerve innervation of flexor carpi radialis and flexor digitorum superficialis, which compensate for loss of flexor carpi ulnaris | Hypothenar eminence, fifth finger, and ulnar side of fourth finger | Intrinsic hand muscles, flexor carpi ulnaris | Activity modification, NSAIDs, elbow pads, physical therapy, night splinting in 45 degrees of extension with neutral forearm, steroid injection | No improvement after 3 to 4 months of conservative treatment Most common procedures are surgical decompression or nerve transposition; in one Cochrane review they were equally effective18 |
| Ulnar nerve at the wrist (cyclist's palsy) | Atrophy of intrinsic hand muscles (hypothenar, lumbrical, interosseous); pain, paresthesia, numbness of the hand; positive Froment sign (Figure 6; https://www.youtube.com/watch?v=WnTVWnTFymA) | Hypothenar eminence, fifth finger, and ulnar side of fourth finger | Intrinsic hand muscles (grip strength) | Patient education, activity modification, padding on handlebars, splinting, physical therapy, and NSAIDs; steroid injection not indicated because causes are usually related to structural or mechanical abnormality; drain ganglion cyst if this is the cause | Management of anatomic cause (e.g., ganglion cyst, lipoma, hook of hamate fracture), no improvement after 2 to 4 months of conservative treatment Postsurgical splinting and rehabilitation recommended Typical return to work in 6 to 8 weeks |
SHOULDER AND ARM
Brachial Plexus. Brachial plexus injury is commonly associated with contact sports. Known as a stinger, this injury causes transient paresthesia and weakness radiating from the neck in the distribution of the injured nerve root. Proposed mechanisms are traction, compression, or direct trauma to the brachial plexus or cervical nerve root (e.g., leading with the shoulder during a tackle in football).20 The most common distribution is the C5 and C6 myotomes and dermatomes. Following a first episode, return to play is acceptable when there is complete resolution of symptoms and cervical spine injury has been excluded.32,39 Persistent or recurrent stingers prompt additional evaluation for cervical stenosis or other bony abnormalities.32
Axillary Nerve. The axillary nerve is vulnerable as it passes around the humerus and through the quadrilateral space of the posterior shoulder. Shoulder dislocations, repetitive use injuries, humeral neck fractures, and local pressure (e.g., from crutches) are mechanisms of injury.19 Damage to the axillary nerve results in paresthesia or pain of the lateral shoulder and weakness in shoulder external rotation, extension, abduction, and forward flexion.
Long Thoracic Nerve. The long thoracic nerve is vulnerable to traction injury at its nerve roots located at the middle scalene.20 Other mechanisms of injury include direct blows to the nerve as it exits the pectoralis muscle at the fourth or fifth rib, repetitive stretching (e.g., throwing a baseball, serving a volleyball), or iatrogenic damage (e.g., during a radical mastectomy).20,21 Injury to this nerve is the most common cause of scapular winging.20,21
Spinal Accessory Nerve. The spinal accessory nerve is vulnerable to injury in the posterior triangle of the neck from direct trauma or iatrogenic damage. Findings on examination include scapular winging and weakness in shoulder shrugging and shoulder abduction past 180 degrees.21 Chronic injury may result in trapezius atrophy.
Suprascapular Nerve. The suprascapular nerve is vulnerable at several locations. The first is posterior to the clavicle, occurring with clavicular fractures. It is susceptible to stretching injuries related to overhead activities at the suprascapular and spinoglenoid notches.33 It can also be entrapped by glenoid labral cysts that extend from the capsule with labral injury.33 Symptoms of suprascapular nerve entrapment include shoulder pain and shoulder abduction and forward flexion weakness. Rotator cuff injury can present similarly; therefore, magnetic resonance imaging, ultrasonography, or electrodiagnostic studies are usually appropriate to determine the specific etiology if initial radiography is inconclusive.18,33
Radial Nerve. The radial nerve is vulnerable to injury and entrapment at several locations. Proximally, middle to distal third humeral shaft fractures are the most common cause of traumatic injury.40 The most common compressive cause results from sustained pressure on the posterior arm at the location of the radial groove, where the nerve lies directly on periosteum and is not protected by muscle. This is known as radial neuropathy, or sometimes Saturday night palsy.17 Compression also occurs at the axilla, as it passes through the triceps brachii lateral head.41 The nerve innervates the extensors of the wrist and fingers, causing wrist and finger drop. Sensory deficit usually affects the posterior forearm and dorsal hand.17
FOREARM AND ELBOW
Median Nerve. Proximal median nerve entrapment is rare. The primary clinical finding is pain in the proximal volar forearm. Other findings may include cramping, decreased grip strength, or paresthesia in the first three digits.22
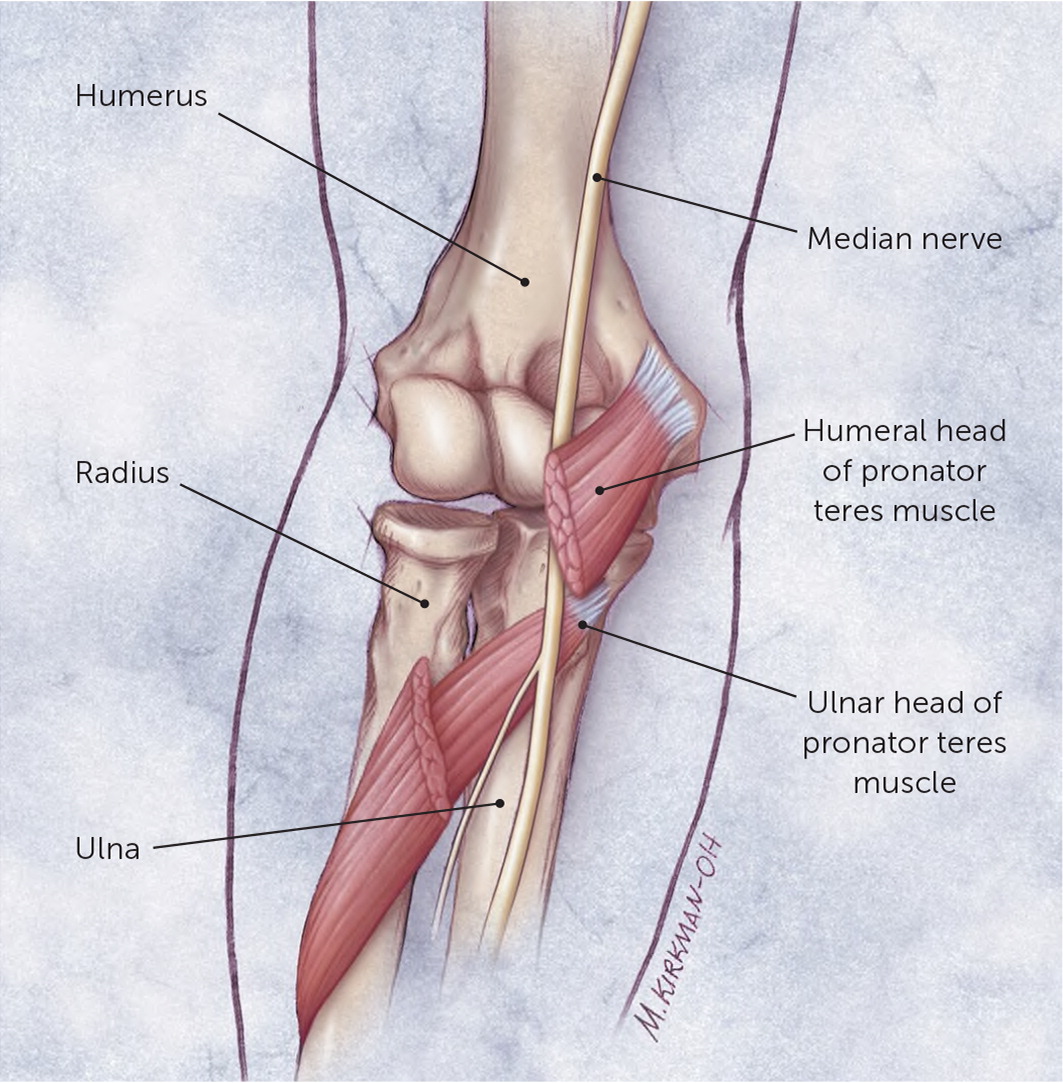
Pronator and anterior interosseous nerve syndromes are the two most common compression neuropathies of the median nerve occurring around the elbow.22 Pronator syndrome occurs with compression of the median nerve between the two heads of the pronator teres (Figure 3)42 or under the proximal edge of the flexor digitorum superficialis (see a video about pronator syndrome). It develops insidiously over months to years, often exacerbated by activities with the arm in pronation, such as repetitive hammering or a backhand swing with a tennis racket. The pronator syndrome test is performed by resisting the patient's pronation starting with the elbow in neutral and moving into extension (see a video demonstrating the pronator syndrome test). When positive, it will induce paresthesia and pain.22
The anterior interosseous nerve is the motor-only nerve for deep muscles of the forearm. The most common examination finding in anterior interosseous nerve syndrome is weakness in the flexor pollicis longus and flexor digitorum profundus, resulting in the inability to make an OK sign. Subtle weakness can be detected by attempting to break apart the thumb and second digit while the patient makes an OK sign22 (see a video about the anterior interosseous nerve).
Radial Nerve. At the elbow, the radial nerve divides into a superficial branch (sensory only) and a deep branch (posterior interosseous nerve [motor only]; Figure 4).42 Entrapment of the superficial radial nerve causes pain 3 cm to 4 cm distal to the lateral epicondyle along the proximal lateral forearm with activity or during sleep. Pain is exacerbated by extending the elbow, pronating the forearm, and flexing the wrist.30
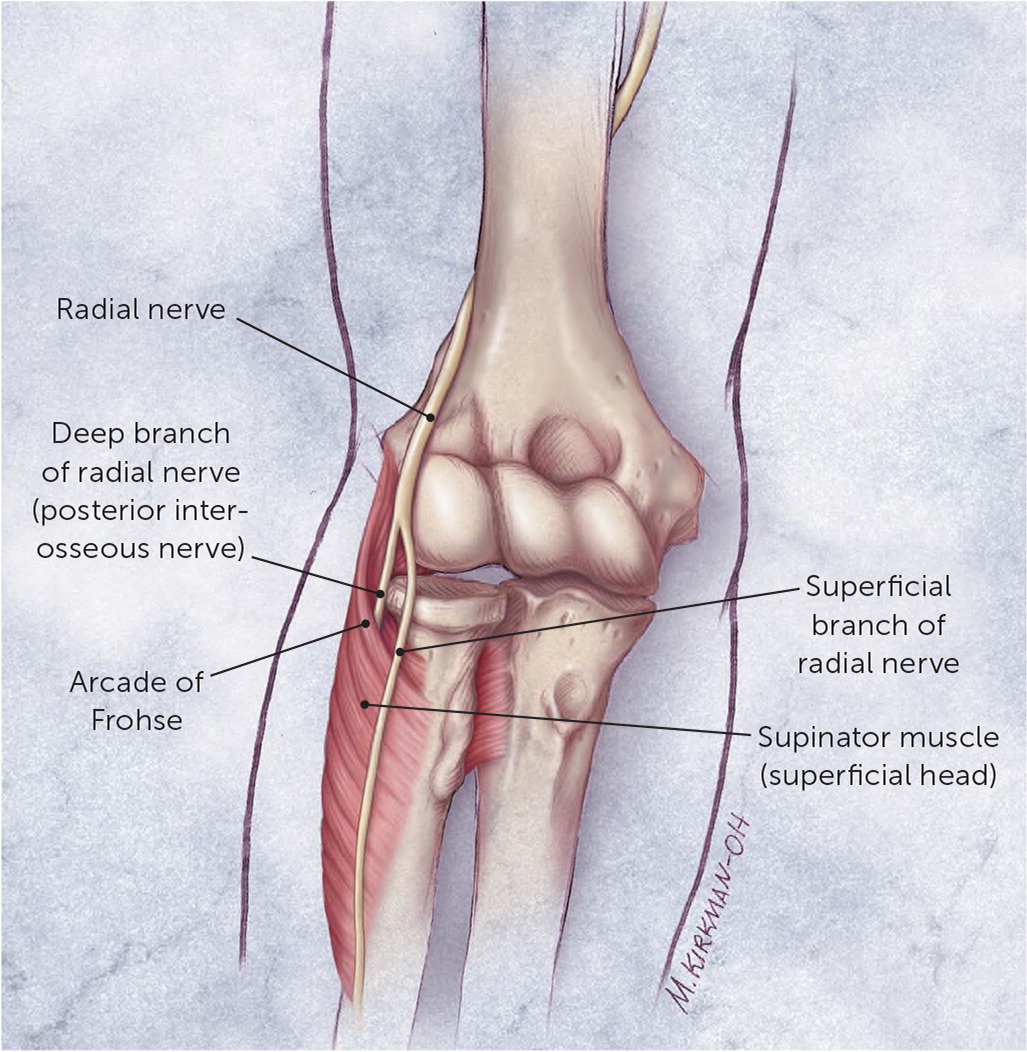
Posterior interosseous nerve syndrome results in motor-only weakness. Examination findings include loss of finger extension (finger drop) but preserved wrist extension with radial deviation of the wrist. This is caused by compensatory actions of the extensor carpi radialis longus, which is not innervated by the posterior interosseous nerve.30 These findings are usually from compression by space-occupying lesions (most commonly lipoma) or synovitis of the elbow.30
Additionally, a lesion proximal to the split, known as radial tunnel syndrome, may have both the motor and sensory symptoms described above.
Ulnar Nerve. At the elbow, the ulnar nerve passes posteriorly and superficially to the medial epicondyle within the cubital tunnel, leaving it susceptible to compression from external and internal sources. Symptoms include pain and paresthesia in the ulnar nerve dermatome, especially in the fourth and fifth digits of the hand.17,18,35 This is exacerbated by repetitive elbow flexion, which compresses the area of the cubital tunnel. Patients may have point tenderness over the ulnar nerve and a positive Tinel sign.35 Late findings are motor weakness of finger and thumb abduction.35
HAND AND WRIST
Median Nerve. At the wrist, the median nerve travels under the transverse carpal ligament (i.e., carpal tunnel syndrome), which has been reviewed previously in American Family Physician.1 Symptoms include pain in the wrist and hand, numbness and tingling in the first three digits, and weak grip strength. Atrophy of the thenar muscles occurs with prolonged injury.36 The Tinel sign and Phalen test are often used in the evaluation of carpal tunnel syndrome but have a wide range of sensitivity (38% to 100% and 42% to 85%, respectively) and specificity (54% to 98% and 55% to 100%, respectively).23,24 Electrodiagnostic testing is used to increase the diagnostic likelihood of carpal tunnel syndrome and should be performed if surgery is being considered.26,43
Radial Nerve. At the wrist, the superficial radial nerve is susceptible to injury by compression because it runs superficially to the flexor retinaculum. This has been termed handcuff neuropathy because of the potential for injury by circumferential pressure on the wrist. The superficial radial nerve has no motor component but provides sensation to the dorsal aspect of the hand and wrist.40
Ulnar Nerve. The ulnar nerve can become entrapped at the wrist in the Guyon canal, which is a fibro-osseous tunnel bordered by the hook of hamate and the pisiform (Figure 5).44 Occupational causes include activities that put pressure on the volar surface of the wrist, such as operating a jackhammer, cycling (i.e., cyclist's palsy), or weight-lifting. Other causes include fractures, lipomas, ganglion cysts, and systemic diseases (e.g., diabetes mellitus, rheumatoid arthritis, hypothyroidism) that cause localized edema.38,45
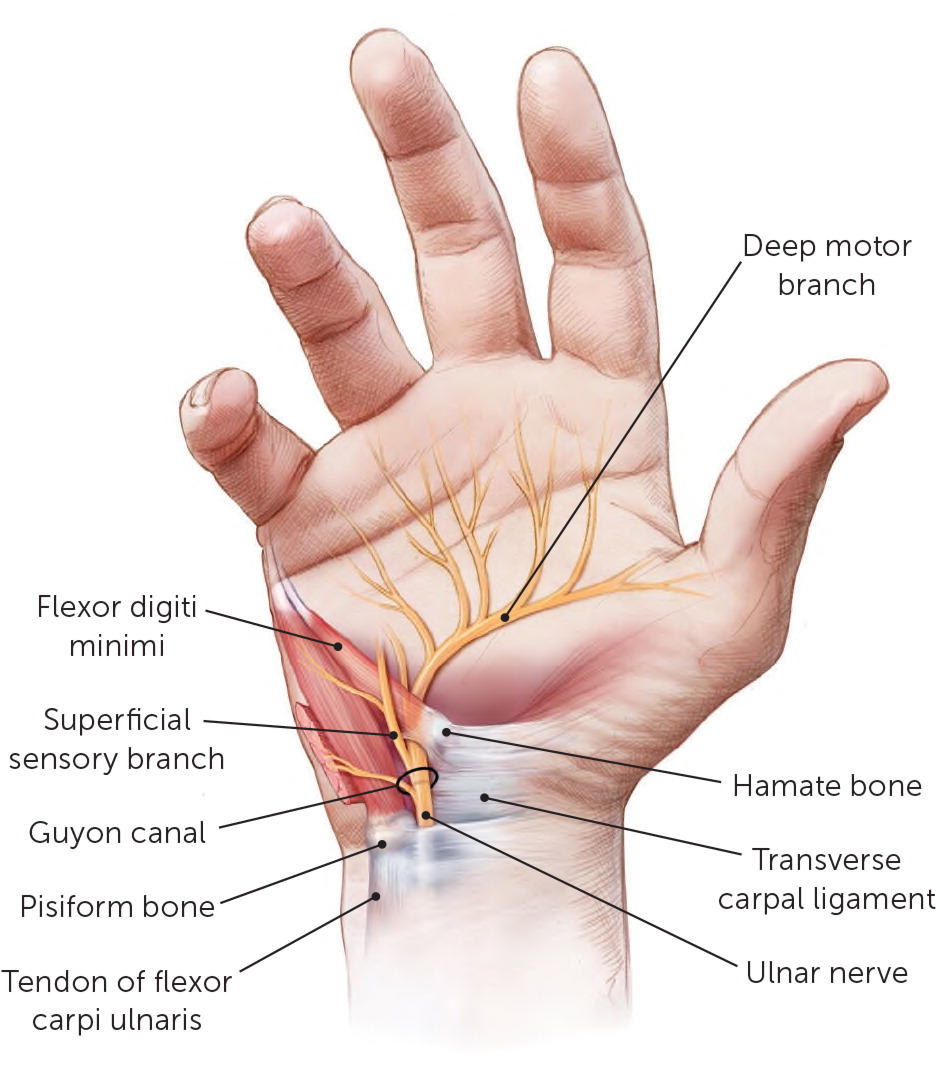
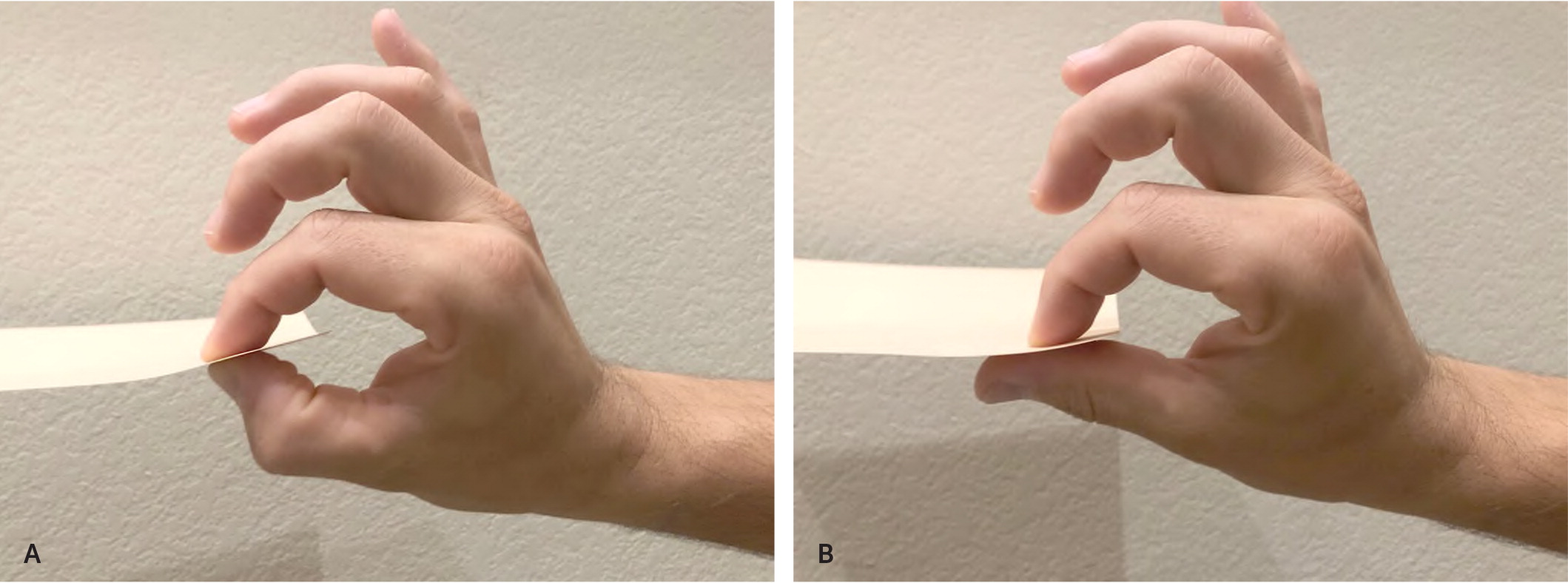
Findings of ulnar nerve entrapment include atrophy of the hypothenar, lumbrical, and interosseous muscles.38 Motor dysfunction is less common because of the deep nature of the motor branch, but it results in weakness of abduction and adduction of the fingers as well as the pincer mechanism.46 The Froment sign (Figure 6) can be observed with ulnar nerve entrapment at any anatomic location, but it is more common when injury occurs to the deep branch at the wrist.38,46 Sensory disturbances occur over the hypothenar eminence, the fifth digit, and half of the fourth digit.38
Diagnostic Testing
The primary diagnostic tests for evaluation of nerve injury and entrapment include electrodiagnostic tests, subdivided into nerve conduction studies and electromyography (EMG), and imaging, which includes magnetic resonance imaging and ultrasonography. With findings of severe weakness or multiple nerve involvement, imaging should be performed immediately; otherwise, it can be initiated after six to eight weeks of conservative treatment.47–50 A summary of imaging indications is provided in Table 3.47–49
| Imaging | General use and technique | Median nerve assessment | Radial nerve assessment | Ulnar nerve assessment |
|---|---|---|---|---|
| Magnetic resonance imaging | Fat-suppressed highly T2-weighted images demonstrate nerve pathology the best Low slice thickness: 2 mm to 3 mm in distal extremity and 4 mm to 5 mm in proximal extremity Identify anatomic abnormalities such as ganglion cysts or bony abnormalities Rule out other causes by identifying abnormalities of surrounding soft tissues Evaluate for muscle denervation Evaluate for nerve tumors | Carpal tunnel syndrome: evaluate persistent nerve distress and/or inadequate surgical release | Posterior interosseous nerve: thickened superficial head of supinator (most common entrapment point of posterior interosseous nerve), denervation of the supinator muscle Superficial radial nerve: imaging of choice for evaluation of surrounding muscle | Cubital tunnel syndrome: perform with extended elbow, shows nerve enlargement, external compression by loose bodies or space-occupying lesions, and regional inflammatory and denervation changes Guyon canal: useful for persistent symptoms with normal electromyography or tumor noted on ultrasonography |
| Ultrasonography | Use high-resolution (15 to 18 MHz) transducers Identify causes of entrapment such as fibrous bands, ganglion cysts, anomalous muscles, and bony abnormalities Evaluate for changes in nerve thickness (by cross-sectional area) and fascicular appearance Assessment of nerve and surrounding tissue vascularization Easy comparison to contralateral arm Dynamic testing | Carpal tunnel syndrome: assess nerve thickness within the carpal tunnel and pronator quadratus for a change greater than 2 mm | Posterior interosseous nerve: superficial nerve is easy to visualize, enlargement and hypoechogenicity of the nerve can be seen | Cubital tunnel syndrome: nerve appears enlarged and hypoechoic, loss of normal fibrillar appearance; comparison of cross section to contralateral side, shows dynamic snapping of nerve Guyon canal: shows thickened and hypoechoic nerve and ganglion cyst or accessory muscle |
Electrodiagnostic testing is helpful to confirm the diagnosis, determine severity, and monitor progression of nerve damage.50 This can be especially helpful in presurgical planning for more common nerve entrapments, such as carpal tunnel syndrome and cubital tunnel syndrome.51,52 Nerve conduction studies evaluate the speed and time of conduction across the nerve; EMG measures the tested muscle's response to stimulation.50 Changes to both nerve conduction studies and EMG will occur depending on the chronicity and degree of injury, so they should be ordered simultaneously.50–52 The ability of EMG or nerve conduction studies to detect nerve injury is variable and requires subjective interpretation; they are best used as an adjunct to physical examination and imaging.50
Magnetic resonance imaging and ultrasonography are used for evaluating deeper soft tissue pathology and bony abnormality compressing a nerve or for increased signal and nerve thickness indicative of nerve injury.40,53 Magnetic resonance imaging can identify local muscular atrophy consistent with denervation.53 Ultrasonography can evaluate for a variety of changes that occur in peripheral nerve entrapment syndromes.47,48 A useful point-of-care application of ultrasonography is determining specific sites of entrapment by compression with the ultrasonography transducer to recreate symptoms.47,48 Specifically, ultrasonography is helpful in the diagnosis of carpal tunnel syndrome; one meta-analysis found that a cross-sectional area of the median nerve at the carpal tunnel inlet of 9 mm2 or more is 87.3% sensitive and 83.3% specific for carpal tunnel syndrome.49 Accurate interpretation is dependent on sonographer experience, and correlation to EMG has yet to be shown.49
Treatment
In the absence of traumatic injury, initial treatment of nerve injuries should be conservative and includes patient education, relative rest, and activity modification.13–22,29–31,33–35,37,38 Physical therapy, yoga, and acupuncture may be helpful, although conclusive evidence is lacking.13–22,29–31,33–35,37,38 Surgical options include nerve decompression, exploration for anatomic causes and treatment, or nerve transfers.54,55 Despite low complication rates, these procedures are often associated with lack of full resolution of symptoms, even when patients complete a rehabilitation program.54,55 Carpal tunnel syndrome is one of the few entrapment neuropathies to have evidence-based treatment.13–16,24–28 Conservative treatment options and surgical indications for each of the nerves are listed in Table 2.13–38
This article updates a previous article on this topic by Neal and Fields.12
Data Sources: PubMed, Essential Evidence Plus, the Cochrane database, and the Agency for Healthcare Research and Quality were searched using key terms peripheral nerve entrapment, peripheral nerve injury, radial nerve, median nerve, ulnar nerve, and treatment of peripheral nerve injury/entrapment. Search dates: September/October 2019; February 26, 2020; May 2, 2020; August 2020; and January 2, 2021.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as the official policy or position of the U.S. Air Force, the Department of Defense, or the U.S. government.
